Documente Academic
Documente Profesional
Documente Cultură
Micro Final Notes
Încărcat de
Sarah PlunkettDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Micro Final Notes
Încărcat de
Sarah PlunkettDrepturi de autor:
Formate disponibile
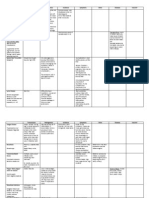
I. Respiratory Infections Unit 6. Major Infections Bonanza Accompanies Ch. 21 A. RESPIRATORY ANATOMY 1.
Upper respiratory tract throat and up a. Sinuses: several pairs, around eyes and nose b. Pharynx: nasal cavity and space behind mouth c. Larynx: voice box d. Trachea :in front of esophagus, hard and ringed Lower respiratory tract a. Bronchi branching tubes to lungs b. Alveoli tiny pockets in lungs, site of gas exchange with blood Connection to ears Eustachian tubes from inner ear to pharynx: mucus can back up into them, carrying pathogens that may cause ear infections Unique Defenses as compared to the non-unique defenses like mucosal layer, lymph nodes, epithelia a. Saliva contains lysozyme, other antibacterial factors b. Alveolar macrophages c. Mucociliary escalator cilia in bronchi and trachea push mucus up toward mouth and nose, along with any pathogens it contains
2.
3. 4.
B. GENERAL PRINCIPLES 1. 75-80% U.S. acute infections are URTI or LRTI a. Majority are viral b. Seasonality Worse in cold weather, because proteins slower to denature (and people spend more time in tight quarters). Cold doesnt make you sick! 1. Symptoms coughing, sneezing, stuffiness, LRTI: wheezing, rattle, fatigue, fever. -pnea = breathing (dyspnea, apnea) Treatment Abx for bacterial; rest for viral. Color of sputum/mucus may help (yellow/green = more often bacterial).
3.
C. UPPER RESPIRATORY TRACT INFECTIONS Group A Strep (GAS): S. pyogenes Alpha-hemolyticcan digest RBCs. Transmission: Contact Droplet precautions! a. Diseases Strep throat painful, burning, white patches on back of throat/tonsils Scarlet fever potential complication of strep throat due to exotoxin in blood Full body rash, high fever nd Rheumatic fever Auto-immune complication from 2 or later exposure: antibodies to strep cross-react with self-antigens on the heart and/or joints: congestive heart failure, joint pain a. Pathogenesis Capsule, hyaluronidase, streptolysins kill phagocytes that eat them. Can do antigenic variation. Has toxins that can cause toxic shock syndrome. 2. Corynebacterium diphtheriae a. Chinese-letter pattern describes smear appearance due to binary fission process called snapping b. Transmission: contact Droplet precautions! c. Pathogenesis Diphtheria toxin = exotoxin that inhibits eukaryotic translation, killing cells. Dead cells build up in pharynx and may slough off/block airways. If toxin gets into blood, may cause death. d. Incidence: very rare in US (DTaP vaccine) D in DTaP (kids) or Tdap = adult booster e. USSR: serious spike after vax stopped during chaos @Cold War End 1.
3.
Parainfluenza virus (HPIV1-4) a. Transmission: contact Droplet precautions! b. Croup, laryngitis, bronchitis, others Croup = dry, barking cough common in infants. May develop into bronchitis or pneumonia. The younger the patient, the worse the symptoms. a. Serotypes 1-4 shares common evolutionary ancestor with influenza, and like influenza has antigenic shift and drift. Serotypes are defined by whether Abs cross-recognize them: if Abs in ELISA bind to one HPIV but not another, they must be different serotypes. Some serotypes worse than others. Common cold a. Transmission: contact b. Symptoms Coughing, congestion, headaches from sinus pressure. No fever. If fever, infection is more serious. c. Rhinovirus, Coronavirus, Adenovirus Three groups of virus cause the vast majority of common colds. No treatment is available. Prevention is the best medicine. Protect others by coughing/sneezing into a tissue or your elbow instead of your hands, which can infect others via handshakes or fomites. d. Others usually bacterial Most URTIs are viral, but these are more often bacterial: e. Acute sinusitis 1. Secondary to cold (why?) Presumably because the immune system is distracted by the common cold, and because bacteria with the right VFs survive well in the mucus. 2. Often caused by other resp. tract pathogens i.e. those that can progress to laryngitis, pneumonia. So important to treat sinusitis! f. Otitis media infections of the middle ear via Eustachian tube. Diagnosed by inflamed eardrum. More common in young children b/c E. tubes are shorter. Meningitis link Important to treat because many of the otitis pathogens can also progress to meningitis. a. Transmission: contact
4.
D. LOWER RESPIRATORY TRACT INFECTIONS 1. Pneumonia Lung infection i. General a. Transmission: contact droplet precautions! b. 100+ organisms cause c. Symptoms Usual: rattling in chest, shortness of breath, fever, chest pain, wet, thick mucus on coughing, white stuff on X-ray ii. Community-Acquired (CA) vs nosocomial a. Most common: Streptococcus pneumoniae (pneumococcus) The pneumococcus is one of three special cocci, and is not significantly related (by evolution) to the other two. Unlike Strep pyogenes (GAS) is gamma-hemolytic (does not degrade RBCs at all), but causes several diseases, including otitis, meningitis, pneumonia). Vaccine. b. 20% are viral: usually 1. Influenza, HPIV Soon to be discussed or already done 2. Respiratory syncytial virus (RSV) coming up iii. Atypical pneumonia also called walking pneumonia, common and less serious. a. Mild, no sputum b. Caused by obligate intracellular pathogens Their virulence strategy is to hide inside alveolar cells. 1. Chlamydophila pneumoniae (text incorrectly identifies genus as Chlamydia) Dont confuse with the evolutionarily related STD! Survives phagocytosis by alveolar macrophages and replicates in phagosome.
iv.
Mycoplasma pneumoniae: children Mycoplasma is super-tiny and lacks a cell wall. Lives in bronchial/alveolar epithelia. Hospital-Acquired (HA) Pneumonia nosocomial a. Can be any of above eg pnuemococcus, Chlamydophila, but often bacteria in wrong place 1. GI residents, eg Enterobacter, Pseudomonas From fecal contamination of LRTI 2. Skin residents, eg Staphylococcus aureus (w/ MRSA) From skin contamination of LRTI. Especially dangerous if MRSA. b. Who gets it, when Mostly elderly patients already sick, especially if on ventilator and/or Abx that compromise normal flora
2.
2.
Mycobacterium tuberculosis acid-fast a. Transmission: contact, aerosol mycolic acid gives exceptionally long stability on surfaces, can be transmitted through air ducts. Airborne precautions! b. Pathogenesis i. Mycolic acid: protects from many Abx, drying ii. Lives in macrophages, slow-growing survives phagocytosis and lives in phagosome, dividing only occasionally. Tubercles in lungs = masses of infected macrophages, some of which may die and calcify (obvious on X-ray). Tubercles can last for decades and may obstruct airways c. TB symptoms Bloody cough, trouble breathing. May disseminate to GI, brain, fetus. Asymptomatic (95%) Symptoms usually only develop in immunocompromised, but transmission may still occur Primary TB initial exposure: bacteria set up tubercles and infection may progress if immunity is weak. Secondary TB reactivation of tubercles due to immune compromise Effect of Rx consistent Abx treatment for 6-24 months required to eradicate. Tx very unlikely during treatment a. TB Test: Inject TB Ag just under the skin. If person has antibodies, inflammation will occur within a couple days. Its like an ELISA in the skin! But cant distinguish reliably between past and present infections: chest X-ray needed for that. b. TB Vaccine: exists, but low efficacy (<70%), and not given because would guarantee positive TB tests c. Incidence: 1/3 world! Why? Was declining, but two factors caused the comeback: 1) HIV/AIDS; 2) USSR collapse underfunded Russian prisons were riddled with TB and couldnt afford drugs, so they cut pills in half for prisoners MDR strains. d. Directly Observed Therapy (DOT) The gold standard. Requires that treatment be administered directly by trained health care worker so as to prevent more MDR. Influenza a. Transmission: Contact Droplet precautions! b. Disease NOT vomiting and diarrhea (though that may happen in ~10% cases). Mainly fever, achiness, fatigue, cough c. A,B,C serotypes A = pandemics; B = regional epidmics; C = very mild, usually not a problem. Dont remember serotype? Look it up! d. Host range very broadmany mammals and birds. Key species for human problems = pigs, chickens, humans. Factory farms here and close living quarters in other countries create opportunities for Ag shift. e. Viral receptors the main recipients of shift, since they are exposed to Abs a. Hemagglutinin (HA) b. Neuramidinase (NA) f. H/N Strains Monitoring and banking of H/N combinations is used for surveillance and for deciding what goes in the annual vaccine g. On February 23, 2012 the World Health Organization (WHO) recommended that the Northern Hemisphere's 2012-2013 seasonal influenza vaccine contain the following three vaccine viruses: a. an A/California/7/2009 (H1N1)pdm09-like virus; b. an A/Victoria/361/2011 (H3N2)-like virus; c. a B/Wisconsin/1/2010-like virus (from the B/Yamagata lineage of viruses).
