Documente Academic
Documente Profesional
Documente Cultură
Xerophtalmia - Khurana
Încărcat de
Aslesa Wangpathi PagehgiriDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Xerophtalmia - Khurana
Încărcat de
Aslesa Wangpathi PagehgiriDrepturi de autor:
Formate disponibile
CHAPTER
19
19
Systemic Ophthalmology
Disorders of skin and mucous membranes Haematological diseases OCULAR ABNORMALITIES IN TRISOMIES ADVERSE OCULAR EFFECTS OF COMMON SYSTEMIC DRUGS
OCULAR MANIFESTATIONS OF SYSTEMIC DISEASES Introduction Nutritional deficiences Xerophthalmia Systemic infections Metabolic disorders
OCULAR MANIFESTATIONS OF SYSTEMIC DISEASES
INTRODUCTION
Ocular involvement in systemic disorders is quite frequent. It is imperative for the ophthalmologists as well as physicians to be well conversant with these. Many a time, the ocular manifestations may be the presenting signs and the ophthalmologist will refer the patient to the concerned specialist for diagnosis and/or management of the systemic disease. While, in other cases the opinion for ocular involvement may be sought for by the physician who knows to look for it. Ocular lesions of the common systemic disorders are enumerated and a few important ones are described here.
OCULAR MANIFESTATIONS OF NUTRITIONAL DEFICIENCES
the eyes due to conjunctival irritation and vascularisation of the cornea. 4. Deficiency of vitamin C. It may be associated with haemorrhages in the conjunctiva, lids, anterior chamber, retina and orbit. It also delays wound healing. 5. Deficiency of vitamin D. It may be associated with zonular cataract, papilloedema and increased lacrimation.
XEROPHTHALMIA
They term xerophthalmia is now reserved (by a joint WHO and USAID Committee, 1976) to cover all the ocular manifestations of vitamin A deficiency, including not only the structural changes affecting the conjunctiva, cornea and occasionally retina, but also the biophysical disorders of retinal rods and cones functions.
Etiology
1. Deficiency of vitamin A. Ocular manifestations of vitamin A deficiency are referred to as xerophthalmia. 2. Deficiency of vitamin B1 (thiamine). It can cause corneal anaesthesia, conjunctival and corneal dystrophy and acute retrobulbar neuritis. 3. Deficiency of vitamin B2 (riboflavin). It can produce photophobia and burning sensation in
It occurs either due to dietary deficiency of vitamin A or its defective absorption from the gut. It has long been recognised that vitamin A deficiency does not occur as an isolated problem but is almost invariably accompanied by protein-energy malnutrition (PEM) and infections.
WHO classification (1982)
The new xerophthalmia classification (modification of original 1976 classification) is as follows:
434
Comprehensive OPHTHALMOLOGY
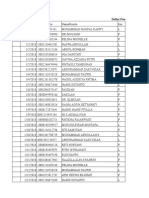
XN X1A X1B X2 X3A X3B XS XF
Night blindness Conjunctival xerosis Bitots spots Corneal xerosis Corneal ulceration/keratomalacia affecting less than one-third corneal surface Corneal ulceration/keratomalacia affecting more than one-third corneal surface. Corneal scar due to xerophthalmia Xerophthalmic fundus.
Clinical features
1. X N (night blindness). It is the earliest symptom of xerophthalmia in children. It has to be elicited by taking detailed history from the guardian or relative. 2. X1A (conjunctival xerosis). It consists of one or more patches of dry, lustreless, nonwettable conjunctiva (Fig. 19.1), which has been well described as emerging like sand banks at receding tide when the child ceases to cry. These patches almost always involve the inter-palpebral area of the temporal quadrants and often the nasal quadrants as well. In more advanced cases, the entire bulbar conjunctiva may be affected. Typical xerosis may be associated with conjunctival thickening, wrinkling and pigmentation.
Fig. 19.2. Xerophthalmia, stage XIB: Bitot spots.
4. X2 (corneal xerosis). The earliest change in the cornea is punctate keratopathy which begins in the lower nasal quadrant, followed by haziness and/or granular pebbly dryness (Fig. 19.3). Involved cornea lacks lustre. 5. X3A and X3B (corneal ulceration/keratomalacia), Stromal defects occur in the late stage due to colliquative necrosis and take several forms. Small ulcers (1-3 mm) occur peripherally; they are characteristically circular, with steep margins and are sharply demarcated (Fig. 19.4). Large ulcers and areas of necrosis may extend centrally or involve the entire cornea. If appropriate therapy is instituted immediately, stromal defects involving less than one-third of corneal surface (X3A) usually heal, leaving some useful vision. However, larger stromal defects (X3B) (Fig. 19.5) commonly result in blindness.
