Documente Academic
Documente Profesional
Documente Cultură
Systemic Lupus Erythematosus (SLE)
Încărcat de
Daniel MazariegoDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Systemic Lupus Erythematosus (SLE)
Încărcat de
Daniel MazariegoDrepturi de autor:
Formate disponibile
Systemic Lupus Erythematosus (SLE)
The manifestations are protean, and there is no characteristic or pathognomonic finding. Instead, this disease is diagnosed by finding suggestive serologic and clinical findings. Findings may include:
Skin rash - malar or discoid Sensitivity to light (photodermatitis) Serositis - inflammation of serosal surfaces along with effusions Glomerulonephritis - the worst problem with SLE Cytopenias - anemia, leukopenia, thrombocytopenia Antinuclear antibody - rim pattern, anti double stranded-DNA and anti-Smith autoantibodies are most specific for SLE Arthralgias, myalgias Vasculitis - anywhere: CNS, skin, kidney, etc Decreased serum complement - especially C1q Thrombosis - in arteries or veins
Genetic factors: tends to run in families; association with HLA Dr-2 and Dr-3; more common in young women (especially African-American). Drugs can produce "drug-induced" SLE: list includes procainamide, hydralazine, isoniazid, d-penicillamine. Discoid lupus erythematosus (DLE): a benign disease with skin involvement; ANA positive in only a third (but some of these go on to SLE).
Scleroderma (Progressive Systemic Sclerosis, PSS)
Characterized by excessive fibrosis in a variety of tissues from collagen deposition by activated fibroblasts. About 75% of cases are in women, mostly middle aged. Patterns of disease include: Limited scleroderm, or CREST syndrome: the benign form of PSS, serologically suggested by the presence of anti-centromere antibody
C = Calcinosis in skin and elsewhere R = Raynaud's phenomenon, sensitivity to cold E = Esophageal dysmotility from submucosal fibrosis S = Sclerodactyly from dermal fibrosis T = Telangiectasias
Diffuse scleroderma: the worst form of PSS; Scl-70 (anti-DNA topoisomerase I) antibody shows specificity for this form. It may include all of the findings with CREST, but additionally has renal findings: arterial intimal thickening and proliferation (hyperplastic arteriolosclerosis) leading to malignant hypertension with arterial fibrinoid necrosis, thrombosis, and renal infarction. Half of diffuse PSS patients die from renal disease. The lungs in this form of scleroderma may have diffuse alveolar fibrosis leading to honeycomb fibrosis
Morphea: this is skin fibrosis only
Polymyositis-Dermatomyositis
Characterized by inflammation of skeletal muscle with weakness. Sometimes it is associated with a skin rash (hence, dermatomyositis). It is seen in ages 40-60, but also in ages 5-15, mostly in women. Some of these patients have Jo-1 antibody. Inflammation in polymyositis is mainly mediated by cytotoxic CD8 cells. In dermatomyositis, mainly antigen-antibody complexes produce a vasculitis in muscle and skin. Some adults (1020%) develop cancer.
Sjogren's Syndrome
Characterized by dry eyes and dry mouth as a result of lacrimal and salivary gland involvement by lymphocytic infiltration, fibrosis, and destruction mediated by CD4+ cells helping antibody production, of which anti-SS-A and anti-SS-B are the most specific. Most patients are middle to older age women. Lacrimal and salivary gland inflammation of any cause (including Sjogren's) is called Mikulicz's syndrome.
PRIMARY IMMUNODEFICIENCY SYNDROMES
X-linked Agammaglobulinemia of Bruton
Congenital agammaglobulinemia (Bruton's Disease) results from a genetic defect on the long arm of X chromosome, so that males are primarily affected (inheritance occurs in an X-lined recessive pattern). The mutations affect production of a tyrosine kinase (Bruton tyrosine kinase, or btk) active in early pre-B cells which diminishes their maturation and leads to virtual absence of all immunoglobulin classes. Infants are observed to have multiple infections with bacterial organisms (Hemophilus, Staphylococcus), particularly in skin and lung. Agammaglobulinemia is the result of absent B-cells, but T-cell mediated immunity is intact. If affected persons survive, many will develop autoimmune diseases.