3.
h.
Pandemics frequent b/c of high antigenic shift frequencyherd immunity never possible to achieve a. 1918 Worst by far, but probably wouldnt be as bad today. We made the mistake of transporting itvia WWI, in planes, trains and later hospitals, where infected and uninfected patients were packed together. Similar mutations have arisen since and never get far, because their hosts are quickly quarantined and treated. b. Avian Flu (H5N1) 50% + mortality in humans, but so far can only spread chickens humans. Cases on map at right. Current controversy: European scientists recently made a human human strain in the lab: should they publish how it was made? Read the news. c. H1N1 flu (2009) Recent pandemic traced back to pig factory farms, where high population density favors development of virulent disease.
4.
Respiratory Syncytial Virus (RSV) a. Transmission: Contact Droplet precautions. b. Pathogenesis Causes alveolar and bronchial cells to fuse and form syncytia, which results in lower gas exhange abilities, alveolar collapse c. Disease Hypoxia and retention of CO2 difficulty breathing, death d. SIDS link Likely responsible for some cases of SIDS, especially with secondary factors like tobacco smoke exposure Whooping Cough a. Transmission: Contact Droplet precautions b. Bordetella pertussis Bacterium that causes it. c. Pathogenesis Pertussis toxin, destroys cilia of respiratory tract. Mucus collects in lungs. d. Disease Congestion, sneezing progresses over 1-2 weeks to paroxysmal coughing and apnea (inability to breathe), exhaustion, death possible e. Incidence: rare but rising (DTaP, Tdap) Legionairres Disease lung bacterium a. Transmission: Aerosol b. Legionella pneumophila. c. Obligate intracellular Very difficult to culture, fastidious. d. Amoebas In the environment, free-living, harmless amoebas act as a reservoir. They must be inhaled for infection to occur. You must inhale in spray to become infected. Air conditioning units, showerheads and produce sprays at groceries have all been implicated. e. Symptoms Usually only in immunocompromised people. Severe pneumonia with high fever high mortality rate (15-50% of those with symptoms) Hantavirus Pulmonary Syndrome (HPS) a. Transmission: aerosol Specifically, aerosolized urine or feces from infected rodents (reservoir) b. Sin Nombre virus, Asia Prior to 1990s, hantaviruses only found in East Asia. Outbreak in Navajo Nation in 1994 led to discovery of new hantavirus, now called Sin Nombre. Cases are sporadic today, mainly in W/SW US. c. Epidemiology Tends to arise at newly dispersed suburban edges, especially with those storing food d. Symptoms Sudden flu-like symptoms, lungs fill with fluid, high mortality rates Q Fever a. Transmission: aerosol From aerosolized sheep placenta/fetuses. Causes spontaneous abortion to facilitate its transmission among herd animals. b. Coxiella burnetii Endospores, so can survive long after remains have decayed c. Obligate intracellular bacteria hard to culture d. Goats, sheep Most common in those with frequent contact with these animals e. Symptoms f. Q Fever Flu-like symptoms, chills, cough
5.
6.
7.
8.
g. 9.
Abortion can cause fetal death in humans
Inhalation Anthrax a. Transmission: aerosol inhaled endospores. Human to human transmission not demonstrated, but droplet precautions still recommended. b. Bacillus anthracis Common in soil, but has high ID50, plus must be inhaled for serious disease. Thus, very rare. c. Symptoms Mild, until anthrax toxin accumulates sufficiently to kill many alveolar cells cyanosis, death. Prophylactic Abx recd for possible exposures. d. Bioterrorism Endospores and non-obvious pathology make it attractive, but would require high degree of training and production facility for significant dispersal. Still, big deal on the NCLEX.
E. FUNGAL INFECTIONS General principles 1. Primarily immuno-compromised 2. LRTIs Can see hyphae on X-ray 3. Pneumocystis carinii Pneumonia (PCP) Very common in AIDS patients 4. Transmission: aerosol (at least) Maybe also droplet 5. Symptoms Mild pnuemonitis, dry caugh, but progressive inability to breath (dyspnea) and pneumonia. Hypoxia, death. 6. HIV Most patients with PCP have HIV. Significant decline now that HAART is available. 7. Others to review from Unit I a. Histoplasmosis b. Coccidiomycosis c. Aspergillosis II. Digestive Infections A. DIGESTIVE ANATOMY 1. GI Tract a. Mouth Teeth, tongue, gums, salivary glands b. Esophagus Behind trachea c. Stomach pH 2 d. Small Intestine long; absorbs nutrients e. Large Intestine (Colon) shorter, regulates water balance f. Rectum, anus Accessory Organs i. Liver i. Functions: Detox blood, make bile (emulsifies fat), make complement. Has Kupffer cells (macrophages) i. Hepatic portal system blood from GI capillaries collects into hepatic portal vein that enters liver capillary beds for detox of anything that entered through mouth, then blood exits through hepatic vein to re-enter general systemic circulation ii. Pancreas exocrine function: makes essential digestive enzymes for small intestine; endocrine function: makes insulin for blood iii. Gall Bladder stores bile made by liver, empties to small intestine after meal
2.
B. GENERAL PRINCIPLES 1. Common symptoms a. Gastritis, enteritis, gastroenteritis vomiting, diarrhea. Only danger = dehydration. b. Dysentery blood in stool: dangerous because of possible ulcers, sepsis. c. Enteric fever systemic infection originating from GI, with fever and abdominal pain Food poisoning common problem related to consuming a pathogen, usually in undercooked meat or unwashed vegetables. Many viruses, bacteria and protozoa can cause. Hand washing after toilet is for the protection of others from fecal-oral pathgoens, not yourself. (Although it can be a good time to get droplet-borne pathogens off your hands!) Endogenous vs exogenous endogenous pathogens are normal commensals gone bad due to immune compromise or imbalance (eg one created by antibiotics). Exogenous = enter body from outside, usually primary pathogens Common treatments a. Supportive therapy ORT = oral rehydration therapy; IV rehydration for more serious cases. Water plus salt/sugar. b. Metronidazole Often used for bacterial/protozoan infections because it targets anaerobic metabolism
2. 3. 4. 5.
C. ORAL INFECTIONS 1. Mouth bacteria a. Plaque: a multispecies cooperative A biofilm. Brushing and flossing disrupts it physically and is important to do daily. b. Streptococcus spp. Major components in the biofilm, especially in its initiation. Their capsules can help start the slime layer. Most are harmless, but S. pyogenes, S pneumoniae are not, and some others cause cavities. c. Saliva Contains IgA, lysozyme, and more. Protects against many microbes, but not perfect, especially vs biofilms. Dental caries aka cavities a. Acid on pellicle Several organisms ferment sugars into acid. This acid breaks down the pellicle. If hole grows deep enough, other bacteria can colonize the pulp of the tooth, bone or worse b. Sugar The more simple sugars in your diet, the more acid can be produced. c. S. mutans most common association with cavities, very slimy! But multiple species always present. Gingivitis inflammation of the gum surfaces. Periodontitis Inflammation of the deeper gums. May infect bone teeth fall out. Genetic predisposition Some people are more likely to host S. mutans and friends.
