Documente Academic
Documente Profesional
Documente Cultură
Acute Myocardial Infarction: Recognition and Assessment
Încărcat de
HasnainKhimjiDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Acute Myocardial Infarction: Recognition and Assessment
Încărcat de
HasnainKhimjiDrepturi de autor:
Formate disponibile
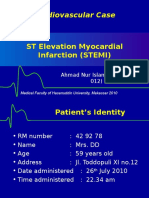
Acute MI 2009-10
ACUTE MYOCARDIAL INFARCTION
RECOGNITION AND ASSESSMENT
Symptoms and signs Severe, persistent chest pain Dyspnoea Fear Pallor Sweating Anxiety Peripheral vasoconstriction Shock Investigations ECG (see below) Markers of myocardial injury if patient located in emergency portal of entry (A&E/ECC/HAC/CCU), use myoglobin and/or troponin T, depending on location see Triage of patients with chest pain guideline if patient located in other wards, use serial daily plasma creatine kinase (CK) and aspartate transaminase (AST) after coronary occlusion, CK rises to peak at 24 hr (6-12 hr if thrombolytic therapy given) and AST at 48 hr Plasma cholesterol (within 12 hr of onset of symptoms; otherwise leave for at least six weeks) Venous blood glucose and HbA1c If using unfractionated heparin and reteplase as thrombolytic therapy, FBC, INR, APTT see Heparin-induced thrombocytopenia guideline
IMMEDIATE TREATMENT
Aspirin 300 mg (chew, macerate and swallow) Diamorphine 1 mg/min IV until pain relieved, up to maximum 10 mg (5 mg in elderly or frail patients) Metoclopramide 10 mg IV over 1-2 min (4 mg in young adults 15-19 yr <60 kg) with 8 hrs before repeating O2 high flow see Oxygen therapy in acutely hypoxaemic medical patients guideline Atenolol 5 mg IV (over 5 min) or 50 mg orally daily, unless contraindicated see BNF section 2.4 Start atorvastatin 80 mg for all acute coronary syndromes, unless eGFR abnormal if eGFR 30-60, substitute atorvastatin 40 mg if eGFR <30 (i.e. CKD 4/5) take specialist advice before commencing statins Admit all patients with acute myocardial infarction (MI), or unstable angina with acute ST depression and/or raised troponin T (>0.05 ng/mL) to Ward 76/77 under the care of duty consultant cardiologist via Heart Assessment Centre (HAC) If ECG shows ST elevation MI (STEMI), follow MANAGEMENT OF STEMI If patient has a Non-ST Elevation MI (NSTEMI), follow MANAGEMENT OF NSTEMI
MANAGEMENT OF STEMI
If pre-hospital thrombolysis has been given, follow further management in this guideline admit to coronary care unit/ward 76 Look out for patients who may have been randomized by ambulance service into a study of primary angioplasty versus thrombolysis
Acute MI 2009-10
If thrombolysis not already given, consider for primary angioplasty Contact cardiology SpR on call (07936 182946) immediately if decision is NOT for primary angioplasty, give thrombolytic therapy if not contraindicated follow Thrombolytic therapy (STEMI)
Thrombolytic therapy (STEMI) Start treatment as soon as diagnosis of STEMI made and contraindications excluded. National Service Framework states that interval between patients arrival and commencement of thrombolytic therapy (`door-to-needle time') should be <20 min. Time delay means muscle lost Indications Presentation within 12 hr of onset of symptoms Typical cardiac chest pain persisting for >30 min >1 mm ST segment elevation in two or more precordial leads or two or more bipolar leads OR >1 mm ST segment depression in leads V1-V3 (suggesting acute posterior infarction) OR LBBB with any of the following in leads V1-V3: >1 mm ST segment depression >1 mm ST segment elevation where QRS complex positive >5 mm ST segment elevation where QRS complex negative Contraindications Absolute: active bleeding Relative: major trauma/major surgery within previous four weeks stroke/TIA within previous three months confirmed subarachnoid haemorrhage at any time traumatic cardiac massage or intracardiac injection known bleeding disorder active dyspepsia or history of GI haemorrhage sustained systolic BP >180 mmHg proliferative retinopathy recent head injury pericarditis INR >2.0 Cardiogenic shock and ventricular arrhythmias