Documente Academic
Documente Profesional
Documente Cultură
Trau Ocl
Încărcat de
Luis KabreraDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Trau Ocl
Încărcat de
Luis KabreraDrepturi de autor:
Formate disponibile
Volume 4 Number 1 December 1999
Occlusal Trauma: Effect and Impact on the Periodontium
William W. Hallmon*
* Baylor College of Dentistry, Dallas, Texas.
This focused review is limited to a number of investigations in an attempt to specically address the histological and clinical effects of excessive occlusal forces on the teeth and periodontium and to provide a basis of classication for this interaction. This review does not include the effects of occlusal forces on dental implants or dental prostheses/appliances. Ann Periodontol 1999;4:102-107. KEY WORDS Occlusion, histology; occlusion, trauma.
or many years the role of occlusion and its dynamic interactive impact on the periodontium has been an issue of controversy and extensive debate.1-37 Although a variety of occlusal conditions have purportedly been related to this interaction (e.g., bruxism, malocclusion, abfraction, etc.), the central focus has been on occlusal trauma (primary and secondary) resulting from excessive force(s) applied to the periodontium. Occlusal trauma is dened as an injury of the attachment apparatus or tooth as a result of excessive occlusal forces.38 In an attempt to clarify and better understand this condition, early investigators used human necropsy specimens7,12,15,19,39 and a variety of animal models as a basis for clinical and histological studies.3-6,8-11,14,20-37 Findings were often diverse and somewhat contradictory. In the animal studies, factors of concern included differences among animals, forces applied, and lack of controls.16 Retrospective descriptive observations of the effect of excessive forces on the periodontium were derived from human necropsy materials.7,12,15,19,39 The selection of study sites was based on occlusal wear, patterns of pocket formation, and the presence of attachment loss, leaving some question as to the presence of ongoing occlusal trauma.40,41 Despite the foregoing concerns, the majority of these early studies agreed that occlusal trauma, in and of itself, failed to result in pocket formation or loss of connective tissue attachment.16,40 It is apparent that
102
Ann Periodontol
Hallmon
our understanding of the effects of excessive occlusal force and the destructive, adaptive, and reparative response of the periodontium has been complicated by a relative lack of evidence based on well-controlled prospective studies in human beings.40-42 This focused review is limited to a number of investigations in an attempt to specically address the histological and clinical effects of abnormal occlusal forces on the teeth and periodontium and to provide a basis of classication for this interaction. This review does not include the effects of occlusal forces on dental implants or dental prostheses/appliances. SIGNIFICANCE OF OCCLUSAL TRAUMA TO INFLAMMATORY PERIODONTAL DISEASE Denitions To facilitate orientation and understanding of this topic, the following denitions will apply to the review and discussion of the relationship between excessive occlusal forces and the periodontium. Occlusal trauma refers to a response or effect and is dened as an injury to the attachment or tooth as a result of excessive occlusal forces.38 Primary occlusal trauma is injury resulting from excessive occlusal forces applied to a tooth or teeth with normal support, while secondary occlusal trauma is injury resulting from normal occlusal forces applied to a tooth or teeth with inadequate periodontal support.38 Combined occlusal trauma refers to injury resulting from abnormal occlusal forces applied to a tooth or teeth with inadequate (abnormal) periodontal support.43 Traumatogenic occlusion refers to a cause and is dened as any occlusion that produces forces that cause an injury to the attachment apparatus.38 Primary, secondary, and combined occlusal trauma were originally described in the periodontal literature in 192844 and serve as a basis of discussion of the sequellae of occlusal trauma.45,46 Despite continued acceptance and diagnostic use of these dened conditions,38 this reviewer was unable to nd specic support for these terms based on evidence derived from controlled studies. In an in vitro stress model study using nite element analysis to calculate periodontal ligament stresses in primary and secondary occlusal trauma, stress values increased as bone support decreased.47 This was especially notable after reducing the supporting bone 4 mm or more.47 Histological Studies The histologic features of occlusal trauma have been studied extensively in animals and human autopsy materials.7,11,12,19,21,22,39,48,49 Alterations of the periodontium that have been associated with occlusal trauma will vary with the magnitude and direction of applied force, and location (pressure versus tension). These changes may include widening/compression of