2.
3. 4. 5.
D. GI INFECTIONS 1. Stomach ulcers Inflamed stomach lining breaks down until it bleeds a. Transmission: unknown Mysterious because H. pylori cannot survive outside the body. 50%+ adults are infected b. Helicobacter pylori A microaerophile and acidophile, this spiral bacterium is perfectly adapted for the stomach. c. Symptoms Abdominal pain, nausea, anorexia, possible internal hemorrhage d. Pathogenesis i. Development Many infected, but illness only starts with immune compromise and/or stress. Mucus declines, and stomach lining harmed by own acid. ii. Virulence factors Catabolizes proteins, then uses urease to make ammonia from the amino acids. This raises pH in and around bacterium. Have receptors to stick to stomach cells and block mucus formation.
2.
Enterobacteriaceae Gram negative rods found in GI a. General characteristics i. Transmission: fecal-oral ii. Facultative anaerobes iii. Most are opportunists i.e., endogenous a. Exceptions: true pathogens Shigella, Salmonella b. All cause disease in other parts of body e.g. respiratory tract, urinary tract, vagina, wounds iv. Coliforms vs non-coliforms Coliforms = normal fecal bacteria, ferment lactose. Non-coliforms = pathogens, do not ferment lactose i. O, K, H antigens: O is sugar part of LPS; K is capsule sugars, and H are flagellar proteins. Differences in these are used to distinguish serotypes. i. Virulence a. Secretion systems on pathogenicity islands P. islands encode multiple proteins that assemble into tiny needles that inject virulence factors into cells. So they live extracellularly, but influence host cells kind of like a virus might. b. Enterotoxins family of exotoxins released by some of these bugs. Cause salt channels to open on cells, leading to salt efflux water efflux diarrhea a. Escherichia coli i. Most strains = mutualists Make vitamin K, help digest food ii. Strain virulence determined by exchangeable genes Genes that increase virulence are on plasmids or pathogenecity islands, so normal E. coli may be transformed or transduced or conjugated into meaner bugs. iii. Many toxins, including Shiga toxin Made by various members of this species. Shiga toxin = cytotoxin. Blocks eukaryotic cell protein synthesis. iv. Pathogenic strains a. Enterotoxigenic E. coli (ETEC) Common cause of travellers diarrhea (rarely serious save in infants) b. Enteropathogenic E. coli (EPEC) fimbriae aid attachment to cells and degrade microvilli. Mainly seen in bottle-fed infants. c. Enterohemorrhagic E. coli (EHEC), O157:H7 Shiga toxin producers. Very low ID 50. Epidemics in various foods. Serious degradation of microvilli hemorrhaging and death. d. Others other strains exist b. Shigellosis i. Four Shigella species primary pathogens ii. ID50 very low! 1-10 organisms for worst species iii. Symptoms range in severity by species from diarrhea dysentery iv. Pathogenesis a. Shiga toxin they are E. coli cousins. E. coli may have gotten it from them. b. Intracellular motility / spread (see figure in book) live inside of host cells and run around in cytoplasm until they hit plasma membrane, forming protrusions into neighboring cells. Thus, can spread from cell to cell without exposure to humoral immunity. c. Salmonella enterica primary pathogens i. Strain diversity Once were multiple species but are now considered one species with multiple serotypes. ii. Gastroenteritis caused by S. enterica serotype Enteridis. (Book = error) Common cause of food poisoning a. Complications 1. Bacteremia seen mainly in immunocompromised: blood and bone infections 2. Enteric fever chronic infection of lymphatic organs and bone b. Virulence Invade the GALT via phagocytic cells lining intestine c. Chickens can be transovarially transmitted in chickens, so raw eggs can be vehicle iii. Typhoid fever caused by Salmonella entrica subtype Typhi
a. b. c. 3.
Pathogenesis Lives in GI macrophages that travel to lymph nodes and, on dying, release bacteria to infect more MFs. LPS released into lymphatic fluid each time. Disease Fever, gastroenteritis Vaccine For travellers from northern world to southern. But requires booster every two years.
C. diff. Major hospital problem a. Clostridium difficile endospores, obligate anaerobe. Infants are a reservoir due to diet and no effect of exotoxins on immature guts a. Pathogenesis endospore enters your GI and usually is outcompeted by commensalsunless they are absent due to Abx. Also, survives long time in environment. Produce cytotoxin and enterotoxin. b. Disease i. Enteritis sulfurous diarrhea ii. Enteric hemorrhage if enough cells die, mucosa may ulcerate 55 Cholera a. b. c. d. e. f.
4.
Vibrio cholerae C-shaped bug Alkaline freshwater acts as resevoir Endemicity South Asia and ssAfrica have regular cases during rainy seasons Epidemics Occur wherever large numbers of people live densely w/o good sewage treatment. Pathogenesis Cholera toxin causes rapid salt and water loss into the bowel lumen Symptoms Very intense diarrhea, rice water stool, severe abdominal pain
5.
Campylobacter jejuni a. Enteritis Very common cause, especially from undercooked meat b. Reservoir pets, livestock c. Guillain Barre Syndrome? GBS = unknown cause and possibly multiple causes, but C. jejuni highly associated with onset of symptoms Rotavirus a. 40-60% of gastroenteritis b. Major cause of infant death worldwide c. Pathogenesis: kills microvilli cells, resulting in inflammation and decreased nutrient absorption. Fats malabsorbed d. dsRNA virus the only one of human clinical importance e. Vaccine standard childhood vaccine Enterovirus a. Large family, including polio, coxsackie, more Start in GI but may move elsewhere b. Often spread to other organs/systems, including nervous, cardiac No treatment known Listeriosis A form of food poisoning, high ID50 a. Listeria monocytogenes b. Pathogenesis Similar to Shigella: live inside of cells and spread intercellularly. May travel in WBCs to other parts of the body. c. Diseases i. Enteritis in healthy people ii. Meningitis in immunocompromised people iii. Fetuses May kill fetus or cause brain damage . Giardia, Toxoplasma, Entamoeba: Review from Unit 1
6.
7.
8.
9.
Cryptosporidiosis a. Cryptosporidium parvum b. Obligate intracellular protist sporozoan, with life cycle kind of like T. gondii, but can use many species as definitive hosts c. Diseases i. Enteritis explosive diarrhea, malabsorption for weeks ii. Immunocompromised common problem in AIDS patients and may last for life
10. Worms a. Whipworm nematode i. Trichuris trichiura a. Small: ~1-3 inches b. Can live years in host dog or human ii. Disease a. Enteritis chronic diarrhea b. Small hemorrhages may occur where worms attach. 1. Secondary infections of bacteria 2. Anemia if worm load high b. Review from Unit I i. Hookworm ii. Ascariasis iii. Pinworm iv. Tapeworm E. HEPATITIS 1. Overview a. Viruses Viruses that cause hepatitis are unrelated, evolutionarily. They all just happen to live in the liver. There is no cure, little treatment (interferons for some). b. Alcohol and drugs Exacerbate hepatitis because they kill liver cells. Liver detoxifies both, and so they accumulate in liver cells, stressing them. Fortunately, liver is capable of regeneration c. Symptoms i. Inflammation abdominal pain, jaundice, fatigue, weight loss, diarrhea, dark urine ii. Hepatocellular Carcinoma (HCC) May develop in some people, probably due to constant damage and regeneration in liver more and more mutations in liver cells cancer. d. Chronic vs Acute Chronic may be lifetime. Some viruses are only acutesudden onset, last a few months at most. Hepatitis A Virus (HAV) a. Transmission: fecal-oral Not sex! Often associated with unwashe produce b. Disease i. Asymptomatic Many people ii. Acute hepatitis Some people c. Vaccine available Hepatitis B Virus (HBV) a. Transmission i. Sex, blood, MTCT same as HIV notice map b. Half-life, ID50 much longer and lower than HIV c. Disease i. Hepatitis chronic, often lifelong ii. HCC may develop
2.