Fig. 19.1. Xerophthalmia, stage XIA: Conjunctival xerosis.
3. X1B (Bitots spots). It is an extension of the xerotic process seen in stage X1A. The Bitots spot is a raised, silvery white, foamy, triangular patch of keratinised epithelium, situated on the bulbar conjunctiva in the inter-palpebral area (Fig. 19.2). It is usually bilateral and temporal, and less frequently nasal.
Fig. 19.3. Xerophthalmia, stage X2: Corneal xerosis.
SYSTEMIC OPHTHALMOLOGY
435
Fig. 19.4. Xerophthalmia, stage X3A: Keratomalacia involving less than one-third of corneal surface.
Fig. 19.6. Xerophthalmia, stage XS: Corneal scars.
Fig. 19.5. Xerophthalmia, stage X3B: Keratomalacia involving more than one-third of corneal surface.
Fig. 19.7. Xerophthalmia, stage XF: Xerophthalmic fundus.
6. XS (corneal scars). Healing of stromal defects results in corneal scars of different densities and sizes which may or may not cover the pupillary area (Fig. 19.6). A detailed history is required to ascertain the cause of corneal opacity. 7. XFC (Xerophthalmic fundus). It is characterized by typical seed-like, raised, whitish lesions scattered uniformly over the part of the fundus at the level of optic disc (Fig. 19.7).
Treatment
2. Vitamin A therapy. Treatment schedules apply to all stages of active xerophthalmia viz. XN, X1A, X1B, X2, X3A and X3B. Oral administration is the recommended method of treatment. However, in the presence of repeated vomiting and severe diarrhoea, intramuscular injections of water-miscible preparation should be preferred. The WHO recommended schedule is as given below: i. All patients above the age of 1 year (except women of reproductive age): 200,000 IU of vitamin A orally or 100,000 IU by intramuscular injection should be given immediately on diagnosis and repeated the following day and 4 weeks later. ii. Children under the age of 1 year and children of any age who weigh less than 8 kg should be treated with half the doses for patients of more than 1 year of age.
It includes local ocular therapy, vitamin A therapy and treatment of underlying general disease. 1. Local ocular therapy. For conjunctival xerosis artificial tears (0.7 percent hydroxypropyl methyl cellulose or 0.3 percent hypromellose) should be instilled every 3-4 hours. In the stage of keratomalacia, full-fledged treatment of bacterial corneal ulcer should be instituted (see pages 120-123).
436
Comprehensive OPHTHALMOLOGY
iii. Women of reproductive age, pregnant or not: (a) Those having night blindness (XN), conjunctival xerosis (X1A) and Bitots spots (X1B) should be treated with a daily dose of 10,000 IU of vitamin A orally (1 sugar coated tablet) for 2 weeks. (b) For corneal xerophthalmia, administration of full dosage schedule (described for patients above 1 year of age) is recommended. 3. Treatment of underlying conditions such as PEM and other nutritional disorders, diarrhoea, dehydration and electrolyte imbalance, infections and parasitic conditions should be considered simultaneously.
Prophylaxis against xerophthalmia
2. Medium-term approach. It includes food fortification with vitamin A. 3. Long-term approach. It should be the ultimate aim. It implies promotion of adequate intake of vitamin A rich foods such as green leafy vegetables, papaya and drum- sticks (Fig. 19.8). Nutritional health education should be included in the curriculum of school children.
The three major known intervention strategies for the prevention and control of vitamin A deficiency are: 1. Short-term approach. It comprises periodic administration of vitamin A supplements. WHO recommended, universal distribution schedule of vitamin A for prevention is as follows: i. Infants 6-12 100,000 IU orally every months old and 3-6 months. any older children who weigh less than 8 kg. ii. Children over 200,000 IU orally every 1 year and under 6 months. 6 years of age iii. Lactating 20,000 IU orally once at mothers delivery or during the next 2 months. This will raise the concentration of vitamin A in the breast milk and therefore, help to protect the breastfed infant. iv. Infants less 50,000 IU orally should than 6 months be given before they old, not being attain the age of 6 breastfed. months. A revised schedule of vitamin A supplements being followed in India since August 1992, under the programme named as Child Survival and Safe Motherhood (CSSM) is as follows: First dose (1 lakh I.U.)at 9 months of age along with measles vaccine. Second dose (2 lakh I.U.)at 18 months of age along with booster dose of DPT/OPV. Third dose (2 lakh I.U.)at 2 years of age.
