Documente Academic
Documente Profesional
Documente Cultură
Coplications of Puerperium
Încărcat de
vijjimanthena9467Descriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Coplications of Puerperium
Încărcat de
vijjimanthena9467Drepturi de autor:
Formate disponibile
Seminar on
complications
of
Puerperium.
Submitted To: Submitted By:
Mrs. K.P. Sunandha, Ms.Mercy Parneetha. K.A
Asst. Professor, M.Sc (N) II year
Obstetric and gynaecological OBG Nursing,
Nursing Department, J.M.J College of Nursing.
J.M.J College of Nursing.
Name of the Guide : Mrs. K.P. Sunandha
Name of the Student : Ms. Mercy Parneetha. K.A.
Class : M.sc. (Nursing) II Year
Subject : Obstetrics and gynaecological nursing
Unit : IV
Name of the topic : Complication
Of Puerperium.
Group : M.Sc (N) Students
Place : M.Sc (N) Class room
Date : 27.02.2012
Time : 2:00pm to 4:00pm.
Method of Teaching : Lecture cum Discussion.
A. V aids : Black Board, Transparency, Power point, Pull chart,
Strip tease, Bulletin Board.
General Objectives:
By the end of the class, the students acquire in-depth knowledge
regarding the complications of puerperium, appreciate the physical and
physiological changes in puerperium and develop skills in taking care of the
mother with any of the complications.
Specific Objectives:
By the end of the class, the students will be able to
define puerperium.
describe the postpartum complications principles.
enumerate the most postpartum complications.
explain the postpartum complications.
Perineal Rupture
Uterine and Vaginal Rupture
Post Parturient Uterine Atony
Post Parturient straining
Bacterial Puerperal Infection
Postpartum Haemorrhage
Postpartum Endometritis
Postpartum Cardiomyopathy
Postpartum thyroiditis
Postpartum Depression.
Introduction:
The Postpartum period, also known as the puerperium, begins with the
delivery of the baby and placenta. The end of the Postpartum period is less well
defined, but is often considered the 6-8 weeks after delivery because the effects
of pregnancy on many systems have resolved by this time and these systems
have largely returned to their pre- pregnant state.
Health care providers should be aware of the medical and psychological
needs of the postpartum mothers and sensitive to cultural differences that
surround child birth.
Definition:
Puerperium- a period from the expulsion of the placenta until 6-8 weeks
after birth, during which time the uterus and other organs and systems
return to their pre pregnant state and lactation is initiated.
Many changes take place within the first 10-14 days.
Role changes.
(or)
Period of confinement during and just after birth
includes 6 subsequent weeks postpartum during which normal pregnancy
involution occurs.
(or)
Involution is the process whereby the genital organs revert back
approximately to the state as they were before pregnancy.
Duration:
Puerperium begins as soon as the placenta is expelled and lasts for
approximately 6 weeks when the uterus becomes regressed almost to the non-
pregnant size.
The period is arbitrarily divided into-
a) immediately within 7 days
b) early upto 6 weeks
c) remote- upto 6 weeks.
Postpartum Complications: Principles
The most frequent cause of postpartum hemorrhage is uterine atony.
Anything that over distends the uterus causes it to contract poorly or
overworks the uterus is a set-up for uterine atony.
Postpartum Complications
Most important postpartum complications
1. Perineal rupture
2. Retained placenta
3. Uterine prolapse
4. Uterine and vaginal rupture
5. Post parturient paraplegia
6. Post parturient uterine atony
7. Post parturient straining
8. Bacterial puerperal diseases
9. Puerperal intoxication
10. Puerperal infection
11. Septic metritis
12. Puerperal tetani
13. Puerperal vaginitis and vulvitis
1. Perineal Rupture
Causes :
1. Spontaneous, during the second stage of labor (vigorous straining)
2. Extreme traction of an oversized fetus
3. Predisposition include a hypoplastic vulva
Surgical correction:
1. Cleaning the perineal region
2. Light epidural anesthesia
3. Exposure the operative area by placing tension suture in the perineal skin
4. The free edge of the shelf is incised to a depth of 3 cm and extended laterally
and caudally on each side
5. Synthetic non-absorbable suture and a No. 2 or 3 half circle cutting edge
needle are used in the modified vertical suture pattern, starting at the deepest
part.