3.
d. e. 4.
iii. HIV co-infections common b/c of same Tx. Co-infections are synergistically worse than each alone Virulence factor: HBsAg Hepatitis B soluble antigen: virus sheds bits of receptor, presumably to sop up antibody Vaccine Now given at birth
Hepatitis C Virus (HCV) similar to HBV but less severe. RNA virus, less stable. a. Transmission: Sex, blood, MTCT b. Chronic hepatitis, HCC Both can occur, but less likely than with HBV c. HIV co-infection Same as HBV: both become worse d. Vaccine There isnt one. Hepatitis D Virus (HDV) a. HBV relative: Satellite virus b. Smallest viral genome. Has lost its ability to replicate on its own. Requires HBV in the same cell and steals HBVs proteins. Works because both are transmitted by same means, so often ferried together. Exacerbates HBV infection. Most common for IDU.
5.
III. Genitourinary Infections Unit 6. Major Infections Bonanza Accompanies Ch. 23 A. URINARY TRACT ANATOMY 1. 2. 3. 4. Kidneys (neph-) Filter blood to remove toxins, urea Ureters connect kidneys to bladder Bladder stores urine Urethra tube through which urine exits body
B. URINARY INFECTIONS 1. Healthy urine is sterile few things can live in high [urea]; bacteria need urease a. Gram stain urine common way to confirm UTI b. WBC in urine indicate possible inflammation Bacterial infections viral infections not common, although possible cause of chronic cystitis a. Usually GI bacteria, esp. E. coli due to rectal proximity b. Females: lifetime risk simple anatomy c. Males: mainly infants, elderly Treatment Abx based on culture Urinary catheters major source of infections Types a. Urethritis inflammation of the urethra b. Cystitis inflammation of the bladder c. Nephritis inflammation of the kidney (secondary to UTI or systemic infection) d. Prostatitis inflammation of the prostate Virulence factors a. P pili to adhere to epithelia b. Urease to degrade urea
2.
3. 4. 5.
6.
C. REPRODUCTIVE ANATOMY 1. Female a. b. c. d. e. Male a. b. c. d.
Ovaries make eggs Fallopian tubes eggs travel to uterus Uterus where embryo/fetus matures Cervix muscular ring capping vagina; normally closed or nearly so Vagina birth canal Testes where sperm mature Epididymis where sperm are stored Vas deferens path sperm travel to exit Urethra exit from body; shared with urine unlike in females, so more regularly disinfected
2.
D. STIs OVERVIEW 1. Women more severely affected: why?Urethra shares urine in males, so inflammation will cause pain in urination. Women less likely to know they are infected and go untreated longer. Men more likely to transmit: why? It is easier for the insertive partner to transmit to the receptive partner than vice versa. Prenatal screening for STIs Required by most states. a. Neonatal health Neonates can be infected during birth b. Surveillance Can be extrapolated to determine prevalence in general population. c. Diseases screened Usually chlamydia, gonorrhea. Sometimes HIV. d. III. Urogenital Infections Common effects a. Genital ulcers open sores on genitals: painful, increased HIV/HBV/HCV transmission b. Sexually transmitted urethritis Mostly men c. Epididymitis very painful, fever d. Cervicitis creates discharge changes e. Vaginitis usually due to normal flora, not sexually transmitted (but sometimes sexually related) f. Pelvic inflammatory disease (PID) Abdominal pain or no symptoms at all: inflammation of uterus, fallopian tubes, ovaries. Can cause sterility, miscarriages, ectopic pregnancies. Risk rises with # partners. g. Lymphadenitis swelling of inguinal nodes common symptom Prevention a. Relative risks of sexual behaviors: abstinence outercourse female oral male oral vaginal anal b. Barrier contraceptives i. Condoms male or female ii. Proper use 85%-95% more effective than nothing at preventing STD transmission iii. Chemical contraceptives eg pill, spermicides = ineffective at preventing STD transmission c. Early detection / partner notification important public health measures d. Role of sexual health clinics i. III. Urogenital Infections D. STIs Overview
2. 3.
4.
5.
6.
Mastitis inflammation of mammary glands a. Not an STI, but reproductive! Mainly occurs in first 3 months of lactation, when ducts developing b. Disease painful, red swelling on breast, fever, malaise c. Prevention keep ducts drained of milk d. Treatment of reproductive infections e. Bacterial Abx f. Viral only treatment is for HSVno cures.
E. REPRODUCTIVE INFECTIONS Syphilis declining a. Treponema pallidum fastidious bacterium b. Transmission: Sexual, MTCT c. Syphilis 1: Chancres genital sores 2: systemic, fever, malaise, lymphadenitis, rash may be anywhere, especially feet soles Latency possibly decades 3: Organ failure nervous system or CV system, lesions on skin (gummas Fetus can cause spontaneous abortion or cause congenital syphilis Gonorrhea a. Neisseria gonorrhoeae (gonococcus) The second special coccus b. Transmission: sexual, MTCT c. Pathogenesis lives in lymphoid tissue under mucosal lining, has complement evasion VFs, survives phagocytosis d. Gonorrhea (clap) Genital creamy white discharge Oral/Anal redness, pain, pus PID common cause Neonatal blindness Chlamydia a. C. trachomatis intracellular in epithelia; C. pneumoniae relative b. Transmission: sexual, MTCT c. Diseases Genital: cloudy discharge Oral / anal: sores PID: most common cause Trachoma (Neonates) inflammation of eyelid scarring and blindness in neonates. a. Incidence: top STD in U.S. 4. Herpes simplex 1,2 (HSV1,HSV2) a. Tissue tropism HSV1 oral HSV2 genital. Skin = lytic tissue, Trigem/sacral nerves = latent. b. Latency/reactivation stress/IC related c. Primary vs Recurrent primary last longer, more severe (may be fever, pain); recurrent may have no symptoms other than minor sores d. Special cases i. Neonates may be fatal, especially if 1 infection at birth ii. Health Workers ob/gyn, dentists may get sores on hands 3. 2. 1.
Human papillomavius (HPV) a. Strains 200+! b. Transmission: contact c. Diseases i. Warts benign tumors: growths, not sores Genital cauliflower appearance Elsewhere all warts, anywhere i. Cervical cancer only a few strains cause thisfour cause 2/3 of all cancers ii. Others? Oropharyngeal; some evidence of link to prostate cancer b. Pathogenesis have genes that make proteins that cause cell to divide. Why? It does not have a gene for DNAdependent DNA polymerase. It must use the host cells replication enzyme, but the cell will only produce that enzyme when dividing. c. Screening: Pap smear Very effective; reduces cervical cancer rates 90+% where used. Cervical cancer may develop years after sex with transmitting partner has ceased, so exams are regular. e. Treatment cryotherapy f. Vaccine Gardisil or Cervarix i. What it is subunit vaccine against the four strains that most often cause cancer, so it is not a guarantee! ii. Controversy some people upset about vaccinating pre-teen girls against an STD. But the vaccine is most effective in these years. iii. Boys? Men are transmitters, and possibly affected by cancers toostudies in progress on whether they should get vax too 6. 7. Trichomonas: Review from unit 1 Candidiasis: Review from unit 1 a. Not generally an STI imbalance in hormones that increases alkalinity of vagina, or Abx b. Fungal commensal Bacterial vaginosis (BV) a. Commensals as opportunists When vaginal fluid becomes too acidic b. Symptoms irritation, pain, strong odor, discharge not a good indicator c. Causes unknown, possibly many i. Multiple sex partners? ii. Douching? iii. Other?
5.
8.