are not contraindications. There is no upper age limit for this treatment although there is little supportive evidence for its use in patients aged >75 yr Choice of agent Standard agent is r-PA (reteplase), which is delivered as both a pre-hospital agent and within hospital administer by giving unfractionated heparin 5000 units by IV bolus, followed by r-PA (reteplase) 10 units by slow IV injection over 1-2 min, repeated after 30 min, then give unfractionated heparin 1000 units/hr via infusion pump for 48 hr, adjusting dose to maintain APTT ratio twice normal In the elderly (>75 yr) not already given pre-hospital dose of r-PA, give streptokinase 1.5 million units in 100 mL of sodium chloride 0.9% by IV infusion over 1 hr Streptokinase can be re-administered within three days of first administration but, after five days, the likely presence of streptokinase antibodies precludes its further use for at least 12 months
Acute MI 2009-10
If thrombolysis contraindicated or unsuccessful, refer to cardiology team on call (07936 182946) for consideration of primary/rescue angioplasty Referral for urgent coronary angiography Refer to cardiology team if patient has a STEMI and: thrombolytic therapy contraindicated thrombolytic therapy fails to settle pain and/or ST segment changes patient has recurrent malignant ventricular arrhythmias Complications Hypotension if occurs de novo, review for cardiogenic shock, mitral regurgitation or tamponade. If streptokinase being administered, stop IV infusion and recommence at a slower rate after BP has recovered Bradycardia usually responds to atropine 300 microgram IV Ventricular tachycardia or idioventricular rhythm usually self-limiting and requires no therapy. If sustained see Cardiac arrhythmias guideline Avoid arterial puncture, central venous cannulation and IM injections in patients undergoing thrombolytic therapy, unless essential to patient care
MANAGEMENT OF NSTEMI
Treatment of choice for NSTEMI is in-patient cardiac catheterization with early revascularization, either by percutaneous intervention (PCI) or CABG. Refer to on-call cardiology SpR (07936 182946) Weigh patient and initiate dalteparin by SC injection (see Table 1 for dosage). Continue until 24 hr after pain relieved Give clopidogrel loading dose 300 mg (600 mg in those who are unstable and likely to require catheter lab management within 24 hr) orally If patient requires continued dalteparin, check platelet count twice weekly from day 5 (day 2 if dalteparin, any other low-molecular-weight heparin, or unfractionated heparin given within last three months) see Heparin-induced thrombocytopenia guideline
Table 1: Calculation of dalteparin SC dosage ALWAYS weigh patient do NOT guess body weight or rely on patients own estimate Body weight Dose SC dalteparin 4043 kg 5,000 units 12 hrly 4448 kg 5,500 units 12 hrly 4952 kg 6,000 units 12 hrly 5356 kg 6,500 units 12 hrly 5760 kg 7,000 units 12 hrly 6164 kg 7,500 units 12 hrly 6568 kg 8,000 units 12 hrly 6972 kg 8,500 units 12 hrly 7377 kg 9,000 units 12 hrly 7881 kg 9,500 units 12 hrly >82 kg 10,000 units 12 hrly If treatment continued for >8 days whilst awaiting angiography/revascularization, reduce dose as follows: women <80 kg and men <70 kg 5,000 units 12 hrly women >80 kg and men >70 kg 7,500 units 12 hrly
Acute MI 2009-10
NON-DIABETIC PATIENTS WITH BLOOD GLUCOSE >11 mmol/L AND ALL PATIENTS WITH DIABETES MELLITUS
Check plasma potassium, but do not await result Give simultaneous IV infusions of glucose 5% and Actrapid insulin via 3-way tap for 24-72 hr glucose 5% 500 mL 12 hrly Actrapid insulin 50 units in 50 mL sodium chloride 0.9% (1 unit/mL), at initial rate of 4 units/hr After 1 hr check capillary glucose (Medisense), chart result, and use Table 2 to adjust infusion rate, aiming for capillary glucose 7-10 mmol/L Repeat capillary glucose hrly after each change of infusion rate, otherwise 2 hrly. Chart all results