the periodontal ligament, bone remodeling (resorption/ repair), hyalinization-necrosis, increased cellularity, vascular dilatation/permeability, thrombosis, root resorption, and cemental tears.2,11,12,39,48,50-53 Collectively, these changes have been interpreted as an attempt by the periodontium to adapt and undergo repair in response to traumatogenic occlusion. Despite isolated reports of apical migration of the junctional epithelium accompanying excessive occlusal forces,3,17 studies generally have failed to disclose associated pocket formation while demonstrating remarkable stability of the Sharpeys fibers and periodontal fibers coronal to the alveolar bone.12,14,15,21 In the absence of existing inammation, it was noted that bony changes accompanying occlusal trauma may be reversed by discontinuing offending occlusal forces.13,30,54 A co-destructive theory55 was proposed based on a zone of irritation (marginal/interdental gingiva; gingival fibers) and zone of co-destruction (transseptal/alveolar crest bers, periodontal ligament, cementum, bone). This theory suggested that occlusal trauma in the presence of plaque-induced inammation may result in alteration of the normal pathway of inammation, and development of angular bony defects with intrabony pockets, but that occlusal trauma, in and of itself, did not cause gingivitis and periodontitis.7,8,55-58 Other studies questioned the role of occlusal trauma on this process,14,15,54 and one particular investigation identied the bacterial plaque front as the agent responsible for the severity and sites of attachment loss and associated bony defects.19 Due to difficulties encountered in the design and implementation of prospective controlled human studies, alternative development and use of animal models for prospective clinical and histologic investigations to study the effects of traumatogenic occlusion on the periodontium have been pursued.41 While such studies may provide information and insight into the trauma-associated response, repair, and the accompanying adaptive process,54 they do not duplicate the dynamics of human masticatory function or rule out significant differences between animals and man.16 Thus, such studies can serve only as a source of indirect evidence. The most widely recognized animal models used in recent times to study this topic include the beagle dog and squirrel monkey.23,49 In a series of studies,20-28 investigators used the beagle dog model and the presence or absence of continuous excessive jiggling forces (cap splint; bar-spring device) in health and experimentally induced periodontitis to study the effect of occlusal forces on the periodontium. Clinical and histologic ndings indicated that heavy occlusal forces in health and established gingivitis resulted in tooth hypermobility, increasing vascularity, vascular dilatation, and bone resorption, but no apical migration of the junctional epithelium or
103
Occlusal Trauma: Effect and Impact on the Periodontium
Volume 4 Number 1 December 1999
induction of or inuence on tissue inammation.20,21 When induced-periodontitis was accompanied by excessive jiggling forces, continued vascular permeability, osteoclastic activity, and polymorphonuclear leukocyte migration were noted, indicative of failure to adapt to the injurious force. Apical migration of the junctional epithelium was more pronounced under these conditions when compared to periodontitis sites without excessive occlusal forces.21,23,25 When jiggling trauma and tooth hypermobility were investigated in a reduced, non-inflamed periodontium that had received periodontal therapy, no progressive marginal destruction or apical migration of the junctional epithelium was observed.58 More recently, this model was used to investigate periodontal