6. The two ends of each suture are left long (8 cm) and are tied together at their
ends to aid in identification of each knot during removal.
7. The suture must not penetrate the rectal mucosa.
8. The perineal skin is closed with vertical mattress suture.
2. Uterine and vaginal Rupture:
Causes
1. Prolonged dystocia with fetal emphysema
2. Uterine torsion
3. Improper manipulation and traction of the fetus
4. Forced traction of the fetus in abnormal p.p.p.
5. Fatigue of the operator
6. Poorly dilated cervix
7. Administration of oxytocin while the cervix is closed.
Treatment
In small uterine rupture
Repeated doses of oxytocin
Parental and intrauterine Antibiotic
Fluid therapy
Close observation of the client.
In large uterine rupture
o Suturing the uterus through the birth way
o Prolapsing the ruptured uterus and suturing it
o Suturing the uterus through laparotomy
3. Postparturient Uterine Atony
The uterus is abnormally large, roomy, flabby and without contraction directly
after birth
Causes:
Uterine inertia (primary and secondary)
Over-thinning of the uterus (twins, hydropsy)
Rupture of the uterus or cervix
Hypocalcaemia
Clinical findings:
- In rectal examination, the uterus found descended in the abdominal
cavity, the uterus lack any contraction and filled with lochia.
- The cervix is dilated with small amount of lochia discharged from the
vulva.
- Secondary retention of placenta
Treatment:
Oxytocin: 50-100 IU, within 24h after birth
Methergin: 5-10 mg i.m.
Calcium gluconate
Local and systemic antibiotic
4. Postparturient Straining
There is a persistent strong uterine birth pains for one or more day after birth
Causes:
There is irritant to the vagina or vulva
Long standing dystocia
Bleeding from the genital tract
Symptoms
The pains may persist for 4-7 days after birth
Continuous or intermittent straining, arched back, sunken eyes and
depression.
Frequent defection, diarrhea.
There is great tendency for prolapse of the vagina or rectum.
Uterine contractions are stronger
Treatment
+ General sedative
+ Epidural anesthesia
+ Local antibiotic within the uterus
+ Treat the original cause
5. Bacterial puerperal Infection
Disease: Puerperal bacterial intoxication
Cause: Saprophytic bacteria
Pathogenesis: Putrifaction of the uterine contents produces toxins which
absorbed through the uterine endometrium to circulate in the blood with
general intoxication.
Symptom: Fever, indigestion, exhaustion, little edema in the genital tract,
abnormal lochia
Treatment: Local antibiotic, Oxytocin, Siphoning the uterus, Supportive
treatment, Antihistaminic, Calcium gluconate, Systemic antibiotic, Epidural
Anesthesia.
Disease: Puerperal bacterial infection
Cause: Saprophytic bacteria
Pathogenesis: Bacterial activities are intensive. Bacteria tend to act locally
in the uterus
Symptom: Fever, Depression, edema of the soft birth way, abdomen is tense
Treatment: same treatment
Disease: Septic metritis
Cause: Coliform , Streptococci and Micrococcus
Pathogenesis: The difficult form of the non-specific Puerperal infection
Symptom: Fever, reddish watery vulval discharge, peritonitis, arthritis.
Treatment: same treatment.
Disease: Puerperal necrosis
Cause: Nechrophorum
Pathogenesis: Necrotic bacteria get entrance to the uterus from the cervix.
Symptom: General health disturbances, liver painful no palpation, the
mucus membrane is yellowish.
Treatment: Local and systemic Antibiotic, supportive treatment
Disease: Puerperal tetanus
Cause: Cl. tetani
Pathogenesis: m.o. enter the uterus through injury in the endometrium.
Symptom: Muscular cramps and stiffness.
Treatment: Anti-tetanic serum, supportive treatment.
Disease: vaginitis and vulvitis
Cause: Saprophytic Bacteria, Nechrophorum.