Fig. 19.8. Rich sources of vitamin A.
Note. The short-term approach has been mostly in vogue especially in Asia. The best option perhaps is a combination of all the three methods with a gradual weaning away of the short-term approach. OCULAR MANIFESTATIONS OF SYSTEMIC INFECTIONS
A. VIRAL INFECTIONS Measles. Ocular lesions are: catarrhal conjunctivitis,
Kopliks spots on conjunctiva, corneal ulceration, optic neuritis and retinitis. Mumps. Ocular involvement may occur as conjunctivitis, keratitis, acute dacryoadenitis and uveitis. Rubella. Ocular lesions seen in rubella (German measles) are congenital microphthalmos, cataract, glaucoma, chorioretinitis and optic atrophy. Whooping cough. There may occur subconjunctival haemorrhages and rarely orbital haemorrhage leading to proptosis.
Ocular involvement in AIDS
AIDS (Acquired Immune Deficiency Syndrome) is caused by Human immunodeficiency virus (HIV) which is an RNA retrovirus.
S-ar putea să vă placă și
- Complications in UveitisDe la EverandComplications in UveitisFrancesco PichiÎncă nu există evaluări
- A Practical Manual of Diabetic Retinopathy ManagementDe la EverandA Practical Manual of Diabetic Retinopathy ManagementÎncă nu există evaluări
- Differences Between Conjunctival and Ciliary CongestionDocument6 paginiDifferences Between Conjunctival and Ciliary CongestionParam KahalÎncă nu există evaluări
- Vitamin A DeficiencyDocument35 paginiVitamin A DeficiencySemina LimbuÎncă nu există evaluări
- 5.vit A DeficiencyDocument21 pagini5.vit A DeficiencyDominic SkskÎncă nu există evaluări
- Fat Soluble Vitamin RevisedDocument80 paginiFat Soluble Vitamin RevisedsumitÎncă nu există evaluări
- Xero PH Thal MiaDocument1 paginăXero PH Thal MiaRavan WidiÎncă nu există evaluări
- Guidelines For The Management of Corneal Ulcer WHODocument36 paginiGuidelines For The Management of Corneal Ulcer WHOichalledhaÎncă nu există evaluări
- Xerophthalmia 190715182114Document31 paginiXerophthalmia 190715182114Murali DharanÎncă nu există evaluări
- PHCN Practical RecordDocument35 paginiPHCN Practical RecordDola KalyanÎncă nu există evaluări
- Xerophthalmia (Vitamin A Deficiency) - Clinical GuidelinesDocument2 paginiXerophthalmia (Vitamin A Deficiency) - Clinical GuidelinesLintya AndaniÎncă nu există evaluări
- Vernal Keratoconjunctivitis: Why Is Allergic Eye Disease A Problem For Eye Workers?Document3 paginiVernal Keratoconjunctivitis: Why Is Allergic Eye Disease A Problem For Eye Workers?darendraabimayuÎncă nu există evaluări
- July Big Mock 2021 AnswersDocument23 paginiJuly Big Mock 2021 AnswershamzabinaqÎncă nu există evaluări
- Eye Care Manajemen PDFDocument6 paginiEye Care Manajemen PDFKiki dwi PratiwiÎncă nu există evaluări
- PHCN PracticalDocument33 paginiPHCN PracticalDola KalyanÎncă nu există evaluări
- Suppurative KeratitisDocument30 paginiSuppurative KeratitisTatik Handayani100% (1)
- Vit A DeficiencyDocument27 paginiVit A DeficiencyNatnaelÎncă nu există evaluări
- Managing Corneal Disease: Focus On Suppurative Keratitis: Fist Steps in ManagementDocument3 paginiManaging Corneal Disease: Focus On Suppurative Keratitis: Fist Steps in ManagementTatik HandayaniÎncă nu există evaluări
- Ophthalmology - Systemic - Community OphthalmologyDocument7 paginiOphthalmology - Systemic - Community OphthalmologyjbtcmdtjjvÎncă nu există evaluări
- OpthaDocument5 paginiOpthavarun2k6Încă nu există evaluări