IV. CNS Infections Unit 6. Major Infections Bonanza Accompanies Ch. 24 A. CNS ANATOMY 1. Brain and spinal cord a. Meninges: 3 layers dura, pia, arachnoid. Line entire CNS (brain and spinal cord) b. Cerebrospinal fluid (CSF) made in the ventricles of the brain, drains unidirectionally down spinal cord and empties into blood c. Blood-brain barrier not a physical structure: refers to fact that endothelia in brain are less permeable. Cranial nerves nerves connected directly to brain (not to spinal cord then brain), which ennervate the head, including major sensory organs like eyes-mouth-nose-ears.
2.
3.
Spinal nerves peripheral (not CNS), two per vertebra. Connect spine and thus brain to rest of body. Can be organized into dermatomes, as each innervates a specific patch of skin, muscle and underlying organs
B. CNS INFECTION OVERVIEW 1. Routes to brain for pathogens a. Via cranial nerves: teeth, middle ear, sinus b. Via blood (possibly in monocyte) across BBB c. Via breaks in skull Edema consequences edema (fluid in tissues) a risk of inflammation (extravasation, vasodilation) a. Vasogenic edema from endothelial cell junctions breaking; protein/fluid in brain b. Cytotoxic edema from WBCs extravasating into brain Common symptoms a. Meningitis inflammation of the meninges: headache, stiff neck, usually high fever, mental dysfunction. Stiff neck can be detected in kids via test at right. b. Encephalitis no meningitis symptoms, but have other signs of infection: seizures, paralysis, mental dysfunction c. Peripheral nerve effects weakness, paralysis of part or all of body Diagnosis Spinal tap smear or culture for pathogens or WBCs Treatment a. Bacterial Abx b. Fungal or protozoan drugs c. Viral usually supportive d. The pathogens POV Brain is a dead endb/c of location and BBB, no way to transmit. Not a goal. Always secondary to infection elsewhere in the body (usually pharynx or systemic), or entirely accidental (eg brain-eating ameba). Peripheral nerves might be favorable places to hang out, though, because they reach epithelia (herpes viruses)
2.
3.
4. 5.
C. MENINGITIS 1. Acute meningitis a. Dangers fast progression to brain damage, hearing loss, death b. Bacterial vs viral worst are bacterial c. Viral causes usually self-resolving and without lasting effects, but sometimes cause long-term effects as above i. Enteroviruses, e.g. coxsackie ii. Mumps, Measles iii. Others Significant causes a. Pneumococcus and Hib i. Streptococcus pneumoniae and Haemophilus influenzae b Bacteria that often cause ear infections, pneumonia ii. RTIs reach meninges via sinuses, where they erode bone iii. Pediatric used to be relatively common among children <5 iv. Vaccines now standard, decreased cases by 90%
2.
b.
Meningococcus i. Neisseria meningititis the meningococcus. Very acute. Intracellular. ii. Transmission: Droplet iii. Systemic High doses of capsule-competent strains may damage endothelia, travel in blood throughout body. Causes sepsis in blood (even if dead, b/c of LPS). Purple rash, non-blanching, 50% mortality within hours. May or may not accompany meningitis. iv. Dorms highest incidence in dorms/barracks v. Vaccine required for most colleges, now standard childhood vaccine Acanthamoeba and Naegleria spp.: Review Unit 1
c. 3.
Chronic meningitis lasts weeks a. Immunocompromised b. Common causes i. Toxoplasma gondii (unit 1) ii. TB (prior slides) iii. Fungi: Histoplasma, Coccidioides, Cryptococcus (unit 1, prior slides) iv. Trypanosoma brucei (unit 1) v. Others
D. ENCEPHALITIS AGENTS 1. 2. Many meningitis agents also cause this Viral encephalitis by Arboviruses, e.g. West Nile Virus, St. Louis encephalitis arbovirus = insect-borne a. Transmission: mosquito b. Only 1% symptomatic c. Other hosts: horses, birds Rabies virus a. Transmission: vector b. Hosts all mammals. Primary urban agents of human transmission = dogs. Primary sylvatic agents of human transmission shown in map, plus bats c. Pathogenesis initially infects lungs, then migrates to peripheral and then central nervous systems, as well as organs throughout the body. Replicates in salivary glands, making swallowing painful d. Symptoms high fever, acute encephalitis. Hosts may avoid eating or drinking due to pain, and inability to swallow saliva creates foaming at mouth. But aggression is just animal response to fear plus CNS disruption. e. Mortality 100% without treatment. Vaccination after exposure can block dissemination out of lungs; only virus for which vaccine is a treatment.
3.
E. Other CNS Infections 1. Tetanus a. Clostridium tetani endospore-forming obligate anaerobe. Reservoir: soil, animal GI (commensal) b. Transmission: parenteral c. Pathogenesis germinates in deep tissue (having been introduced by nail or knife) and produces tetanus exotoxin, which allosterically binds acetylcholine receptors (where neuron meets muscle cell) and activates them d. Symptoms starts with lockjaw (TMJ paralysis), progressive rigid paralysis elsewhere until diaphragm stops working death e. Vaccine: Td, DTaP, Tdap often given with diphtheria/pertussis, needs booster every 10 years f. IV. CNS Infections E. Other CNS Infections
2.
Botulism a. Clostridium botulinum also anaerobic endospore former from soil b. Transmission: food especially canned foods, especially home-canned, or unpasteurized honey (both have high osmotic pressure that prevents other bacteria but endospores survive) or dry processed foods (think Ramen soups) c. Pathogenesis germinates in GI; botulinum exotoxin absorbed into blood and allosterically binds acetylcholine receptors to keep them in permanently inactive state d. Symptoms gastroenteritis, then flaccid paralysis, diaphragm paralysis then death e. SIDS link infants most susceptible, and some SIDS cases may actually be due to undiagnosed botulism Poliomyelitis a. Polio virus an enterovirus b. Transmission: fecal-oral c. Pathogenesis may cross gut to reach blood, spreads to peripheral and then central nervous system. Degrades motor neurons of the spine, which do not regenerate d. Symptoms i. Asymptomatic many people ii. Minor or nonparalytic most people have fever and possible meningitis iii. Paralytic 2% of people, increasing with age of primary infection. Asymmetric paralysis (usually just one limb). e. Vaccines oral or injectable, standard childhood immunizations. There have been cases in US in recent years among Amish (who are unvaccinated) Creutzfeld-Jakob Disease (CJD) a. Prion infectious agent is just a protein that causes certain neural proteins to misfold b. Transmission: food (carnivory) of cattle or sheep fed cattle/sheep brains (or ingestion of human brains) c. Pathogenesis misfolded proteins clump up in neurons until neurons clogged and die d. Symptoms progressive psychiatric and cerebellar problems, demention, death e. Blood banks UK question screens for this
3.
4.
V. Blood Infections Unit 6. Major Infections Bonanza Accompanies Ch. 25 A. CV ANATOMY 1. Circulatory structure systemic = deliver oxygen and nutrients to body cells; pulmonary = pick up oxygen and drop off CO2 a. Arteries carry blood away from heart b. Capillaries where gas/nutrient exchange occurs c. Veins carry blood toward heart Heart double pump a. Cardiac muscle b. Chambers two ventricles, two atria c. Valves at AV and ventricle-artery junctures. Prevent blood backflow. Compromise decreased cardiac efficiency so heart must work harder. Access to organs all cells in the body can be accessed via blood
2.
3.
B. Blood Inf.: OVERVIEW 1. Access to blood Pathogen POV: nice, b/c you can get around the body, but problematic b/c lots of immune cells a. Vector eg bites b. Wounds including iatrogenic wounds, bleeding gums (teeth-brushing) c. Organs across GI, genitourinary tract, respiratory tract Types of infections a. Bacteremia/septicemia/sepsis, viremia, fungemia & parasitemia Ways of describing pathogens in the bloodstream b. Infectious endocarditis infections of the heart muscle or heart valves c. Thrombophlebitis, endoarteritis infections of veins or arteries (endothelial tissue) Venous catheters, IV lines major risk of nosocomial infections i. Typically Staphylococcus aureus or epidermidis (why?) common on skin, can come from patient or nurse ii. Pseudomonas aureginosa common with IV-associated infection (not venous catheters), comes from stool (usually patient) Relationship to shock a. Septic shock Bacteria in the bloodstream, if enough of them. Usually gram negative b. Toxic shock superantigen in bloodstream (with or without bacteria) The superantigen is a toxin that activates any T cell (binds TCR) i. Staphylococcus aureus and Streptococcus pyogenes Produce the toxins that could elicit shock ii. Tampons sometimes implicated, if left in too long (often days)
2.