Pathogenesis: Narrow birth way result in trauma and laceration + m.o.
Symptom: Swollen vulva and vagina.
Treatment: Oily bland antiseptic Antibiotic, Epidural
Anesthesia.
6. Postpartum Hemorrhage
Obstetrical emergency that can follow vaginal or cesarean delivery
Incidence 3% of births
3
rd
most common cause of maternal death in US
Definition
Excessive bleeding that makes the patient symptomatic
(lightheaded, syncope) and/or results in signs of hypovolemia
(hypotension, tachycardia, oliguria)
(or)
A blood loss that exceeds 500 ml after a vaginal birth or 1,000ml
after a cesarean birth.
+ Early Postpartum Hemorrhage blood loss in the first 24 hrs after
childbirth.
+ Late Postpartum Hemorrhage occurs after the first 24 hrs.
Causes of Postpartum Hemorrhage
F Fo ou ur r T Ts s C Ca au us se e A Ap pp pr ro ox xi im ma at te e i in nc ci id de en nc ce e ( (% %) )
T To on ne e A At to on ni ic c u ut te er ru us s 7 70 0
T Tr ra au um ma a
L La ac ce er ra at ti io on ns s, ,
h he em ma at to om ma as s, ,
i in nv ve er rs si io on n, ,
r ru up pt tu ur re e
2 20 0
T Ti is ss su ue e
R Re et ta ai in ne ed d
t ti is ss su ue e, ,
i in nv va as si iv ve e
p pl la ac ce en nt ta a
1 10 0
T Th hr ro om mb bi in n C Co oa ag gu ul lo op pa at th hy y 1 1
Risk Factors
Prolonged 3
rd
stage of labor
Fibroids, placenta previa
Previous PPH
Over distended uterus
Episiotomy
Use of magnesium sulfate, preeclampsia
Induction or augmentation of labor
Management
Swift execution of a sequence of interventions with prompt assessment of
response
Initial steps
Fundal massage
ABCs, O2, IV access with 16g catheters
Infuse crystalloid; transfuse blood products as needed
Examine genital tract, inspect placenta, observe clotting
Give uterotonic drugs
Oxytocin 20 IU per L of NS
Methylergonovine (Methergine) 0.2mg IM q2-4h
Misoprostol 800 or 1000mg PR
Secondary steps
Will likely require regional or general anesthesia
Evaluate vagina and cervix for lacerations
Manually explore uterus
Treatment options
Repair lacerations with running locked absorbable suture
Tamponade
Arterial embolization
Laparotomy
uterine vessel ligation
Hysterectomy
Bimanual uterine compression massage is performed by placing one hand
in the vagina and pushing against the body of the uterus while the other
hand compresses the fundus from above through the abdominal wall. The
posterior aspect of the uterus is massaged with the abdominal hand and
the anterior aspect with the vaginal hand.
Preventive Measures
correcting anemia prior to delivery.
episiotomies only if necessary.
active management of third stage.
assess patient after completion of paper work to detect slow steady
bleeds.
Management of Postpartum Hemorrhage
7. Postpartum Endometritis
Infection of the deciduas (pregnancy endometrium)
Incidence
<3% after vaginal delivery
10-50% after cesarean delivery
5-15% after scheduled elective cesareans
Risk Factors
Prolonged labor, prolonged ROM, multiple vaginal exams, internal
monitors, maternal DM, manual removal of placenta, low
socioeconomic status.
Polymicrobial, ascending infection
Mixture of aerobes and anaerobes from genital tract.
Clinical manifestations (occur within 5 days pp)
Fever most common sign
Uterine tenderness
Foul lochia
Leukocytosis
Bacteremia in 10-20%, usually a single organism
Workup
CBC
Blood cultures
Urine culture
DNA probe / Chlamydia
Imaging studies if no response to adequate in 48-72h
CT scan abd/pelvis
US abd/pelvis
Treatment
Broad spectrum IV
Clindamycin 900mg IV q8h and
Gentamycin 1.5mg/kg IV q8h
Treat until afebrile for 24-48h and clinically improved; oral therapy
not necessary
Add ampicillin 2g IV q4h to regimen when not improving to cover
resistant enterococci
Prevention
prophylaxis for women undergoing C-section
Cefazolin 1-2g IV as single dose
8. Postpartum Thyroiditis
A variant form of Hashimotos thyroiditis occurring within 1 year after
parturition
Incidence 3-16% of postpartum women
Up to 25% in women with Type 1 DM
Thyroid inflammation damages follicles proteolysis of thyroglobulin
release of T3 + T4 TSH suppression.