- What Is The Best Treatment Approach For Severe Blepharitis?: Key Words: Blepharitis ClinicalDocument3 paginiWhat Is The Best Treatment Approach For Severe Blepharitis?: Key Words: Blepharitis ClinicalnicoÎncă nu există evaluări
- Uveitis PDFDocument3 paginiUveitis PDFTri BasukiÎncă nu există evaluări
- MainDocument3 paginiMainomidazadmehr1375Încă nu există evaluări
- WHO NMH NHD EPG 14.4 Eng PDFDocument6 paginiWHO NMH NHD EPG 14.4 Eng PDFIga Amany ZulfaÎncă nu există evaluări
- And Treatment Blepharokeratoconjunctivitis in Children: DiagnosisDocument5 paginiAnd Treatment Blepharokeratoconjunctivitis in Children: DiagnosislordaponkÎncă nu există evaluări
- Tubercular Posterior SchleritisDocument6 paginiTubercular Posterior SchleritisInayatul muthmainnahÎncă nu există evaluări
- Case Report Fusarium Endophthalmitis FollowingDocument5 paginiCase Report Fusarium Endophthalmitis FollowingKreAch3RÎncă nu există evaluări
- Common Bacterial Skin InfectionsDocument6 paginiCommon Bacterial Skin InfectionsagusÎncă nu există evaluări
- A Clinicopathological Study of Vernal Conjunctivitis in Urban and Rural Areas of Eastern India: A Hospital Based StudyDocument8 paginiA Clinicopathological Study of Vernal Conjunctivitis in Urban and Rural Areas of Eastern India: A Hospital Based StudyMuhammad AbdillahÎncă nu există evaluări
- Ini Cet 22ND July 2021Document8 paginiIni Cet 22ND July 2021gksah711Încă nu există evaluări
- Disorders of The EyeDocument16 paginiDisorders of The Eyelisette_sakuraÎncă nu există evaluări
- Successful Treatment of Vitiligo With 0.1% Tacrolimus OintmentDocument4 paginiSuccessful Treatment of Vitiligo With 0.1% Tacrolimus OintmentwillychirinosÎncă nu există evaluări
- Pediatrics With Answers and ExplanationsDocument77 paginiPediatrics With Answers and ExplanationsRamy Elmasry100% (6)
- Experimental Study On Cryotherapy For Fungal Corneal Ulcer: Researcharticle Open AccessDocument9 paginiExperimental Study On Cryotherapy For Fungal Corneal Ulcer: Researcharticle Open AccessSusPa NarahaÎncă nu există evaluări
- Sal Agar 2015Document2 paginiSal Agar 2015occcÎncă nu există evaluări
- OPTHALMIA NEONATORUM: Is An Eye Infection That Occurs at Birth or During The First MonthDocument4 paginiOPTHALMIA NEONATORUM: Is An Eye Infection That Occurs at Birth or During The First Monthcharuz_092823Încă nu există evaluări
- Eyelid Disorders - Diagnosis and Management - AAFPDocument15 paginiEyelid Disorders - Diagnosis and Management - AAFPMufassiraturrahmahÎncă nu există evaluări
- Applsci 11 08323Document8 paginiApplsci 11 08323atmokotomoÎncă nu există evaluări
- First Class Test Topic: GlaucomaDocument10 paginiFirst Class Test Topic: GlaucomaUkash AkramÎncă nu există evaluări
- Prevention of Blindness in Leprosy: An Overview of The Relevant Clinical and Programme-Planning IssuesDocument9 paginiPrevention of Blindness in Leprosy: An Overview of The Relevant Clinical and Programme-Planning IssuesBudi KhangÎncă nu există evaluări
- Dipake Lamellar Ichthyosis enDocument6 paginiDipake Lamellar Ichthyosis enprajnamitaÎncă nu există evaluări
- Jurnal Maharani PutriDocument7 paginiJurnal Maharani Putrikaja177.kevinÎncă nu există evaluări
- Scedosporium Apiospermium Keratitis: A Case: Case Report Open AccessDocument5 paginiScedosporium Apiospermium Keratitis: A Case: Case Report Open AccessqalbiÎncă nu există evaluări