Table 2: Capillary glucose vs Actrapid infusion rate Capillary glucose Actrapid (units/hr = mL/hr) (mmol/L) >15 6 11-14.9 5 7-10.9 3 4-6.9 1 <4 Stop insulin infusion Give glucose 20% 50 mL IV into large vein Test capillary glucose every 15 min Recommence insulin when capillary glucose >7 mmol/L Repeat plasma potassium at 6, 12 and 24 hr after starting infusions and immediately in event of a clinically significant cardiac arrhythmia In patients with normal renal function but with plasma potassium <4.5 mmol/L, replace the 500 mL bag of glucose 5% by a 500 mL pre-mixed bag of glucose 5% with potassium chloride 20 mmol 12 hrly Always use commercially produced pre-mixed bags of infusion fluid. NEVER add potassium chloride to infusion bags When capillary glucose stable between 4-10.9 mmol/L for at least 24 hr, substitute SC insulin, as follows: add up total insulin requirement during 24 hr of normoglycaemia divide into four equal doses give three of the doses as soluble insulin SC (e.g. Actrapid,/Humulin S), giving one dose before breakfast, lunch and evening meal and fourth dose as Isophane insulin SC (e.g. Insulatard/Humulin I) at 2130 hr
SUBSEQUENT MANAGEMENT
Aspirin 75 mg orally daily (to be continued indefinitely) Clopidogrel 75 mg orally daily for one year Bisoprolol 2.5 mg orally daily, or atenolol 25 mg 12 hrly (to be continued indefinitely, if tolerated) If no clinical suspicion of significant mitral/aortic stenosis or hypertrophic cardiomyopathy, plasma creatinine <300 mol/L and there is no other contraindication to using ACE inhibitor, start ramipril see Prescribing regimens and nomograms. Check electrolytes on day 3-5 Check statin has been prescribed, according to renal function (atorvastatin 40-80 mg) give patient information sheet If pain persistent, consider glyceryl trinitrate (GTN) infusion see Prescribing regimens and nomograms, or further dose atenolol 5 mg IV if heart rate >70 beats/min and systolic BP >100 mmHg If pain persists, contact duty cardiology team
Acute MI 2009-10
Unless complications ensue, recommend early return to physical activity: Day 1 bed rest Day 2 sit out of bed Day 3-4 walk round and to toilet Day 5 extend walking distance and try stairs Refer all patients to rehabilitation co-ordinator, who will arrange an early exercise test for all suitable patients as soon as practically possible after discharge and prior to entering rehabilitation programme Patients not wishing to join rehabilitation programme should receive appropriate dietary advice Refer all patients treated with glucose and insulin infusions to diabetes nurse specialist
MONITORING TREATMENT
Continuous ECG monitoring for 24-48 hr (longer if continuing instability or arrhythmia) Measure BP 4 hrly for 24 hr, then twice daily Daily 12-lead ECG. Plasma CK and AST on two consecutive days, unless troponin T already positive Observe for specific complications (more likely to occur if patients not thrombolysed or otherwise reperfused)
Arrhythmias See Cardiac arrhythmias guideline Cardiac failure See algorithm In patients with left ventricular failure (LVF) or impaired LV function, introduce an ACE inhibitor as soon as this is practical see Acute cardiac failure guideline Arrange echocardiogram as out-patient in patients with significant LVF and/or anterior Q wave infarct, to document LV function and exclude LV aneurysm and/or thrombus Pericarditis More likely after large infarcts Pain with persistent/intermittent pericardial rub two to five days after infarction Adequate analgesia (may need diamorphine). Give indometacin 25 mg orally 8 hrly if no contraindication (beware fluid retention and antagonism of loop diuretic) Recurrent ischaemic pain Isosorbide mononitrate SR orally (GTN infusion if necessary see Prescribing regimens and nomograms If persistent chest pain occurs, refer to duty cardiology team for consideration of in-patient stress testing, coronary angiography and possible angioplasty If re-infarction occurs during admission, contact duty cardiology team immediately
Acute MI 2009-10 Management of cardiac failure after acute MI
No Significant arrhythmia? Yes
See Cardiac arrhythmias guideline
No
New systolic murmur?