ligament tissue reactions to trauma (orthodontic elastics alternated buccally/lingually twice weekly) and ligature-induced gingival inflammation.57 In teeth exhibiting increased mobility, the coronal periodontal ligament approaching the inammatory lesion showed an increased width, increased volume of vascular structures and leukocytes, and a reduction in the percentage of collagen per tissue volume. There was also a decrease in the number of collagen bers inserting into the alveolar bone and cementum at these sites. Such changes were not observed adjacent to teeth with normal mobility.59 Other investigators used the squirrel monkey model to study the effects of the presence or absence of jiggling trauma (alternating orthodontic elastic wedging mesial and distal to septum) in health and induced periodontitis.29-37 The authors reported increased tooth mobility and bone loss (widened periodontal ligament spaces) with sustained jiggling forces, but observed little or no associated attachment loss. Removal of these forces did not reduce tooth mobility or result in bone regeneration; however, with control of plaque-associated inflammation, tooth mobility decreased and affected bone became more dense. There was, however, no change in the attachment levels or alveolar bone levels.31-36 Findings associated with these studies resulted in decreased attention to occlusal factors and focused increased therapeutic emphasis on the control of plaque, and thus, inammatory periodontal disease.30 Collectively, these studies suggest that occlusal trauma does not initiate gingivitis or periodontitis. The beagle dog studies demonstrated accelerated progression of pocket formation in the presence of ongoing destructive periodontitis,60 while the squirrel monkey model studies did not.49,54 Although the importance of the role of bacterial plaque in periodontal disease is undisputed, the inuence of occlusal trauma on the attachment level remains controversial. Clinical Studies Since occlusal trauma is a histologic lesion, clinical and radiographic indicators are necessary to assist in
104
its diagnosis. Proposed clinical indicators include mobility, occlusal prematurities, thermal sensitivity, wear facets, muscle tenderness, fractured teeth, and migration of teeth. Radiographic indicators may include altered lamina dura, widened periodontal ligament space, and evidence of root resorption and/or bone loss16,43,61-63 (see Table 1). Although increased tooth mobility is one of the most widely used indicators of occlusal trauma, it may result from bone loss independent of occlusal forces. It may also represent a self-limiting adaptive response of the host periodontium to the sustained application of occlusal forces.11,64 Progressive mobility may be suggestive of on-going occlusal trauma, but assessments and monitoring at differing points in time are necessary to make this determination.16 In a beagle dog study,65 jiggling occlusal forces in a healthy periodontium were associated with mobility, loss of marginal bone, and greater clinical probing depths, but not with changes in the connective tissue attachment level. The increase in probing depth was attributed to enlargement and alteration of the supracrestal connective tissue compartment. Longitudinal and randomized controlled trials have provided limited insight and evidence related to the effects of occlusal forces on periodontitis. In studies investigating the association of occlusal trauma and periodontitis, teeth in patients with occlusal disharmonies (centric relation-centric occlusion, balancing; or protrusive contacts) did not demonstrate any greater Table 1.
Clinical and Radiographic Indicators of Occlusal Trauma
Clinical indicators of occlusal trauma may include one or more of the following: 1. Mobility (progressive) 2. Fremitus 3. Occlusal prematurities 4.Wear facets in presence of other clinical indicators 5.Tooth migration 6. Fractured tooth (teeth) 7.Thermal sensitivity Radiographic indicators of occlusal trauma may include one or more of the following: 1.Widened PDL space 2. Bone loss (furcation; vertical; circumferential) 3. Root resorption
Ann Periodontol
Hallmon