- Jurnal English JhuvanDocument12 paginiJurnal English JhuvanJhuvan FernandoÎncă nu există evaluări
- Journal Reading: Update On The Management of Infectious KeratitisDocument35 paginiJournal Reading: Update On The Management of Infectious KeratitisninataniaaaÎncă nu există evaluări
- Corneal Ulcer: Prepared By: Renuka Shrestha Roll No: 29 PBBN 3rd Year SMTCDocument41 paginiCorneal Ulcer: Prepared By: Renuka Shrestha Roll No: 29 PBBN 3rd Year SMTCsushma shresthaÎncă nu există evaluări
- Ptisis BulbiDocument6 paginiPtisis Bulbiruditacitrahaha100% (1)
- A Case of Fungal KeratitisDocument6 paginiA Case of Fungal KeratitisPhilip McNelsonÎncă nu există evaluări
- Who Classification of Vitamin A Deficiency and ManagementDocument20 paginiWho Classification of Vitamin A Deficiency and Managementapi-3823785100% (2)
- 5 XerophtalmiaDocument36 pagini5 XerophtalmiaMarshet GeteÎncă nu există evaluări
- Vitrectomy in Endophthalmitis: Kapil Bhatia, Avinash Pathengay and Manav KheraDocument17 paginiVitrectomy in Endophthalmitis: Kapil Bhatia, Avinash Pathengay and Manav KheraGrady ChristianÎncă nu există evaluări
- Post Op ComplicationDocument7 paginiPost Op ComplicationSurendar KesavanÎncă nu există evaluări
- Entropion and Ectropion: Disease-a-MonthDocument6 paginiEntropion and Ectropion: Disease-a-MonthWILMER HUANGAÎncă nu există evaluări
- Vitamin-A Prophylaxis Programme 0rDocument38 paginiVitamin-A Prophylaxis Programme 0rShubhendu ChattopadhyayÎncă nu există evaluări
- Pharma Module 4Document4 paginiPharma Module 4Chelsy Sky SacanÎncă nu există evaluări
- Management of Bitot SpotDocument2 paginiManagement of Bitot SpotEsther EunikeÎncă nu există evaluări
- Treating Corneal Ulceration in Dogs Part 2 Deep UlcersDocument16 paginiTreating Corneal Ulceration in Dogs Part 2 Deep UlcersAndreea MayaÎncă nu există evaluări
- Pterygium EmedicineDocument9 paginiPterygium EmedicineThomas SmithÎncă nu există evaluări
- Xerophthalmia (Vitamin A Deficiency) : Ointment, One Application 2 Times Daily (Do Not Apply EyeDocument1 paginăXerophthalmia (Vitamin A Deficiency) : Ointment, One Application 2 Times Daily (Do Not Apply EyeDita Ambarsari SyafruddinÎncă nu există evaluări
- Differential Diagnosis of The Swollen Red Eyelid - AAFPDocument16 paginiDifferential Diagnosis of The Swollen Red Eyelid - AAFPtorome4979Încă nu există evaluări
- Asbtrak Case Report Aslesa Wangpathi Pagehgiri (Turi Cephalia)Document3 paginiAsbtrak Case Report Aslesa Wangpathi Pagehgiri (Turi Cephalia)Aslesa Wangpathi PagehgiriÎncă nu există evaluări
- Clinical Study: Retrograde Intrarenal Surgery Versus Percutaneous Lithotripsy To Treat Renal Stones 2-3 CM in DiameterDocument5 paginiClinical Study: Retrograde Intrarenal Surgery Versus Percutaneous Lithotripsy To Treat Renal Stones 2-3 CM in DiameterAslesa Wangpathi PagehgiriÎncă nu există evaluări
- Febrile Neutropenia GuidelineDocument8 paginiFebrile Neutropenia GuidelineAslesa Wangpathi PagehgiriÎncă nu există evaluări
- Managing Placenta Accreta: Incidence and PathophysiologyDocument9 paginiManaging Placenta Accreta: Incidence and PathophysiologyAslesa Wangpathi PagehgiriÎncă nu există evaluări
- Common Communicable DiseasesDocument13 paginiCommon Communicable DiseasesSanthosh.S.U100% (1)
- PQ 168 MMR MSD Pi July2008Document7 paginiPQ 168 MMR MSD Pi July2008Charles AnthonyÎncă nu există evaluări