Clinical manifestations
20-30%
Hyperthyroidism 2-4 mos pp, lasting 2-8 wks, followed by
hypothyroidism, lasting 2-8 wks, then recovery
20-40%
Hyperthyroidism only
40-50%
Hypothyroidism only, beginning 2-6 mos pp
Symptoms and signs, when present, are mild
Hyperthyroidism
Anxiety, weakness, irritability, palpitations, tachycardia,
tremor
Hypothyroidism
Lack of energy, sluggishness, dry skin
Diagnosis
Small, diffuse, nontender goiter or normal exam
High or high normal T3 + T4, low TSH, low radioiodine uptake
(hyper phase)
Low or low normal T4, high TSH (hypo phase)
65-85% have high antithyroid
Treatment
Most need no treatment.
Hyper: atenolol or propanolol
Avoid in nursing women
Hypo: levothyroxine 50-100 mcg qd for 8-12 wks.
Educate patient on sex, increased risk of developing
hypothyroidism or goiter, likely recurrence with subsequent
pregnancies
9. Postpartum Depression
Most common complication
Occurs in 13% (1 in 8) of women after pregnancy
Recurs in 1 in 4 with prior depression
Begins within 4 weeks after delivery
Multifactorial etiology
Rapid decline in hormones, genetic susceptibility, life stressors
Risk Factors
Prior h/o depression, family h/o mood disorders, stressful life
events
Pattern of sex are similar to other episodes of depression
Depressed mood, anxiety, loss of appetite, sleep disturbance,
fatigue, guilt, decreased concentration
Must be present most of the day nearly every day for 2 wks.
Screening
Edinburgh Postnatal Depression Scale
+ screen with score >/= 10
Check for anemia and thyroid disease
Differential Diagnosis
Baby Blues common, transient mood disturbance
Sadness, weeping, irritability, anxiety, and confusion
Occurs in 40 - 80% of postpartum women.
Postpartum psychosis
Psychiatric emergency due to risk of infanticide or suicide
Bizarre behavior, disorganization of thought, hallucinations,
delusions
usually occurs in first 2 weeks of pp
Treatment
Initiate at half the usual starting dose
Treat for at least 6 12 months after full remission to
prevent relapse
Sertraline or paroxetine for breast-feeding mothers
May also respond to psychotherapy
Hormonal therapy
Patient resources
National Womens Health Info Center (www.4woman.gov)
www.depressionafterdelivery.com
Blues:
Most common perinatal mood disturbance
Prevalence: 30-75%
Onset day 3 or 4
Mild, transient lasting hours to days
Resolve within 2 weeks
No treatment necessary
Postpartum Psychosis
Most rare and severe form of postpartum mood disorder
Prevalence: 0.01-0.02%
Onset: rapid, within 72 hours of birth, 95% of cases within 2 weeks
Treatment: Psychiatric Emergency, Psychiatrist treatment with
medication.