Yes
Echocardiography/Doppler ultrasound for ventricular septal defect and mitral regurgitation
No
Warm and well perfused?
Yes
Basal crackles >10 cm
Furosemide Consider ACE inhibitor No Basal crackles? Yes
No
Inferior MI?
Yes Consider right ventricular infarct: Swan-Ganz catheter and fluid repletion may be required
No
BP >90 mmHg systolic?
Yes
Poor prognosis: Consider SwanGanz catheter and IV dobutamine/ dopamine Consider balloon pump
Give furosemide and IV GTN Consider ACE inhibitor
Acute MI 2009-10
DISCHARGE AND FOLLOW-UP
If no complications, discharge home on day 5-7 Check risk factors for recurrent MI (e.g. smoking, hyperlipidaemia, hypertension, obesity) and advise or treat accordingly (mortality in first two years is doubled in those who continue to smoke and is 3.5-times greater if total cholesterol >6.5 mmol/L) Explain graded return to full activity (see advice booklet) Where appropriate, ensure,patient has climbed stairs to assess for chest pain/shortness of breath Ensure advice booklet and chest pain alert card have been issued If taking atorvastatin, ensure GP letter regarding intensive statin therapy accompanies patient on discharge Warn about post-infarct angina Ensure GTN 500 microgram tablets for sublingual use have been prescribed TTO and patient has been counselled on use Advise not to drive for four weeks and check with insurer (Group 2 drivers must notify DVLA, taxi drivers must notify local council) Ensure referral has been made to cardiac rehabilitation team: Check that rehabilitation plan has been made Middle grade in cardiology will review patients who attend as an out-patient at cardiac rehabilitation. Rehabilitation co-ordinator will arrange If patient declines cardiac rehabilitation or is unsuitable for programme, refer to cardiology follow-up clinic Check that follow-up has been arranged in diabetic clinic for all patients treated with glucose and insulin infusions
Follow-up clinic visit Ask about smoking, exercise and weight reduction Ask about angina if occurring, consider referral for angiography Look for signs of heart failure and measure BP Check cholesterol If patient has not been to catheter lab, consider treadmill exercise Encourage return to work one to three months after infarction Resume driving one month after infarction (except Group 2 drivers) Unless there are contraindications, all patients should be taking the following treatment: STEMI: ACE inhibitor statin therapy beta blocker aspirin clopidogrel (28 days, unless drug eluting stent then 1 year) NSTEMI: ACE inhibitor statin therapy beta blocker aspirin clopidogrel (1 year)
S-ar putea să vă placă și
- ACLS PharmacologyDocument6 paginiACLS PharmacologyEunice Angela Fulgueras80% (5)
- TEFL Entrance ExamDocument3 paginiTEFL Entrance ExammerekÎncă nu există evaluări
- AC7140 Rev CDocument73 paginiAC7140 Rev CRanga100% (1)
- Thrombolytic TherapyDocument16 paginiThrombolytic TherapyAnonymous nrZXFwÎncă nu există evaluări
- Advanced Cardiovascular Life Support (ACLS)Document73 paginiAdvanced Cardiovascular Life Support (ACLS)maya_fitrianaÎncă nu există evaluări
- TPA Protocol: Stroke in Carefully Selected PersonsDocument4 paginiTPA Protocol: Stroke in Carefully Selected PersonsJavier Gonzalez, M.D. DABEMÎncă nu există evaluări
- Fac Thrombolysis 2007Document36 paginiFac Thrombolysis 2007Tri Harjono0% (1)