3.
4.
C. INFECTIOUS ENDOCARDITIS 1. Pathogenesis a. Infection bacteria or virus in the blood infects interior heart muscle, causing damage and resulting clot b. Adherence bacteria stick to the clot, may increase it c. Emboli clot breaks off, flows to smaller blood vessels and blocks blood flow petechial hemorrhages, stroke, coronary embolism d. Immune complexes Abs bind the emboli and recruit complement, increasing cell damage Common causes a. Oral Streptococci enter via bleeding gums b. Skin or fecal bacteria enter via wounds
2.
D. BACTEREMIA 1. 2. Same as endocarditis bugs and Group B Strep (GBS) Beta hemolytic streptococcus a. S. agalactiae normal vaginal flora, but not present in all women. Testing in last ~3 weeks before giving birth. b. Diseases 1. Puerperal fever sepsis in mother, post-birth. Major cause of death due to childbirth if no access to clean water, Abx 2. Neonatal bacteremia, meningitis, pneumonia Depending on where infant infected a. Incidence: common cause of neonatal death in U.S.
E. BLOOD INFECTIONS 1. Epstein Barr Virus (EBV; herpes 4) a. Tissue tropism lytic in pharyngeal epithelia; latent in B cells b. Transmission: droplet Hard to get: requires high ID50 c. Pathogenesis Kills pharyngeal cells, causing inflammation. Causes some B cells to divide, encouraging viral replication. Makes B cells look like monocytes (atypical lymphocytes) d. Symptoms i. Asymptomatic many people have few to no symptoms ii. Infectious mononucleosis Fever, malaise, pharyngitis, lymphadenitis, enlarged spleen. Mainly in adolescent primary infections, probably because they have a very fierce T cell response. iii. Burkitts Lymphoma (Malarial regions) rare B cell cancer of unknown etiology, related to latency in B cells. Only occurs where malaria also occurs. iv. Nasopharyngeal Cancer (China) Common cancer in China of unknown etiology but linked to infection. v. Other lymphomas In IC individuals Cytomegalovirus (CMV; herpes 5) a. Tissue tropism latent in leukocytes/bone marrow (problematic for transplants/transfusions) b. Transmission: droplet + sex? c. Symptoms i. Asymptomatic most healthy people have no symptoms or just feel tired; most infected at some point in life ii. Fetuses if mothers primary infection is in pregnancy, fetus may be born jaundiced (jaundice common in newborns for other reasons too!). Hearing loss and learning disabilities may develop later. iii. Immunocompromised pneumonia if respiratory, flu-like symptoms and pneumonia if via transfusion/transplant Lyme Disease a. Borellia borgdorferi fastidious spiral bacterium with reservoir in mice, problem especially in E. US b. Transmission: deer tick tiny tiny! c. Pathogenesis difficult to study! Hypothesis: unusual cell wall LPS triggers confused chronic immune reaction wherever pathogen is (first skin, later joints/brain) d. Symptoms 1. Rash sometimes bullseye shape with fever, pain for months. Lack of neutrophil response, chronic inflammation. 2. Arthritis later inflammation to joints, very painful Chagas Disease a. Trypanosoma cruzi protozoan flagellate b. Transmission: vector, vertical kissing bug, so called because it is attracted to CO2 exhaled while victim sleeps. Bites near mouth, but actual transmission is from its poop, which may enter through eye or wound. Lives in thatched roofs. c. Pathogenesis May stay at bite site inflammation. If disseminates, forms a pseudocyst inside cardiac or autonomic (involuntary) nervous system cells d. Symptoms Acute: flu-like symptoms. If poop was in eye, get droopy eye for a few weeks, like this kid. Some develop chronic infection and may immediately or years later suffer organ failure, especially of heart or GI, due to pseudocysts e. Distribution: Latin America, US issue with immigrants, blood banks
2.
3.
4.
5.
Brucellosis a. Brucella spp. bacteria b. Transmission: food esp. unpasteurized milk a. goats/sheep, swine, cattle spreads in herd animals by inducing abortion; inhalation/ingestion of decaying fetus/placenta. c. Symptoms a. Flu-like Initial symptoms. May develop into chronic nocturnal fever. b. Abortion causes spontaneous abortion in humans too. Bioterror has been explored as possible bioterror agent Tularemia (Rabbit fever) a. Francisella tularensis fastidious bacterium b. Transmission: multiple Usually wound infected while butchering small mammals, e.g. rabbits, squirrels, for meat. Improbable but ID50 is low! c. Symptoms Ulcerated wound, granulomas in skin, buboes. If disseminated, high fever, organ failure, high mortality. d. Bioterror can also be inhaled, so proposed bioterror agent (but so tough to grow this is really unlikely)
a. 6.
7.
Plague Black plague named for buboes a. Yersinia pestis gram negative bacteria b. Transmission: vector flea bite c. Pathogenesis lives in macrophages, spreads to lymph nodes and rapidly multiply. Massive immune recruitment there, and dying bacteria release LPS into lymph, then blood septic/toxic shock. d. Bubonic plague buboes are purple, swollen lymph nodes. High fever, death in days. Rickettsial infections a. Rickettsia overview i. Obligate intracellular bacteria Very small and simple, kind of like viruses, and also intracellular. ii. Transmission: arthropods All are transmitted by insect/arachnid bites b. Rocky Mountain Spotted Fever i. R. rickettsia ii. Pathogenesis infects and kills endothelial cells, causing blood vessel collapse iii. Symptoms Rash due to blood leaking into tissues, possible clot development and subsequent embolism formation. Organ failure due to blood loss in organ possible. iv. Dog ticks, others Big! Visible! c. Typhus flu-like symptoms, rash (same rash as RMSF), very high fever, high mortality if untreated i. Epidemic Typhus a. R. prowazeckii b. Transmission: vector transmission by lice ii. Endemic Typhus (murine typhus) a. R. typhi b. Transmission: vector transmitted by rat flea Arboviruses insect-borne viruses a. Transmission: Aedes mosquitoes striped mosquito invasive to Americas b. Dengue fever virus i. Diseases a. Dengue Fever Quebrante huesos, breakbone fever. Terrible muscle and joint pain, high fever b. Dengue hemorrhagic fever may develop, depending on strains. Hemorrhage internal and external.
8.
9.
ii. iii. c.
Distribution tropics (can only be spread by Aedes aegypti) U.S. Emergence? Mosquito recently seen in SW US
d.
Yellow fever virus i. Diseases similar to dengue fever but pain is less and liver problems more. Jaundice, swollen abdomen. Hemorrhagic fever may develop. ii. Distribution Equatorial Africa and Latin America iii. Vaccine most effective vaccine ever developed. You get a yellow card (photo) to prove you have it. Others, eg West Nile Borne by other species of Aedes mosquito genus, found farther north, including here. Serious human infections rare.
10. Ebola and Marburg viruses a. Transmission: blood reservoir unknown; bats suspected. Possibly begins with bat bite and spreads to victims caretakers. b. Pathogenesis break down cell:cell boundaries between epi/endothelial cells. c. Symptoms fever, severe hemorrhaging, inside and out. d. Outbreaks Small, every few years in Central/East Africa. Only large outbreaks (numbering in hundreds) associated with iatrogenic transmission: non-sterile practices in hospital care (e.g. no gloves/masks, non-sterile needles). 11. Lymphatic filiariasis sometimes called elephantiasis a. Wuchereria bancrofti, Brugia malayi roundworms b. Transmission: mosquito c. Pathogenesis Baby worms in blood; adult worms live in lymph vessels. Have bacteria inside them that, when released on worm death, cause inflammation, scarring. d. Symptoms Early: parasitemia (baby worms in blood), fever, fatigue. People born in endemic areas may not have symptoms. Later, if untreated: painfully swollen limbs/scrotum from repeated scarring. e. Distribution tropics 12. Malaria: Review Unit 1 13. HIV: Review Unit 5 VI. EYE INFECTIONS Unit 6. Major Infections Bonanza Accompanies Ch. 26 A. EYE ANATOMY 1. 2. 3. 4. Cornea covering over pupil, lens Conjunctiva lines eye and eyelid, makes tears Sclera hard eye casing Optic nerve direct to brain
B. EYE INFECTIONS 1. 2. Pathogen access usually skin (touch) or URTIs Conjunctivitis, keratitis conjunctiva, cornea a. Many bacteria, esp. Pseudomonas; rare viruses b. Amoebas: review Unit 1 c. Neonates, esp. N. gonorrheae
d. 3.