Postpartum Psychiatric Disorders
Disorder Prevalence Onset Duration Treatment
Blues 30-75% Day 3 or 4 Several days None
Postpartum
Depression
10 15% Within weeks Weeks
Months
Treatment by GP or psychiatrist usually required
Postpartum Psychosis 0.01
0.02%
Within 2
weeks
Weeks
months
Psychiatric emergency
Hospitalization required
Subinvolution of uterus:
Description
Incomplete involution or failure of the uterus to return to its normal
size and condition
Cause
Infection
Retained placenta fragments
Assessment
Uterine pain on palpation
Uterus is larger than expected
Fundus is higher in the abdomen
Greater than normal vaginal bleeding
Lochia does not follow normal pattern i.e.:
RUBRA SEROSA -- RUBRA
Backache
Leucorrhea if infection (white, creamy discharge)
Treatment
Methergin 0.2 mg Q3-4H PO for 24-48 hours
Antibiotics
Possibly D&C
Nursing interventions
Medications as ordered
Assessment of fundus
Safety and comfort needs
Mastitis:
Description
Inflammation of the breast as a result of infection
Primarily seen in breast-feeding mothers 2 to 4 weeks after
delivery
Cause
Staph aureus
Hemolytic strep
How it is transmitted:
Babys nose and throat
Mothers or health care providers hands
Cracked nipples
Assessment
Localized heat and swelling
Pain: redness, warmth and firm to touch with areas of lumpiness
Elevated temperature and chills
Tachycardia
Headache
Complaints of flu-like symptoms
Intervention:
Promote comfort of the client
Instruct mother in good hand-washing and breast hygiene
Apply heat to enhance inflammatory process (kill microbes)
Maintain lactation in breast-feeding mothers
Encourage manual expression of breast milk or use of breast pump
every 4 hours
REMEMBER, during EARLY stages of mastitis, the mother is
encouraged to breast-feed DIRECTLY
Encourage mother to support breasts with supportive bra
Administer analgesics as prescribed
Administer antibiotics as prescribed
Possibly I&D
Conclusion:
During pregnancy and Postpartum, changes occur in the circulating blood
volume, peripheral vascular compliance and resistance, myocardial function,
heart rate and the neuro hormonal system. These changes allow the
cardiovascular system to meet the increased metabolic changes demands of
pregnancy.
BIBLIOGRAPY:
+ Lowdermilk,perry and Bobak, maternity &womens health care, 6
th
edition, 1997, mosby, inc., st. Louis, missori, pg no: 358-367.
+ Donna L.Wong &Shannon E. Perry, maternal & child nursing care,
1998,Mosby, Inc, St.Louis,pg no546-574.
+ James DK, PJ steer & etal, High Risk pregnancy management, 2
nd
edition.2001, WB Saun ders, China, pg no. 667-687.
+ D.C Dutta, Text book of obstetrics including perinatology &
contraception, 6
th
edition, New central book agency, Pg no. 543-567.
+ Kamini Rao, Textbook of midwifery & obstetrics for nurses, 1
st
edition,
New Delhi,pg no.276-297.
+ Diane M. Fraber, Myles Text book for Midwives, 15 the edition, Elsevier
, pg no. 98-130.
+ www.encyclopedia.com
+ www.wikepedia.com
S-ar putea să vă placă și
- Augmentation and IOLDocument22 paginiAugmentation and IOLvani reddyÎncă nu există evaluări
- Term PaperDocument85 paginiTerm PaperAbhilash PaulÎncă nu există evaluări
- Uterine Malformations PDFDocument6 paginiUterine Malformations PDFsaritha OrugantiÎncă nu există evaluări
- Thrombo Embolism and PregnancyDocument9 paginiThrombo Embolism and Pregnancysangeetha francisÎncă nu există evaluări
- Seminar Drug.... Mohan.sDocument28 paginiSeminar Drug.... Mohan.smOHAN.S0% (1)
- (Augmentation) Medical and SurgicalDocument17 pagini(Augmentation) Medical and SurgicalNadiya RashidÎncă nu există evaluări