Common Variable Immunodeficiency
This is a heterogenous group of disorders with an incidence of 1 per 100,000 that can involve both humoral and cell mediated immunity. Though there are normal numbers of circulating B lymphocytes, there is impaired secretion of one or more immunoglobulin isotypes, usually IgG or IgA. A selective abnormality of T cell activation, as demonstrated by decreased synthesis of interleukins (IL 2, 4, and 5) has been identified. Patients may have impaired gastrointestinal mucosal immunity. Another variant results from either a decrease in CD4 cells or an increase in CD8 cells. Also occuring is a variant resulting from the presence of T and B lymphocyte autoantibodies. At least two of the three main serum immunoglobulin isotypes are decreased. Persons with CVID are prone to recurrent bacterial infections, particularly sinusitis, bronchitis, pneumonia, bronchiectasis, and otitis. Bordatella pertussis infections occur in childhood. Viral infections are uncommon, though recurrent herpes simplex with eventual herpes zoster is an exception. Giardiasis is common. Half of CVID cases are diagnosed before age 21, but in some cases complications do not develop until adolescence or adulthood.
There is an increased incidence of autoimmune diseases, particularly hemolytic anemia, thrombocytopenia, and pernicious anemia. In about two thirds of cases, normal numbers of circulating B lymphocytes are present. There is a decrease in immunoglobulins, generally in all classes, more often IgG and IgA, but sometimes only of IgG.
DiGeorge Syndrome
The DiGeorge syndrome (or sequence) is a field defect of third and fourth pharyngeal pouch development in utero during organogenesis in the first trimester of pregnancy. A specific deletion on the long arm of chromosome 22 has been implicated. Anatomic structures that may be aplastic or hypoplastic include the thymus, parathyroid glands, great vessels, and esophagus. DiGeorge syndrome may be further subclassified as complete, in which there is almost total absence of thymic tissue, or as partial, in which there is only a decrease in thymic tissue Complete DiGeorge syndrome is characterized by normal levels of circulating immunoglobulin, though in some cases serum IgE is increased and IgA is decreased. However, affected children have markedly decreased numbers of circulating T lymphocytes, making them susceptible to fungal and viral infections. Children with partial DiGeorge syndrome have only a slight decrease in peripheral T lymphocytes and have increased infections, but with less frequency and with less severity than children with the complete form. Accompanying aplasia of parathyroid glands can lead to lifethreatening hypocalcemia that may appear soon after birth.
Severe Combined Immunodeficiency (SCID)
SCID results from different defects with different inheritance patterns, but all demonstrate some degree of failure in development of both humoral and cell-mediated immunity. The major variants of SCID include:
An X-linked form is due to a mutation on the long arm of the X chromosome which produces a defective gamma chain of the interleukin-2 receptor (cytokine receptor). Lacking an intact interleukin receptor renders early lymphocytes incapable of normal differentiation and development to functional T and B cells in response to growth factors. This form accounts for about 60% of cases. Autosomal recessive inheritance linked to a lack of the enzyme adenosine deaminase (ADA) leads to about 35 to 40% of cases. The ADA enzyme is involved in purine metabolism, and its deficiency results in production of metabolites toxic to lymphocytes
There tends to be a greater decrease in cell mediated immunity than in humoral immunity. Normal or increased numbers of B lymphocytes may be present with the X-linked form, but these cells still do not function properly. There is very little serum IgG and virtually no IgM or IgA. Infants develop Candida skin rashes and thrush, persistent diarrhea, severe respiratory tract infections with Pneumocystis carinii and Pseudomonas soon after birth, and failure to thrive after 3 months of age. Severe viral can occur. Maternal T lymphocytes crossing the placenta may produce graft versus host disease
Wiskott-Aldrich Syndrome
An X-linked recessive pattern is seen because the defective gene is located on the short arm of the X chromosome (Xp11.23). The immunodeficiency is accompanied by thrombocytopenia and eczema. Circulating platelets are markedly decreased. T lymphocytes exhibit cytoskeletal disorganization and loss of microvilli by electron microscopy, and they express little CD43 by immunohistochemical staining. There is usually a normal level of serum IgG, along with a decrease in IgM, but often an increase in both IgA and IgE. The initial onset of disease in early childhood is accompanied by recurrent bacterial infections, particularly to encapsulated bacteria such as Streptococcus pneumoniae, with development of pneumonia, meningitis, and septicemia. Later, failure of T lymphocyte function may predispose to recurrent herpetic infections and to Pneumocystis carinii pneumonia. A bleeding problem may result from the severe thrombocytopenia.