- Donor Selection and Blood CollectionDocument14 paginiDonor Selection and Blood CollectionMary ChristelleÎncă nu există evaluări
- Foreign Products Tables PDFDocument13 paginiForeign Products Tables PDFDaphenyÎncă nu există evaluări
- CDC MMR, MMR+V, MMRV Seizure RatesDocument4 paginiCDC MMR, MMR+V, MMRV Seizure RatesVaccineInformation83% (6)
- Perinatal InfectionsDocument24 paginiPerinatal InfectionsAlexandra OanaÎncă nu există evaluări
- Question 1Document87 paginiQuestion 1hemihemaÎncă nu există evaluări
- Integ CD TipsDocument2 paginiInteg CD TipsNia KayeÎncă nu există evaluări
- (IJIT-V7I2P6) :B.Rajalakshmi, G.Sanjana DeviDocument5 pagini(IJIT-V7I2P6) :B.Rajalakshmi, G.Sanjana DeviIJITJournalsÎncă nu există evaluări
- Mumps and RubellaDocument40 paginiMumps and Rubellalaxmi prasannaÎncă nu există evaluări
- Park psm74b - 1Document9 paginiPark psm74b - 1Ch RajeshÎncă nu există evaluări
- REPUBLIC ACT No 10152Document5 paginiREPUBLIC ACT No 10152dteroseÎncă nu există evaluări
- Sample Final Year Exam - 2017Document26 paginiSample Final Year Exam - 2017Taima FayezÎncă nu există evaluări
- Autism OverviewDocument6 paginiAutism Overviewidno1008Încă nu există evaluări
- Statistics and Propaganda: by Jon RappoportDocument6 paginiStatistics and Propaganda: by Jon RappoportSkogspilen Sprett100% (1)
- PNLEDocument34 paginiPNLEnjÎncă nu există evaluări
- Ls 0-2-23d95 024d5889fe646-The Clat Post January 2020 CompressedDocument32 paginiLs 0-2-23d95 024d5889fe646-The Clat Post January 2020 CompressedNiti Kaushik100% (1)
- Viral Infections Part 1 by Nicolle Ann Pancho (Pediatrics Rotation)Document67 paginiViral Infections Part 1 by Nicolle Ann Pancho (Pediatrics Rotation)Nicolle PanchoÎncă nu există evaluări
- Measles: Case Study: Hiro Landazuri Karla Gonzalez Jonathan ChenDocument12 paginiMeasles: Case Study: Hiro Landazuri Karla Gonzalez Jonathan ChenNicole Villanueva, BSN - Level 3AÎncă nu există evaluări
- Advisory 3 With Amendment - MR OPV SIADocument1 paginăAdvisory 3 With Amendment - MR OPV SIAD Alfz EinsTein JDÎncă nu există evaluări
- Nursing Practice II - Community Health Nursing and Care of The Mother and ChildDocument54 paginiNursing Practice II - Community Health Nursing and Care of The Mother and Childanon_840592833Încă nu există evaluări
- 3 GVAP Secretariat Report 2018 SAGE Oct 2018 PDFDocument149 pagini3 GVAP Secretariat Report 2018 SAGE Oct 2018 PDFJoshua SanchezÎncă nu există evaluări
- Oral Viral Infections Diagnosis and ManagementDocument13 paginiOral Viral Infections Diagnosis and ManagementhunarsandhuÎncă nu există evaluări
- PreConception Care 4 Student VersionDocument38 paginiPreConception Care 4 Student VersionKajal SinghÎncă nu există evaluări
- 1 s2.0 S0255085720315474 MainDocument6 pagini1 s2.0 S0255085720315474 MainLidwina ApyakaÎncă nu există evaluări
- TORCH Infections: ICU NursingDocument27 paginiTORCH Infections: ICU NursingLouis Carlos Roderos0% (1)
- Sample Chapter: Miscellaneous VirusesDocument7 paginiSample Chapter: Miscellaneous VirusesskÎncă nu există evaluări
- JanuariDocument19 paginiJanuariKlinik SalamahÎncă nu există evaluări
- CHN HandiesDocument23 paginiCHN HandiesFreeNursingNotesÎncă nu există evaluări
- Neu N TORCH Infections Clinics in Perinatology 2015Document27 paginiNeu N TORCH Infections Clinics in Perinatology 2015vickyÎncă nu există evaluări