- Clinical Speciality SeminarDocument26 paginiClinical Speciality Seminarakanksha100% (1)
- Obg Res - PartographDocument20 paginiObg Res - Partographmohapatra dev100% (1)
- (11-13) Assess The Knowledge On Minor Ailments of Pregnancy-FormatDocument3 pagini(11-13) Assess The Knowledge On Minor Ailments of Pregnancy-FormatMudasir Ahmad BhatÎncă nu există evaluări
- 5.theories and Models of MidwiferyDocument29 pagini5.theories and Models of MidwiferyRatna KumariÎncă nu există evaluări
- Hormonal CycleDocument20 paginiHormonal CycleGunaÎncă nu există evaluări
- Anemia PregnancyمحاضرةDocument33 paginiAnemia PregnancyمحاضرةSamia Abu AishiaÎncă nu există evaluări
- Term Paper 2nd YearDocument83 paginiTerm Paper 2nd YearJomy Suneesh100% (1)
- Seminar MenopauseDocument51 paginiSeminar MenopauseKelvin SuÎncă nu există evaluări
- Lesson Plan On Epilepsy in PregnancyDocument17 paginiLesson Plan On Epilepsy in PregnancyRajaÎncă nu există evaluări
- Ovarian CystDocument3 paginiOvarian Cystpooja singhÎncă nu există evaluări
- Legislations Clinical Rights and Professional ResponsibilityDocument10 paginiLegislations Clinical Rights and Professional ResponsibilityFarheen khanÎncă nu există evaluări
- M.M. College of Nursing: Assignment ON Mild, Moderate and Severe Pre-EclampsiaDocument4 paginiM.M. College of Nursing: Assignment ON Mild, Moderate and Severe Pre-EclampsiaNadiya RashidÎncă nu există evaluări
- Seminar On Obstetrical EmergencieDocument21 paginiSeminar On Obstetrical EmergencieJyothi RameshÎncă nu există evaluări
- Obstetrics & Gynaecology NursingDocument15 paginiObstetrics & Gynaecology Nursingyola listantiaÎncă nu există evaluări
- Independent Nurse PractitionerDocument14 paginiIndependent Nurse PractitionerKarishma Shroff100% (1)
- Welcome To The Morning SessionDocument20 paginiWelcome To The Morning SessionGENERAL sharpÎncă nu există evaluări
- National College of Nursing: Procedure ONDocument6 paginiNational College of Nursing: Procedure ONSumit Yadav100% (1)
- Iec Obg CareDocument16 paginiIec Obg CareBlessy Madhuri100% (1)
- MANAGEMENT OF 3rd AND 4th STAGEDocument18 paginiMANAGEMENT OF 3rd AND 4th STAGENidhi Sharma100% (1)
- Cardio Vascular Disease in PregnancyDocument57 paginiCardio Vascular Disease in PregnancySanthosh.S.U0% (1)
- LabourDocument39 paginiLabourSravanthi Karingula100% (1)
- Prevention of Mother To Child Transmission of HivDocument17 paginiPrevention of Mother To Child Transmission of Hivfiraol mokonnenÎncă nu există evaluări
- Antepartum HaemorrhageDocument18 paginiAntepartum HaemorrhageOjambo Flavia100% (1)
- Genital Tract InjuriesDocument24 paginiGenital Tract InjuriesManisha ThakurÎncă nu există evaluări
- Obg Sem by Padmashree Institute of NursingDocument26 paginiObg Sem by Padmashree Institute of NursingmOHAN.S100% (1)
- 7.recent Advances in Contraceptive TechnologyDocument25 pagini7.recent Advances in Contraceptive TechnologyVeena Dalmeida100% (1)
- Forceps DeliveryDocument7 paginiForceps DeliveryJemin KimÎncă nu există evaluări
- Preventive Obstetrics PDFDocument25 paginiPreventive Obstetrics PDFAnju MargaretÎncă nu există evaluări
- Hormonal Cycle Lesson PlanDocument9 paginiHormonal Cycle Lesson PlanGunaÎncă nu există evaluări
- Handouts OBSTETRICS EMERGENCYDocument9 paginiHandouts OBSTETRICS EMERGENCYAshish GuptaÎncă nu există evaluări
- Postterm PregnancyDocument16 paginiPostterm PregnancyrranindyaprabasaryÎncă nu există evaluări