severity of periodontitis when compared to teeth without such contacts.66,67 It is interesting to note however, that teeth demonstrating signs of occlusal trauma (e.g., bidigital mobility, functional mobility, widened periodontal ligament spaces) had greater probing depths, attachment loss, and less bone support.67,68 It has also been reported that individuals who received prophylactic occlusal adjustment as part of their treatment for periodontitis had a statistically signicant gain in mean probing attachment (0.42 mm) compared to those with no occlusal adjustment (0.02 mm). However, no reduction of tooth mobility was observed between the groups.69 Data from a similar study which evaluated the inuence of furcation involvement and tooth mobility on periodontal attachment and tooth (molar) loss indicated that teeth with furcation invasion and mobility had greater attachment loss than molars with furcation involvement and no mobility.70 A longitudinal study71 (28 years) evaluated the change in attachment level in an adult population and reported that increased age, smoking, and tooth mobility were the factors most closely associated with attachment loss. It should be noted that the occlusion was not specically evaluated in this study. In an 8-year study,72 the relationship between tooth mobility and periodontal therapy was investigated. Pockets associated with clinically mobile teeth did not respond as favorably to treatment as rm teeth with comparable severity of disease. In studies of human teeth undergoing orthodontic movement, elevated levels of interleukin (IL)-1, IL-6, tumor necrosis factor, epidermal growth factor, 2-microglobulin, and prostaglandin E in the gingival crevicular uid have been reported, compared to untreated controls.73,74 These findings should not be interpreted as a cause-and-effect association between occlusal trauma and periodontitis, but do seem to suggest the clinical relevance of tooth mobility. However, it should be noted that tooth mobility may also be the result of numerous other factors, including attachment loss, loss of alveolar bone, inammation of the supporting periodontal structures, widening of the periodontal ligament (physiologic adaption), atrophy of the periodontal ligament, and systemic disease processes which may impact the supporting periodontal tissues.11,31,41 EFFECTS OF NON-FUNCTION ON THE PERIODONTIUM In a study of non-functional teeth, periodontal changes included a decreased width of periodontal ligaments (PDL), increased thickness of cementum, inammation due to increased plaque and calculus accumulation, and increased bone loss due to supraeruption.75 These changes are consistent with those previously dened as periodontal atrophy or atrophy of disuse.76
SUMMARY AND CONCLUSIONS A dened lesion and response of the attachment apparatus has been demonstrated in association with excessive occlusal force(s), and has been termed occlusal trauma. The majority of studies investigating this condition indicate that excessive occlusal forces do not initiate plaque-induced gingival disease or connective tissue attachment loss (periodontitis). The effect of traumatogenic occlusion on the progression of periodontitis has been an area of investigative disagreement, and may represent differences in study design, model selected for study, nature of the applied occlusal forces, and means of inducing periodontal disease. These studies also suggest that tooth mobility may be clinically associated with adverse effects on the periodontium and affect long-term attachment response to therapy, but is not necessarily synonymous with occlusal trauma. REFERENCES
1. Stillman P. What is traumatic occlusion and how can it be diagnosed? J Am Dent Assoc 1925;12:1330-1338. 2. Orban B. Tissue changes in traumatic occlusion. J Am Dent Assoc 1928;15:2091-2106. 3. Stones HH. An experimental investigation into the association of traumatic occlusion with parodontal disease. Proc Royal Soc Med 1938;31:479-496. 4. Box HK. Experimental traumatogenic occlusion in sheep. Oral Health 1935;29:9-15. 5. Glickman I, Weiss LA. Role of trauma from occlusion in initiation of periodontal pocket formation in experimental animals. J Periodontol 1955;26:14-20. 6. Glickman I, Smulow JB. Alterations of the pathway of gingival inammation into the underlying tissues induced by excessive occlusal forces. J Periodontol 1962;33: 7-13. 7. Glickman I, Smulow JB. Effect of excessive occlusal forces on the pathway of gingival inflammation in humans. J Periodontol 1965;36:141-147. 8. Glickman I, Smulow JB. Further observations on the effects of trauma from occlusion in humans. J Periodontol 1967;38:280-293. 