Ataxia-Telangiectasia
A genetic defect is present on the long arm of chromosome 11 which predisposes to chromosome breakage and rearrangement, particularly on chromosomes 7 and 14, leading to a high risk for neoplasia and a marked sensitivity to radiation. This disorder is quite rare and has an autosomal recessive pattern of inheritance. There is a triad of progressive cerebellar ataxia, mucocutaneous telangiectasias, and recurrent respiratory tract infections with a variety of bacterial and fungal organisms. Immunoglobulin deficiencies, particularly IgA and/or IgE, may be present, though serum IgM is usually elevated. The symptoms usually begin between 9 months and 2 years of age.
Selective IgA Deficiency
About 1 in 600 persons of European descent has a virtual lack of circulating IgA as well as secretory IgA which, in most cases, results from failure of the IgA type of B lymphocytes to transform into plasma cells capable of producing IgA or from impaired survival of IgA producing plasma cells. Some patients may have deficiencies in IgG subclasses 2 and/or 4, while IgG subclasses 1 and 3 are increased. Some patients go on to develop common variable immunodeficiency, suggesting that there is a similar defect in B cell maturation and function. Some affected patients are at increased risk for respiratory, gastrointestinal, and urinary tract infections, most often bacterial, and diarrhea is common. More severely affected persons may even have a sprue-like illness with malabsorbtion. Atopy, as demonstrated by asthma, can be present. Concomitant autoimmune diseases, particularly systemic lupus erythematosus and rheumatoid arthritis, can be present. About half of IgA deficient persons develop anti-IgA antibodies of the IgE type, so that transfusion of blood products containing serum with normal IgA levels leads to severe systemic anaphylaxis.
Other Primary Immunodeficiency Disorders
Deficiencies of other components of the immune system are uncommon. Some of the best known are:
Complement component deficiencies: C2 deficiency carries a risk for development of autoimmune disease. C3 deficiency is associated with recurrent bacterial infections. Chediak-Higashi syndrome: A rare autosomal recessive disorder in which peripheral blood neutrophils, monocytes, and lymphocytes contain giant cytoplasmic granules and patients have leukopenia, making them susceptible to bacterial and fungal infections of skin, mucous membranes, and respiratory tract Chronic granulomatous disease: neutrophils and monocytes lack the enzyme NADPH oxidase which is needed to generate intracellular oxidants that destroy phagocytosed infectious organisms, particularly catalase-positive agents such as Staphylococcus aureus, Candida, and Aspergillus, so that chronic infections are common
S-ar putea să vă placă și
- Fast Facts: Familial Chylomicronemia Syndrome: Raising awareness of a rare genetic diseaseDe la EverandFast Facts: Familial Chylomicronemia Syndrome: Raising awareness of a rare genetic diseaseÎncă nu există evaluări
- Immunology FirecrackerDocument45 paginiImmunology FirecrackerMariam A. KarimÎncă nu există evaluări
- Immunodeficiency Syndromes - Hiv/Aids Infection: DR O.O. WilliamsDocument35 paginiImmunodeficiency Syndromes - Hiv/Aids Infection: DR O.O. Williamsseun williamsÎncă nu există evaluări
- Dermatomyositis Case7Document15 paginiDermatomyositis Case7Hanina Macataman MetmugÎncă nu există evaluări
- Immunodeficiencies by Muskan Mishra FinalDocument40 paginiImmunodeficiencies by Muskan Mishra FinalMuskan MishraÎncă nu există evaluări
- Immune-Deficiency Diseases (2022)Document30 paginiImmune-Deficiency Diseases (2022)malkalhmaidh03Încă nu există evaluări
- IMS - Immunomodulation & ImmunodeficienciesDocument3 paginiIMS - Immunomodulation & ImmunodeficienciesJeanne RodiñoÎncă nu există evaluări
- SleDocument66 paginiSlebhushan vichareÎncă nu există evaluări
- Disorders of BloodDocument3 paginiDisorders of BloodCondurache Ilie-AndreiÎncă nu există evaluări