- "Behold, Children Are A Heritage From The Lord, The Fruit of The Womb Is A Reward". - King DavidDocument16 pagini"Behold, Children Are A Heritage From The Lord, The Fruit of The Womb Is A Reward". - King DavidInternational Journal of Innovative Science and Research TechnologyÎncă nu există evaluări
- 001hypertensive Disorders in Pregnancy PDFDocument23 pagini001hypertensive Disorders in Pregnancy PDFRosechelle Bas SamsonÎncă nu există evaluări
- Abortion SeminarDocument16 paginiAbortion SeminarAjit M Prasad Prasad100% (2)
- Abnormal Uterine ActionDocument36 paginiAbnormal Uterine ActionMed PoxÎncă nu există evaluări
- AbortionDocument66 paginiAbortionGunu SinghÎncă nu există evaluări
- Multiple Pregnancy: Presented byDocument49 paginiMultiple Pregnancy: Presented byvarshasharma05Încă nu există evaluări
- Assignment 2Document76 paginiAssignment 2A Noor Ahmad100% (1)
- PuerperiumDocument12 paginiPuerperiumWesam Al-TawilÎncă nu există evaluări
- Obg Ward Teaching Infection ControlDocument37 paginiObg Ward Teaching Infection ControlbhavanaÎncă nu există evaluări
- Uterine Malformations PDFDocument6 paginiUterine Malformations PDFsaritha OrugantiÎncă nu există evaluări
- Conyent Physiology of Third Stage of LabourDocument13 paginiConyent Physiology of Third Stage of LabourJay PaulÎncă nu există evaluări
- Obgyn Anemia in Pregnancy For UG ClassDocument35 paginiObgyn Anemia in Pregnancy For UG ClassMunirathna ChandruÎncă nu există evaluări
- O@g Maternal and Fetal Mesures ContentDocument22 paginiO@g Maternal and Fetal Mesures Contentjeya maniÎncă nu există evaluări
- Iec Obg CareDocument18 paginiIec Obg Carenaga mani100% (1)
- L T College of Nursing SNDT University Churchgate Lesson Plan On Nursing Care of A Patient With Menstrual DisordersDocument13 paginiL T College of Nursing SNDT University Churchgate Lesson Plan On Nursing Care of A Patient With Menstrual DisordersPriyanka NilewarÎncă nu există evaluări
- OBG ARTICLES ANUM NooriDocument22 paginiOBG ARTICLES ANUM NooriVaishali SinghÎncă nu există evaluări
- Perspective of Nursing Education Global and National: By: Sardi Middle East University KuwaitDocument40 paginiPerspective of Nursing Education Global and National: By: Sardi Middle East University KuwaitMohanraj MohanrajÎncă nu există evaluări
- The Third StageDocument7 paginiThe Third Stagebalaramani6890Încă nu există evaluări
- Genetics and TeratologyDocument31 paginiGenetics and Teratologypandem soniyaÎncă nu există evaluări
- Minor AilmentsDocument14 paginiMinor AilmentsGazala100% (1)
- All India Institute of Medical Sciences Jodhpur College of Nursing Practice Teaching ONDocument12 paginiAll India Institute of Medical Sciences Jodhpur College of Nursing Practice Teaching ONFarheen khanÎncă nu există evaluări
- Fetal Physiological Measurements: Proceedings of the Second International Conference on Fetal and Neonatal Physiological MeasurementsDe la EverandFetal Physiological Measurements: Proceedings of the Second International Conference on Fetal and Neonatal Physiological MeasurementsPeter RolfeÎncă nu există evaluări
- Food Crisis in The World !Document6 paginiFood Crisis in The World !ChrissBright E. HermanÎncă nu există evaluări
- Holi With Natural ColoursDocument1 paginăHoli With Natural Coloursankush014Încă nu există evaluări
- Final Test RESIT 61 TNDocument4 paginiFinal Test RESIT 61 TNosamyyÎncă nu există evaluări
- Surgery Toacs APRIL 2012: Hassaan Bari Aga Khan UniversityDocument18 paginiSurgery Toacs APRIL 2012: Hassaan Bari Aga Khan UniversitySyedÎncă nu există evaluări