9. Macapanpan LC, Weinmann JP. The inuence of injury to the periodontal membrane on the spread of gingival inammation. J Dent Res 1954;33:263-272. 10. Goldman HM. Gingival vascular supply in induced occlusal traumatism. Oral Surg Oral Med Oral Pathol 1956;9:939-941. 11. Wentz FM, Jarabak J, Orban B. Experimental occlusal trauma imitating cuspal interferences. J Periodontol 1958;29:117-127. 12. Ramfjord SP, Kohler CA. Periodontal reaction to functional occlusal stress. J Periodontol 1959;30:95-112. 13. Mhlemann HR, Herzog H. Tooth mobility and microscopic tissue changes produced by experimental occlusal trauma. Helv Odontol Acta 1961;5:33-39. 14. Comar MD, Kollar JA, Gargiulo AW. Local irritation and occlusal trauma as co-factors in the periodontal disease process. J Periodontol-Periodontics 1969;40:193-200. 15. Stahl SS. The responses of the periodontium to combined gingival inflammation and occluso-functional stresses in four human surgical specimens. Periodontics 1968;6:14-22. 105
Occlusal Trauma: Effect and Impact on the Periodontium
Volume 4 Number 1 December 1999
16. Ramfjord SP, Ash MM Jr. Signicance of occlusion in the etiology and treatment of early, moderate and advanced periodontitis. J Periodontol 1981;52:511-517. 17. Waerhaug J. Pathogenesis of pocket formation in traumatic occlusion. J Periodontol 1955;26:107-118. 18. Waerhaug J. The infrabony pocket and its relationship to trauma from occlusion and subgingival plaque. J Periodontol 1979;50:355-365. 19. Waerhaug J. The angular bone defect and its relationship to trauma from occlusion and downgrowth of subgingival plaque. J Clin Periodontol 1979;6:61-82. 20. Svanberg G, Lindhe J. Experimental tooth hypermobility in the dog. Odontol Revy 1973;24:269-282. 21. Svanberg G, Lindhe J. Vascular reactions in the periodontal ligament incident to trauma from occlusion. J Clin Periodontol 1974;1:58-69. 22. Svanberg G. Inuence of trauma from occlusion on the periodontium of dogs with normal or inamed gingiva. Odontol Revy 1974;25:165-178. 23. Lindhe J, Svanberg G. Inuence of trauma from occlusion on progression of experimental periodontitis in the beagle dog. J Clin Periodontol 1974;1:3-14. 24. Lindhe J, Ericsson I. Inuence of trauma from occlusion on reduced but healthy periodontal tissues in dogs. J Clin Periodontol 1976;3:110-122. 25. Ericsson I, Lindhe J. Effect of longstanding jiggling on experimental marginal periodontitis in the beagle dog. J Clin Periodontol 1982;9:497-503. 26. Lindhe J, Ericsson I. The effect of elimination of jiggling forces on periodontally exposed teeth in the dog. J Periodontol 1982;53:562-567. 27. Ericsson I, Lindhe J. Lack of signicance of increased tooth mobility in experimental periodontitis. J Periodontol 1984;55:447-452. 28. Nyman S, Lindhe J, Ericsson I. The effect of progressive tooth mobility on destructive periodontitis in the dog. J Clin Periodontol 1978;5:213-225. 29. Polson AM, Meitner SW, Zander HA. Trauma and progression of marginal periodontitis in squirrel monkeys. III. Adaptation of interproximal alveolar bone to repetitive injury. J Periodont Res 1976;11:279-289. 30. Polson AM. The relative importance of plaque and occlusion in periodontal disease. J Clin Periodontol 1986; 13:923-927. 31. Polson AM, Kantor ME, Zander HA. Periodontal repair after reduction of inammation. J Periodont Res 1979; 14:520-525. 32. Polson AM, Meitner SW, Zander HA. Trauma and progression of marginal periodontitis in squirrel monkeys. IV. Reversibility of bone loss due to trauma alone and trauma superimposed upon periodontitis. J Periodont Res 1976;11:290-298. 33. Kantor M, Polson AM, Zander HA. Alveolar bone regeneration after the removal of inammatory and traumatic factors. J Periodontol 1976;47:687-695. 34. Perrier M, Polson A. The effect of progressive and increasing tooth hypermobility on reduced but healthy periodontal supporting tissues. J Periodontol 1982; 53:152-157. 35. Polson AM, Zander HA. Effect of periodontal trauma upon intrabony pockets. J Periodontol 1983;54:586591. 36. Polson AM, Adams RA, Zander HA. Osseous repair in the presence of active tooth hypermobility. J Clin Periodontol 1983;10:370-379. 37. Polson AM. Trauma and progression of marginal periodontitis in squirrel monkeys. II. Co-destructive factors 106
38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. 52. 53. 54. 55. 56. 57. 58. 59.