Connection to contacts improper cleaning, leaving in too long
Trachoma a. Chlamydia trachomatis The STD b. Transmission: vertical/contact often during birth, can also be from eye discharge to anothers eyes via hands/cloth c. Pathogenesis scar tissue from infection covers eye d. Prevention: antibiotics in newborns eyes e. Prevention: SAFE surgery antibiotics face washing environmental improvements. Important in very poor communities without clean water or latrines Sty: Staphylococcus aureus usually. A boil in an eyelash follicle. Loaisis a. Loa loa worm b. Transmission: deer fly vector Central Africa forests (solid below) c. Disease parasitemia while it migrates to eye; then vision loss due to inflammation/scarring Onchocerciasis (River blindness) a. Onchocerca volvulus Another worm, related to loa loa, also African (hatched region on prev. slide) b. Transmission: black fly vector breeds in fast-moving water (hence River blindness). Thus, bigger problem in some ways than loa loa b/c of where people live c. Disease similar to loaiasis. Results in blindness. d. Impact Major problem; once common for young girl to be assigned to lead grandfather around by a stick, hence this statue at WHO HQ e. WHO efforts massive control program over past 40 years: drugs, education and vector elimination great success
4. 5.
6.
VII. Skin Infections Unit 6. Major Infections Bonanza Accompanies Ch. 26 A. SKIN ANATOMY 1. Skin layers a. Epidermis outermost layer, includes dead cells, waxy proteins, live cells, pigment b. Dermis connective tissue underneath, with capillaries c. Subcutaneous fat d. Fascia thin webbing connecting skin and muscle Blood vessels subQ and dermis Hair shafts follicles begin in dermis Sweat glands produce sweat, antibacterial, dermis Sebaceous glands produce oil, antibacterial, dermisassociated with follicles Pathogen entry a. Wounds mostly opportunists, fecal or Staphylococcal b. Glands/follicles w/ right virulence factors c. Blood systemic skin Lesions many designations for pock-marks a. Macules flat discoloration b. Papules raised bumps (often cell division) c. Vesicles fluid-filled, palpable d. Pustules pus-filled, palpable
2. 3. 4. 5. 6.
7.
B. SURFACE INFECTIONS 1. Folliculitis infected hair follicle and/or associated glands a. Bacterial infections bacteria get into hair follicle/gland and cause inflammation. b. Role of sebum Caused by bacteria with VFs that enable eating of sebum. Sebum production increases in adolescence. c. Boils (Skin abcess) blocked gland with lots of inflammation, pus d. Carbuncles complicated boil: larger, with fever Acne blocked sebaceous gland (small boil-like infection) a. Propionibacterium acnes most common cause. Can eat glycerol in sebum. b. Diseases i. Acne Most common skin infection, mostly teenagers. Whiteheads are caused by pus. Blackheads are the pushed up hair follicle. ii. Nosocomial opportunist Can infect IC patients in the hospital, problem on vents/central lines c. Treatment topical antibiotics best. Accutane also used for extreme cases. Reduces sebum production. However, many bad side effects, and pulled from market in 2009! d. Abx resistance rising due to topical treatments Impetigo a. Staphylococcus spp., GAS (Streptococcus pyogenes) Infected vesicle ruptures and bacteria spread around the area. Both species have VFs for breaking down connective tissue. Slimy yellow liquid (exudate) produced Erysipelas a. GAS (Streptococcus pyogenes) infection spreading beneath epidermis using collagenase and hyaluronidase. May lead to sepsis Scalded skin syndrome a. Staphylococcus aureus Infection can be anywhere in the body, including a wound or at tampon. Skin peels off, very painful, with fever! b. Pathogenesis Staph exotoxins called exfoliatins travel in the blood and will cause pulling away of epidermis wherever their concentration is high. Herpes simplex virus 1 (HSV1) already discussed Human papilloma virus (HPV) already discussed
2.
3.
4.
5.
6. 7.
C. SOFT TISSUE INFECTIONS 1. Tissue affected subQ and lower 2. Access a. Open wound (cut, scrape, other infection) b. Puncture / Surgical 3. Gangrene a. General i. What it is deep infection with an anaerobe, often Clostridium perfringens. C. perfringens has many VFs for penetrating tissue (e.g. lipase, hyaluronidase, collagenase) ii. Black color H2S, rotten egg iii. Treatment often debridement, also hyperbaric treatment b. Gas gangrene wound infection, usually puncture wound like knife or gunshot that plants endospore deep in tissue. Very foul odor.
c. d.
Dry gangrene: Ischemia or other necroses in extremities, eg with diabetes lack of oxygen causes dead tissue to pile up, anaerobes eat it Wet gangrene edematous fluid collected in tissue gets infected because fresh blood not flowing in with WBCs, Abs, etc. Bacteria grow in the stagnant blood. i. Bedsores ii. Other moist parts of body with inadequate venous flow iii. VII. Skin Infections C. Soft Tissue Infections
3.
Necrotizing fasciitis a. GAS (Streptococcus pyogenes) GAS from mouth enter a wound and can, if dose is high enough, kill fascia b. Pathogenesis multiple exotoxins and other VFs, including the ability to both make and break clots, and a superantigen that causes shock Pseudomonas aeruginosa actually infects many parts of the body as an opportunist when normal flora or barriers are compromised. Major problem in CF patients pneumonia. Also a UTI. If it gets into wounds, may cause necrosis Pyocyanin green-blue pigment made by bacterium makes easy to recognize. Smell like grape Kool-Aid Especially burns burn patients especially susceptible to skin infections generally, esp. this. 4.
b. c. 5.
Cutaneous anthrax a. Bacillus anthracis common soil bacterium b. 95% of anthrax cases respiratory infections rare and cause bioterrorism alert. Skin cases are also notifiable, though! c. Pathogenesis endospore gets into wound and causes papule, then ulcer. If does not get into bloodstream, resolves okay.
D. Fungal/Parasitic Review from Unit 1 1. Candida albicans 2. Tinea spp. 3. Leishmania
E. Systemic Infections Affecting Skin all viral 1. Measles a. Transmission: droplet highly contagious b. Symptoms cough/congestion/fever progress to spots on inside of cheek and then to full-body macular rash due to virus in lymph. Without supportive care, death rates are 10-25% among healthyhigher among IC. Small chance of encephalitis and permanent brain damage. c. Vaccine US/Europe: part of the MMR d. WHO goals Sustainable reduction in 47 countries. Strengthen local providers to create culture of routine childhood immunizations. 90% reduction in Africa from 00-08! Rubella (German measles) a. Transmission: droplet, vertical b. Symptoms mild or asymptomatic with fever, lymphadenopathy and faint macular rash c. Fetus Very high frequency of placenta crossing: congenital rubella growth defects, retardation, and/or deafness d. Vaccine The R in MMR Varicella zoster (herpes 3)
2.
3.
a. b.
Tissue Tropism lytic in epithelium; latent in spinal nerves Diseases i. Chicken pox Full body vesicular rash, itchy! Virus stays in spinal nerve for ~1/3. ii. Shingles Virus reemerges when immune system weakened (?) and causes very painful rash along dermatome associated with that spinal nerve. Adults have stronger anti-viral response. Can last months and can be fatal.