- Disability EssayDocument7 paginiDisability Essayapi-459529771Încă nu există evaluări
- Budget Justification Fy2021Document418 paginiBudget Justification Fy2021Lisa FabianÎncă nu există evaluări
- Child Protection Training ManualDocument229 paginiChild Protection Training Manualbabuin1Încă nu există evaluări
- Probiotics, Prebiotics and The Gut Microbiota: Ilsi Europe Concise Monograph SeriesDocument40 paginiProbiotics, Prebiotics and The Gut Microbiota: Ilsi Europe Concise Monograph Seriesjimmy7forever100% (1)
- Veterinary Internal Medicne - 2008 - Bruchim - Heat Stroke in Dogs A Retrospective Study of 54 Cases 1999 2004 andDocument9 paginiVeterinary Internal Medicne - 2008 - Bruchim - Heat Stroke in Dogs A Retrospective Study of 54 Cases 1999 2004 andGuillermo MuzasÎncă nu există evaluări
- Sitogenetika Dan Peranannya Dalam Keganasan Hematologi: ResearchDocument23 paginiSitogenetika Dan Peranannya Dalam Keganasan Hematologi: ResearchFebryanti Priskila SilaenÎncă nu există evaluări
- Cardiovascular Risk Factors in Airline PilotsDocument4 paginiCardiovascular Risk Factors in Airline Pilotsluis11256Încă nu există evaluări
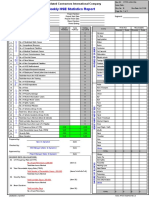
- Hse Statistics Report Pp701 Hse f04 Rev.bDocument1 paginăHse Statistics Report Pp701 Hse f04 Rev.bMohamed Mouner100% (1)
- ReferensiDocument2 paginiReferensiYuanita RosalinaÎncă nu există evaluări
- Do No Harm by Henry Marsh ExtractDocument15 paginiDo No Harm by Henry Marsh ExtractAyu Hutami SyarifÎncă nu există evaluări
- Renal Pharmacology 2023Document116 paginiRenal Pharmacology 2023sami MesfinÎncă nu există evaluări
- Over PopulationDocument60 paginiOver PopulationSpencer VenableÎncă nu există evaluări
- Important Classifications PDFDocument42 paginiImportant Classifications PDF330 Himank MehtaÎncă nu există evaluări
- Full Download Test Bank For Ebersole and Hess Gerontological Nursing and Healthy Aging 2nd Canadian Edition by Touhy PDF Full ChapterDocument36 paginiFull Download Test Bank For Ebersole and Hess Gerontological Nursing and Healthy Aging 2nd Canadian Edition by Touhy PDF Full Chapteradrianblackiadxetkrqm100% (15)
- Adams4e Tif Ch47Document19 paginiAdams4e Tif Ch47fbernis1480_11022046100% (1)
- Book 28Document56 paginiBook 28Er Sana WarsiÎncă nu există evaluări
- Abreviaciones ChatDocument4 paginiAbreviaciones ChatrojarodÎncă nu există evaluări
- Excretory Products and Their EliminationDocument6 paginiExcretory Products and Their Eliminationkanth3012Încă nu există evaluări
- Cardiovascular Responses To An Isometric Handgrip Exercise in Females With PrehypertensionDocument7 paginiCardiovascular Responses To An Isometric Handgrip Exercise in Females With PrehypertensionGuilherme LimaÎncă nu există evaluări
- Icru Report 62Document62 paginiIcru Report 62Luis Ramirez100% (1)
- Cassey Ho - PIIT 2.0Document45 paginiCassey Ho - PIIT 2.0Nikolett Mészáros100% (14)
- Rickey Dixon Letter To The Court On NFL Concussion Settlement FeesDocument9 paginiRickey Dixon Letter To The Court On NFL Concussion Settlement FeesRobert Lee100% (1)
- PCT For BodybuildersDocument12 paginiPCT For BodybuildersJon Mester100% (4)
- Science: Quarter 1 - Module 1: Week 1-2Document31 paginiScience: Quarter 1 - Module 1: Week 1-2Kirt Dimamay HilarioÎncă nu există evaluări
- Efficacy of Doctorvox On Mutational FalsettoDocument8 paginiEfficacy of Doctorvox On Mutational FalsettoANA CRISTINA MENDEZ DIAZÎncă nu există evaluări
- Pediatrics - Hesi Practice ExamDocument10 paginiPediatrics - Hesi Practice ExamWizzardÎncă nu există evaluări