60. 61. 62.
of periodontitis and mechanically-produced injury. J Periodont Res 1974;9:108-113. The American Academy of Periodontology. Glossary of Periodontal Terms. Chicago: The American Academy of Periodontology; 1992:34. Weinmann JP. The adaptation of the periodontal membrane to physiologic and pathologic changes. Oral Surg Oral Med Oral Pathol 1955;8:977-981. Svanberg GK, King GJ, Gibbs CH. Occlusal considerations in periodontology. Periodontol 2000,1995;9:106-117. Gher ME. Non-surgical pocket therapy: Dental occlusion. Ann Periodontol 1996;1:567-580. Consensus Report: Occlusal trauma. Proceedings of the World Workshop in Clinical Periodontics. Chicago: The American Academy of Periodontology; 1989:III-1/III-23. Bjorndahl O. Periodontal traumatism. J Periodontol 1958; 29:223-231. Box HK. Treatment of the Periodontal Pocket. Toronto: University of Toronto Press; 1928:28-32. Posselt U, Emslie RD. Occlusal disharmonies and their effect on periodontal diseases. Int Dent J 1959;9:367381. Posselt U. Occlusion related to periodonticsReview of literature. In: Ramfjord SP, Kerr DA, Ash MM, eds. World Workshop in Periodontics 1966;225-270. Reinhardt RR, Pao YC, Krecji RF. Periodontal ligament stresses in the initiation of occlusal traumatism. J Periodont Res 1984;19:238-246. Bhaskar SN, Orban B. Experimental occlusal trauma. J Periodontol 1955;26:270-284. Polson AM. Interrelationship of inammation and tooth mobility (trauma) in pathogenesis of periodontal disease. J Clin Periodontol 1980;7:35l-360. Oppenheim A. Human tissue response to orthodontic intervention of long and short duration. Am J Orthod Oral Surg 1942;28:263-301. Grant D, Bernick S. The periodontium of ageing humans. J Periodontol 1972;43:660-667. HaneyJ, Leknes KN, Lie T, Selvig KA, Wikesj UME. Cemental tear related to rapid periodontal breakdown: A case report. J Periodontol 1992;63:220-224. Ishikawa I, Oda S, Hayashi J, Arakawa S. Cervical cemental tears in older patients with adult periodontitis. Case reports. J Periodontol 1996;67:15-20. Polson AM, Heijl LC. Occlusion and periodontal disease. Dent Clin North Am 1980;24:783-795. Glickman I. Inammation and trauma from occlusion, co-destructive factors in chronic periodontal disease. J Periodontol 1963;34:5-10. Glickman I. Clinical signicance of trauma from occlusion. J Am Dent Assoc 1965;70:607-618. Glickman I. Occlusion and the periodontium. J Dent Res 1967;46(Suppl. 1):53-59. Ericsson I, Lindhe J. Lack of effect of trauma from occlusion on the recurrence of experimental periodontitis. J Clin Periodontol 1977;4:115-127. Biancu S, Ericsson I, Lindhe J. Periodontal ligament tissue reactions to trauma and gingival inammation. An experimental study in the beagle dog. J Clin Periodontol 1995;22:772-779. Ericsson I. The combined effects of plaque and physical stress on periodontal tissues. J Clin Periodontol 1986; 13:918-922. Glover ME. Occlusal therapy and its role in the etiology and treatment of periodontal diseases. Tex Dent J 1988;105:44-47. Wank GS, Kroll YJ. Occlusal trauma. An evaluation of
Ann Periodontol
Hallmon
63. 64. 65. 66. 67. 68. 69.
70.
71.
72. 73.