- Paracetamol ToxicictyDocument32 paginiParacetamol ToxicictyWasim R. IssaÎncă nu există evaluări
- ACLS DrugsDocument16 paginiACLS Drugstostc100% (2)
- Antiplatelet Therapy For Acute StrokeDocument10 paginiAntiplatelet Therapy For Acute StrokeInstalasi OK RSI JombangÎncă nu există evaluări
- Main Stroke Protocol - Use For All Suspected Stroke-TIA PatientsDocument2 paginiMain Stroke Protocol - Use For All Suspected Stroke-TIA PatientsRivulet1Încă nu există evaluări
- Tatalaksana STEMI: Rizky Ramadhan N, DR RS Jampang KulonDocument17 paginiTatalaksana STEMI: Rizky Ramadhan N, DR RS Jampang KulonRizky Ramadhan NuriaÎncă nu există evaluări
- Acute Coronary Syndrome 2022Document38 paginiAcute Coronary Syndrome 2022Anonymous100% (1)
- Treatment MGRDocument12 paginiTreatment MGRMod AntbugÎncă nu există evaluări
- Unfractionate Heparin Low Molecular Weight HeparinDocument3 paginiUnfractionate Heparin Low Molecular Weight HeparinArun KumarÎncă nu există evaluări
- Mechanical ThrombectomyDocument58 paginiMechanical Thrombectomyres.uditacharyaÎncă nu există evaluări
- Most of Cardiac Care Unit (C.C.U) DrugsDocument57 paginiMost of Cardiac Care Unit (C.C.U) DrugsOsama OmarÎncă nu există evaluări
- Strokes Student HandoutDocument4 paginiStrokes Student HandoutMiss LindiweÎncă nu există evaluări
- Acute Coronary Syndrome (ACS) : Basic Principles For ACSDocument4 paginiAcute Coronary Syndrome (ACS) : Basic Principles For ACSRendra DananjayaÎncă nu există evaluări
- Myocardial InfarctionDocument20 paginiMyocardial InfarctionRio Ramon HilarioÎncă nu există evaluări
- Protocol For Intensive Intravenous Insulin Infusion For ICUDocument2 paginiProtocol For Intensive Intravenous Insulin Infusion For ICUburlacuraduuÎncă nu există evaluări
- Anticoagulation Monitoring Hand-OutDocument69 paginiAnticoagulation Monitoring Hand-OutApril OcampoÎncă nu există evaluări
- Anticoagulation Protocol For PostDocument8 paginiAnticoagulation Protocol For PostMohammed IbrahimÎncă nu există evaluări
- Anticoagulant Pocket GuideDocument8 paginiAnticoagulant Pocket GuideDrew John Minardi100% (2)
- Target Range For Glycemic Control: 80-140 MG/DL (Generally 110 MG/DL)Document3 paginiTarget Range For Glycemic Control: 80-140 MG/DL (Generally 110 MG/DL)Otchi Pudtrie Wijaya100% (1)
- AclsDocument73 paginiAclsKamel Hady50% (2)
- Ventura County Medical Center: Mi Thrombolysis, Management ofDocument3 paginiVentura County Medical Center: Mi Thrombolysis, Management ofblackcat657Încă nu există evaluări
- Management of Acute Ischemic Stroke (AIS) DR GaneshDocument69 paginiManagement of Acute Ischemic Stroke (AIS) DR GaneshDr Ganeshgouda MajigoudraÎncă nu există evaluări
- CCU HandoverDocument9 paginiCCU Handoverapi-192342497Încă nu există evaluări
- STEMI Extensive Anterior Wall Onset 4 Hours Killip I TIMI Score 3-14Document28 paginiSTEMI Extensive Anterior Wall Onset 4 Hours Killip I TIMI Score 3-14Akbar IskandarÎncă nu există evaluări
- Pharmacy TeachingDocument22 paginiPharmacy TeachingDavid FlynnÎncă nu există evaluări
- Management of ArrhythmiasDocument4 paginiManagement of ArrhythmiasAray Al-AfiqahÎncă nu există evaluări
- Afib Flowchart 1-21 SLWDocument3 paginiAfib Flowchart 1-21 SLWIndra WijayaÎncă nu există evaluări
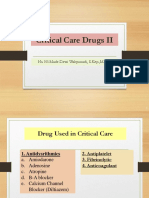
- Critical Care Drugs 2Document23 paginiCritical Care Drugs 2Asri Ernadi100% (1)