3.
Chickenpox and shingles (herpes 3) d. Treatment Herpes simplex drugs can be used e. Vaccine Routine childhood shot since 1995. Shingles vaccine is essentially chicken pox vaccine with higher dose f. Links among shingles and chicken pox and vaccine People who have never had chicken pox cannot get shingles (though they may have had mild case of chicken pox). The vaccine protects against shingles (which is why it is given despite chicken pox being fairly benign). However, the use of the vaccine in children seems to increase the incidence of shingles among adults in the same society who carry the latent virus. The thinking is that those adults were routinely exposed to infected kids shedding virus, giving their VZV-specific memory cells a tiny little taste and causing proliferation more memory cells. This kept the latent virus better in check. Today, few kids are shedding virus so the memory may decline. Smallpox (Variola) a. Transmission: droplet b. Symptoms Fever, pustular rash, 20-30% mortality c. History Routine childhood infection throughout Old World; genocidal in New World d. Eradication 1950s-70s, last case in 1977 Somalia. Vaccinations stopped in US in 1972. e. Bioterror Vials stored in Moscow and Atlanta. Fears of bioterror means US keeps vax stockpiles.
4.
S-ar putea să vă placă și
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- NCLEX Cram SheetDocument2 paginiNCLEX Cram SheetSarah Plunkett100% (1)
- Concept Map of Nursing SchoolDocument1 paginăConcept Map of Nursing SchoolSarah PlunkettÎncă nu există evaluări
- Backup NclexDocument61 paginiBackup NclexSarah PlunkettÎncă nu există evaluări
- Drugs Med-SurgTest 3Document6 paginiDrugs Med-SurgTest 3Sarah PlunkettÎncă nu există evaluări
- MedSurg Medications & TablesDocument71 paginiMedSurg Medications & TablesSarah PlunkettÎncă nu există evaluări
- Patho FinalDocument25 paginiPatho FinalSarah PlunkettÎncă nu există evaluări
- MedSurg Medication Study Guide Test 1Document12 paginiMedSurg Medication Study Guide Test 1Sarah PlunkettÎncă nu există evaluări
- Helicobacter Pylori-A: Transmission Pathogenesis Incidence Symptoms Other Diseases Vaccine? Stomach UlcersDocument4 paginiHelicobacter Pylori-A: Transmission Pathogenesis Incidence Symptoms Other Diseases Vaccine? Stomach UlcersSarah PlunkettÎncă nu există evaluări
- Soft Tissue InfectionsDocument1 paginăSoft Tissue InfectionsSarah PlunkettÎncă nu există evaluări
- Upper Respiratory Tract InfectionsDocument1 paginăUpper Respiratory Tract InfectionsSarah PlunkettÎncă nu există evaluări
- Eye InfectionsDocument1 paginăEye InfectionsSarah PlunkettÎncă nu există evaluări
- Transmission Pathogenesis Incidence Symptoms Other Diseases Vaccine? Acute MeningitisDocument4 paginiTransmission Pathogenesis Incidence Symptoms Other Diseases Vaccine? Acute MeningitisSarah PlunkettÎncă nu există evaluări
- Blood InfectionsDocument3 paginiBlood InfectionsSarah PlunkettÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Environmental and Sustainability Issues - 1Document21 paginiEnvironmental and Sustainability Issues - 121. PLT PAGALILAUAN, EDITHA MÎncă nu există evaluări
- Fill in The Table by Determining The Functions of The Following ItemsDocument6 paginiFill in The Table by Determining The Functions of The Following ItemsJessabel CandidatoÎncă nu există evaluări
- Oertel - Extracts From The Jāiminīya-Brāhma A and Upanishad-Brāhma A, Parallel To Passages of TheDocument20 paginiOertel - Extracts From The Jāiminīya-Brāhma A and Upanishad-Brāhma A, Parallel To Passages of Thespongebob2812Încă nu există evaluări
- Aipl2009 V120000001Document7 paginiAipl2009 V120000001Olof HedinÎncă nu există evaluări
- Motion of A Simple Pendulum in A FluidDocument16 paginiMotion of A Simple Pendulum in A FluidGokul JeevaÎncă nu există evaluări
- Regulatory Framework For Water Dams in QuebecDocument2 paginiRegulatory Framework For Water Dams in QuebecRaveeÎncă nu există evaluări
- The Practice of Veterinary Anesthesia - Small Animals, Birds, Fish, and ReptilesDocument382 paginiThe Practice of Veterinary Anesthesia - Small Animals, Birds, Fish, and ReptilesMárcio MoreiraÎncă nu există evaluări
- Pastor O. I. Kirk, SR D.D LIFE Celebration BookDocument63 paginiPastor O. I. Kirk, SR D.D LIFE Celebration Booklindakirk1100% (1)
- Steam Purity Considerations For New TurbinesDocument46 paginiSteam Purity Considerations For New Turbinesomertrik100% (1)
- Department of Mechanical EnginneringDocument11 paginiDepartment of Mechanical EnginneringViraj SukaleÎncă nu există evaluări
- Jerms B 2109 - 0BDocument10 paginiJerms B 2109 - 0BNothing is ImpossibleÎncă nu există evaluări
- Fast Track Pro Drivers Read MeDocument3 paginiFast Track Pro Drivers Read MeMatt JerniganÎncă nu există evaluări
- CA InsideDocument1 paginăCA InsideariasnomercyÎncă nu există evaluări
- Big Fat Lies - How The Diet Industry Is Making You Sick, Fat & PoorDocument212 paginiBig Fat Lies - How The Diet Industry Is Making You Sick, Fat & PoorangelobuffaloÎncă nu există evaluări
- Biology Unit 4Document44 paginiBiology Unit 4Mohammad KhanÎncă nu există evaluări
- Q3 Module 15Document33 paginiQ3 Module 15jovielyn kathley manaloÎncă nu există evaluări
- Science BiologyDocument76 paginiScience BiologynaninanyeshÎncă nu există evaluări
- Materi B.inggris SMP Kelas 9 Kurikulum 2013Document21 paginiMateri B.inggris SMP Kelas 9 Kurikulum 2013Siti DianurÎncă nu există evaluări
- CSA Pre-Test QuestionnaireDocument16 paginiCSA Pre-Test Questionnairedaniella balaquitÎncă nu există evaluări
- Earthing ResistanceDocument4 paginiEarthing ResistanceNeeraj Purohit100% (1)
- MIKE21BW Step by Step GuideDocument124 paginiMIKE21BW Step by Step Guideflpbravo100% (2)
- Mensuration Practice SheetDocument1 paginăMensuration Practice SheetSonia SabuÎncă nu există evaluări
- Modeling Plastics in ANSYS (Compatibility Mode) PDFDocument14 paginiModeling Plastics in ANSYS (Compatibility Mode) PDFashutosh.srvÎncă nu există evaluări
- Detailed Lesson Plan in Science IiiDocument3 paginiDetailed Lesson Plan in Science Iiicharito riveraÎncă nu există evaluări
- HPLC Columns by SciencixDocument49 paginiHPLC Columns by SciencixBrett HarrisÎncă nu există evaluări
- UntitledDocument300 paginiUntitledUnbox itÎncă nu există evaluări
- Relatório Final Do Período Experimental - Paulo Manuel Correia Da SilvaDocument56 paginiRelatório Final Do Período Experimental - Paulo Manuel Correia Da SilvaMagda RuanoÎncă nu există evaluări
- Course Specification Course Title: Basic Architectural DraftingDocument1 paginăCourse Specification Course Title: Basic Architectural DraftingDinah Fe Tabaranza-OlitanÎncă nu există evaluări
- Pre-Test First QTR 2022-2023Document3 paginiPre-Test First QTR 2022-2023anna marie mangulabnanÎncă nu există evaluări
- DRS Rev.0 GTP-TR1!01!002 Condensate RecyclingDocument4 paginiDRS Rev.0 GTP-TR1!01!002 Condensate RecyclingBalasubramanianÎncă nu există evaluări