its relationship to periodontal prostheses. Dent Clin North Am 1981;25:511-532. Burgett FG. Trauma from occlusion - periodontal concerns. Dent Clin North Am 1995;39:301-311. Gher ME. Changing concepts. The effects of occlusion on periodontitis. Dent Clin North Am 1998;42:285-299. Neiderud A-M, Ericsson I, Lindhe J. Probing pocket depth at mobile/nonmobile teeth. J Clin Periodontol 1992;19:754-759. Shefter GJ, McFall WT Jr. Occlusal relations and periodontal status in human adults. J Periodontol 1984; 55:368-374. Pihlstrom BL, Anderson KA, Aeppli D, Schaffer EM. Association between signs of trauma from occlusion and periodontitis. J Periodontol 1986;57:1-6. Jin LJ, Cao CF. Clinical diagnosis of trauma from occlusion and its relation with severity of periodontitis. J Clin Periodontol 1992;19:92-97. Burgett FG, Ramfjord SP, Nissle RR, Morrison EC, Charbeneau TD, Caffesse RG. A randomized trial of occlusal adjustment in the treatment of periodontitis patients. J Clin Periodontol 1992;19:381-387. Wang H-L, Burgett FG, Shyr Y, Ramfjord S. The inuence of molar furcation involvement and mobility on future clinical periodontal attachment loss. J Periodontol 1994;65:25-29. Ismail AI, Morrison EC, Burt BA, Caffesse RG, Kavanagh MT. Natural history of periodontal disease in adults: Findings from the Tecumseh periodontal disease study. J Dent Res 1990;69:430-435. Fleszar TJ, Knowles JW, Morrison EC, Burgett FG, Nissle RR, Ramfjord SP. Tooth mobility and periodontal therapy. J Clin Periodontol 1980;7:495-505. Grieve WG, Johnson GK, Moore RN, Reinhardt RA, DuBois LM. Prostaglandin E (PGE) and interleukin-1 (IL-1) levels in gingival crevicular uid during human orthodontic tooth movement. Am J Orthod Dentofacial Orthop 1994;105:369-374.
74. Uematsu S, Mogi M, Deguchi T. Interleukin (IL)-1, IL6, tumor necrosis factor-, epidermal growth factor, and 2-microglobulin levels are elevated in gingival crevicular uid during human orthodontic tooth movement. J Dent Res 1996;75:562-567. 75. Pihlstrom, BL, Ramfjord SP. Periodontal effects of nonfunction in monkeys. J Periodontol 1971;42:748-756. 76. Goldman HM, Schluger S, Fox L, Cohen DW. Periodontal Therapy, 2nd ed. St. Louis: CV Mosby Co.; 1960:5052. Send reprint requests to: Dr. William W. Hallmon, TAMUS Baylor College of Dentistry, Department of Periodontics, 3302 Gaston Avenue, Dallas, TX 75246. Fax: 214/828-8411; e-mail: whallmon@tambcd.edu
107
S-ar putea să vă placă și
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- EndoperioDocument21 paginiEndoperioLuis KabreraÎncă nu există evaluări
- Bayram 2017Document4 paginiBayram 2017Luis KabreraÎncă nu există evaluări
- Antibacterial Activity of Calcium Hydroxide CombinDocument9 paginiAntibacterial Activity of Calcium Hydroxide CombinLuis KabreraÎncă nu există evaluări
- 1 s2.0 S134900791630038X MainDocument12 pagini1 s2.0 S134900791630038X MainLuis KabreraÎncă nu există evaluări
- 1 s2.0 S1121417115000205 MainDocument5 pagini1 s2.0 S1121417115000205 MainLuis KabreraÎncă nu există evaluări
- Artiuculo Pasta TriantibioticaDocument8 paginiArtiuculo Pasta TriantibioticaLuis KabreraÎncă nu există evaluări
- Annrcse01531 0070Document2 paginiAnnrcse01531 0070Luis KabreraÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
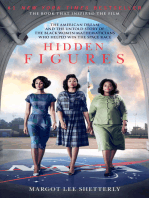
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Basal Osseointegrated Implants ClassificDocument7 paginiBasal Osseointegrated Implants ClassificAnkur SaladaÎncă nu există evaluări
- Appendix E EditedDocument6 paginiAppendix E EditedReyn Christian Tajos OmegaÎncă nu există evaluări
- Chapter # 1Document19 paginiChapter # 1Hadiqa Afzal855Încă nu există evaluări