- Acute Coronary SyndromeDocument41 paginiAcute Coronary SyndromeAbdulhameed MohamedÎncă nu există evaluări
- Esc Acs GuidelinesDocument62 paginiEsc Acs GuidelineszakiyaÎncă nu există evaluări
- Aha/Asa 2018 Guidelines For The Early Management of Patients With Acute Ischemic StrokeDocument4 paginiAha/Asa 2018 Guidelines For The Early Management of Patients With Acute Ischemic StrokeFrancisco PuenteÎncă nu există evaluări
- Anticoag GuidelinesDocument22 paginiAnticoag Guidelinesyusuf100% (1)
- An Update Management of Acute Ischemic Stroke: SurotoDocument36 paginiAn Update Management of Acute Ischemic Stroke: SurotoShinta DianÎncă nu există evaluări
- Acute Coronary SyndrommeDocument50 paginiAcute Coronary SyndrommeAndriani Kemala SariÎncă nu există evaluări
- Medicine ManagementsDocument87 paginiMedicine ManagementsMohamed LibanÎncă nu există evaluări
- Cardio BBDocument73 paginiCardio BBايات عبدالرحمنÎncă nu există evaluări
- Enoxaparin Sodium Injection I.PDocument15 paginiEnoxaparin Sodium Injection I.PSuhailansariÎncă nu există evaluări
- 1210 DIASTOLIC HypertensionDocument44 pagini1210 DIASTOLIC HypertensionBoysz TheBestÎncă nu există evaluări
- Management of Coronary Heart DDocument12 paginiManagement of Coronary Heart DelisdaÎncă nu există evaluări
- Protocol For in Patient Status Epilepticus in Adults (Includes Convulsive and Non-Convulsive Status Epilepticus)Document3 paginiProtocol For in Patient Status Epilepticus in Adults (Includes Convulsive and Non-Convulsive Status Epilepticus)BarneyÎncă nu există evaluări
- Acetaminophen ToxicityDocument16 paginiAcetaminophen ToxicityMohil PratapÎncă nu există evaluări
- Entresto Prescribing InformationDocument3 paginiEntresto Prescribing InformationLabontu IustinaÎncă nu există evaluări
- 12 Hours: Continue To Monitor: High-Risk NSTEACSDocument1 pagină12 Hours: Continue To Monitor: High-Risk NSTEACSMeita ReligiaÎncă nu există evaluări
- CHC-PC-0033: Procedure Number Version NosDocument7 paginiCHC-PC-0033: Procedure Number Version NosQari Ramadhan AminÎncă nu există evaluări
- Clozapine Monitoring GuidelinesDocument3 paginiClozapine Monitoring GuidelinesAntoine JusticeÎncă nu există evaluări
- Blackshear - Chest Pain ContrastDocument13 paginiBlackshear - Chest Pain ContrastMazen SalamaÎncă nu există evaluări
- Induced HPDocument4 paginiInduced HPmaddythedocÎncă nu există evaluări
- 1 RBH Icu Insulin Guidelines May 2009Document6 pagini1 RBH Icu Insulin Guidelines May 2009bastarduniverseÎncă nu există evaluări
- Pocket Card - Alteplase Injection For Acute Ischemic Events - September 2021Document5 paginiPocket Card - Alteplase Injection For Acute Ischemic Events - September 2021Natalia OrtizÎncă nu există evaluări
- Af NoteDocument6 paginiAf NoteMohammed SadoonÎncă nu există evaluări
- TCA PoisoningDocument4 paginiTCA PoisoningaayceeÎncă nu există evaluări
- Q1. What Is JDBC? Explain Different Types JDBC Drivers With Suitable DiagramDocument64 paginiQ1. What Is JDBC? Explain Different Types JDBC Drivers With Suitable DiagramjyebbwycqmfkuxÎncă nu există evaluări
- UV-Visible Systems - Operational Qualification - Col23 PDFDocument10 paginiUV-Visible Systems - Operational Qualification - Col23 PDFIsabelle PlourdeÎncă nu există evaluări
- Review of Related Literature and Related StudiesDocument23 paginiReview of Related Literature and Related StudiesReynhard Dale100% (3)