- Minor Connectors Rests and Rest Seats in Removable Dental ProsthesisDocument68 paginiMinor Connectors Rests and Rest Seats in Removable Dental ProsthesismujtabaÎncă nu există evaluări
- Centric Relation: Handout AbstractsDocument21 paginiCentric Relation: Handout Abstractsizeldien5870Încă nu există evaluări
- Interdisciplinary Treat Planning ChapterDocument56 paginiInterdisciplinary Treat Planning ChapterJulio César Huayllasco de la Cruz0% (1)
- The International Journal of Periodontics & Restorative DentistryDocument8 paginiThe International Journal of Periodontics & Restorative DentistrySeptimiu TiplicaÎncă nu există evaluări
- DP OussamaDocument4 paginiDP OussamaDinda Tryana SembiringÎncă nu există evaluări
- Asm 275 Unit 2 Lab Answers and QuestionsDocument24 paginiAsm 275 Unit 2 Lab Answers and QuestionsTony Liu100% (15)
- Metallic and Plastic Denture Base Materials Used For Partially Edentulous CasesDocument4 paginiMetallic and Plastic Denture Base Materials Used For Partially Edentulous Caseskhaled alahmadÎncă nu există evaluări
- Estimating The Age of The HorseDocument3 paginiEstimating The Age of The HorsegustavoxinaidersÎncă nu există evaluări
- BCP Perawat Gigi Ahli (Bukti Catatan Pribadi/ Harian)Document7 paginiBCP Perawat Gigi Ahli (Bukti Catatan Pribadi/ Harian)Devy EkaputriÎncă nu există evaluări
- Gingivitis Associated With Systemic Diseases (Diabetes Mellitus &leukemia)Document18 paginiGingivitis Associated With Systemic Diseases (Diabetes Mellitus &leukemia)Sana RashadÎncă nu există evaluări
- Fa 50Document5 paginiFa 50Sumidhi 14Încă nu există evaluări
- 10.2 Major Surgical ProceduresDocument22 pagini10.2 Major Surgical ProceduresishtiiiÎncă nu există evaluări
- Functions of The Digestive SystemDocument12 paginiFunctions of The Digestive SystemRomeo Penyihir ChrestomancyÎncă nu există evaluări
- Corporate Today Nobel Biocare Global Symposium June 24 2016 0116-13-12 2Document2 paginiCorporate Today Nobel Biocare Global Symposium June 24 2016 0116-13-12 2Dr.SnehalÎncă nu există evaluări
- Frush y FisherDocument24 paginiFrush y FisherValeria Vanessa Membreño Agüero100% (1)
- Vita MFT Forme I ObliciDocument1 paginăVita MFT Forme I Oblici25082608Încă nu există evaluări
- A Novel Method For Fragment Reattachment After Post Placement - StyleitalianoDocument6 paginiA Novel Method For Fragment Reattachment After Post Placement - StyleitalianoDr. Valeriu Anghileanu Zubná ambulanciaÎncă nu există evaluări
- Smile Direct ClubDocument2 paginiSmile Direct ClubLéopold deCrewÎncă nu există evaluări
- Innovative Sonic Powered Irrigation: Three Benefi Ts in One SolutionDocument8 paginiInnovative Sonic Powered Irrigation: Three Benefi Ts in One Solutionpatel keralÎncă nu există evaluări
- Ayurveda ExtractionDocument9 paginiAyurveda ExtractionDr-Beneesh VK0% (1)
- Evidence Based EndodonticsDocument114 paginiEvidence Based EndodonticsSanket PandeyÎncă nu există evaluări
- Tips For The NDECCDocument2 paginiTips For The NDECCMagda Jakubowska-EwiczÎncă nu există evaluări
- Case Study Oral PathologyDocument3 paginiCase Study Oral Pathologyapi-292187519Încă nu există evaluări
- Ijomi 2017 Vol 32 P 1296 1307Document12 paginiIjomi 2017 Vol 32 P 1296 1307John MacioÎncă nu există evaluări
- Functional Occlusion: Science-Driven ManagementDocument4 paginiFunctional Occlusion: Science-Driven Managementrunit nangaliaÎncă nu există evaluări
- T1 - Biomechanics of Torque - Vijay Jayde PDFDocument7 paginiT1 - Biomechanics of Torque - Vijay Jayde PDFAnonymous LNLz3MtVÎncă nu există evaluări
- Determinants of OcclusionDocument68 paginiDeterminants of OcclusionPhoebe DavidÎncă nu există evaluări