- Machine DesignDocument627 paginiMachine DesignlucarÎncă nu există evaluări
- 7094 Bangladesh Studies: MARK SCHEME For The May/June 2011 Question Paper For The Guidance of TeachersDocument11 pagini7094 Bangladesh Studies: MARK SCHEME For The May/June 2011 Question Paper For The Guidance of Teachersmstudy123456Încă nu există evaluări
- Geography Paper 1Document7 paginiGeography Paper 1Sudhir TewatiaÎncă nu există evaluări
- Check List For Design Program of A Parish ChurchDocument11 paginiCheck List For Design Program of A Parish ChurchQuinn HarloweÎncă nu există evaluări
- Day 1 Training Material FlowDocument200 paginiDay 1 Training Material FlowGhazouani AymenÎncă nu există evaluări
- K To 12 Math 7 Curriculum Guide PDFDocument15 paginiK To 12 Math 7 Curriculum Guide PDFEdmar Tan Fabi100% (1)
- Thom22e ch03 FinalDocument44 paginiThom22e ch03 FinalDionisius AlvianÎncă nu există evaluări
- Haldex Valve Catalog: Quality Parts For Vehicles at Any Life StageDocument108 paginiHaldex Valve Catalog: Quality Parts For Vehicles at Any Life Stagehoussem houssemÎncă nu există evaluări
- Sample Engagement LetterDocument5 paginiSample Engagement Letterprincess_camarilloÎncă nu există evaluări
- Clepsydra - PesquisaDocument2 paginiClepsydra - PesquisaJose Maria SantosÎncă nu există evaluări
- Rise of Al JazeeraDocument1 paginăRise of Al Jazeeraইlish ProductionsÎncă nu există evaluări
- Lecture 5: Triangulation Adjustment Triangulation: in This Lecture We Focus On The Second MethodDocument5 paginiLecture 5: Triangulation Adjustment Triangulation: in This Lecture We Focus On The Second MethodXogr BargarayÎncă nu există evaluări
- Hazop Close Out ReportDocument6 paginiHazop Close Out ReportKailash PandeyÎncă nu există evaluări
- Classical School of Thought: Ms. Salma ShaheenDocument62 paginiClassical School of Thought: Ms. Salma ShaheenQasim Ali100% (1)
- List of Famous Cities On River Banks in The WorldDocument2 paginiList of Famous Cities On River Banks in The WorldDiptangshu DeÎncă nu există evaluări
- Towards A Brighter Ecological Future: Group 2Document24 paginiTowards A Brighter Ecological Future: Group 2As YangÎncă nu există evaluări
- Et200sp Im 155 6 PN ST Manual en-US en-USDocument47 paginiEt200sp Im 155 6 PN ST Manual en-US en-USayaz officeÎncă nu există evaluări
- Research Paper Effect of Mobile Banking On Customer-823Document11 paginiResearch Paper Effect of Mobile Banking On Customer-823amittaneja28Încă nu există evaluări
- 2 Beats Per Measure 3 Beats Per Measure 4 Beats Per MeasureDocument24 pagini2 Beats Per Measure 3 Beats Per Measure 4 Beats Per MeasureArockiya StephenrajÎncă nu există evaluări
- Pe8 Mod5Document16 paginiPe8 Mod5Cryzel MuniÎncă nu există evaluări
- Biography of Anna HazareDocument4 paginiBiography of Anna HazareGenesis FirstÎncă nu există evaluări
- I - Pronunciation Choose The Word Whose Stress Pattern Is Different From The Other Three in The Following QuestionsDocument6 paginiI - Pronunciation Choose The Word Whose Stress Pattern Is Different From The Other Three in The Following QuestionsHaÎncă nu există evaluări
- SET UP Computer ServerDocument3 paginiSET UP Computer ServerRicHArdÎncă nu există evaluări
- NCP81205Document1 paginăNCP81205Tom TomÎncă nu există evaluări
- Pu3-Mo A1 MoversDocument40 paginiPu3-Mo A1 MoversMiss María José SalasÎncă nu există evaluări