- Ple 2015 Board Review May 2015 Patho OnlyDocument10 paginiPle 2015 Board Review May 2015 Patho OnlyMa Katherina ArellanoÎncă nu există evaluări
- Immunodeficiency DisorderDocument14 paginiImmunodeficiency DisorderAaryan PatelÎncă nu există evaluări
- Lecture-3.3.6-Systemic Autoimmune Diseases With Examples-2Document3 paginiLecture-3.3.6-Systemic Autoimmune Diseases With Examples-2aditya sahuÎncă nu există evaluări
- 15 2023 ImmunodeficienciesDocument29 pagini15 2023 ImmunodeficienciesalirezazngneÎncă nu există evaluări
- Immunology AssignmentDocument27 paginiImmunology AssignmentShadma KhanÎncă nu există evaluări
- 5 Immunodeficiency DisordersDocument37 pagini5 Immunodeficiency Disorderswanda murielÎncă nu există evaluări
- Systemic SclerosisDocument36 paginiSystemic SclerosisrgardónÎncă nu există evaluări
- Impaired ImmunityDocument2 paginiImpaired ImmunityMikee AmagsilaÎncă nu există evaluări
- Diseases of Immune System Part 2Document47 paginiDiseases of Immune System Part 2KundaÎncă nu există evaluări
- Immune DeficiencyDocument18 paginiImmune DeficiencyDr anas AbdullahÎncă nu există evaluări
- Disorders of The Immune System ImmunityDocument7 paginiDisorders of The Immune System ImmunityMarinelle TumanguilÎncă nu există evaluări
- Immuno DeficienciesDocument13 paginiImmuno DeficienciesNikhil TyagiÎncă nu există evaluări
- bt302 Mid & Final Term NotesDocument58 paginibt302 Mid & Final Term NotesFarogh e HaqÎncă nu există evaluări
- Blok Imunohematologi: Praktikum Patologi AnatomiDocument24 paginiBlok Imunohematologi: Praktikum Patologi AnatomininisÎncă nu există evaluări
- ANA TestDocument9 paginiANA TestNena_mileyÎncă nu există evaluări
- Immunodeficiency DiseasesDocument19 paginiImmunodeficiency DiseasesZaheer Abbas ChannaÎncă nu există evaluări
- Severe Combined Immunodeficiency 06-02-08Document11 paginiSevere Combined Immunodeficiency 06-02-08Manisanthosh KumarÎncă nu există evaluări
- Department of Internal Medicine Iii Hemorrhagic Syndromes: - Rajkumar Subasaravanan Subgroup "12"Document122 paginiDepartment of Internal Medicine Iii Hemorrhagic Syndromes: - Rajkumar Subasaravanan Subgroup "12"Suba Saravanan 12Încă nu există evaluări
- 6 - Immune Deficiency Diseases 2Document8 pagini6 - Immune Deficiency Diseases 2Belle Galao GepteÎncă nu există evaluări
- Di George Syndrome-6 - 1Document6 paginiDi George Syndrome-6 - 1usamas85556Încă nu există evaluări
- بحث immunodeficiency disorder2Document25 paginiبحث immunodeficiency disorder2suqylÎncă nu există evaluări
- Immune Deficincies - SarahDocument10 paginiImmune Deficincies - SarahkhaledÎncă nu există evaluări
- Subject Seminar: Primary Immuno Deficiency DisordersDocument83 paginiSubject Seminar: Primary Immuno Deficiency DisordersVarun B RenukappaÎncă nu există evaluări
- Membranous GlomerulonephritisDocument5 paginiMembranous GlomerulonephritisRobertÎncă nu există evaluări
- AutoimmunityDocument8 paginiAutoimmunityRachit NarangÎncă nu există evaluări
- Sle DevDocument10 paginiSle DevDev VithlaniÎncă nu există evaluări
- Objective PEDSDocument58 paginiObjective PEDSlaraÎncă nu există evaluări
- Chapter 28 (Aim Disorders)Document9 paginiChapter 28 (Aim Disorders)Vince Martin ManaigÎncă nu există evaluări
- MRCPCH Guide Heme: A Hypochromic MicrocyticDocument8 paginiMRCPCH Guide Heme: A Hypochromic MicrocyticRajiv KabadÎncă nu există evaluări
- DiGeorge SyndromeDocument18 paginiDiGeorge SyndromeRupesh MohandasÎncă nu există evaluări
- Autoimmune Hepatitis: Mu ViDocument68 paginiAutoimmune Hepatitis: Mu VidrsajusvÎncă nu există evaluări
- Harrison SLEDocument11 paginiHarrison SLEpazucenaÎncă nu există evaluări
- Lecture 03Document30 paginiLecture 03bsmls-f18-017Încă nu există evaluări
- Bloody Gum: First PBL SessionDocument39 paginiBloody Gum: First PBL SessionRathimalar MogarajaÎncă nu există evaluări
- Pediatrics - ImmunodeficiencyDocument3 paginiPediatrics - ImmunodeficiencyJasmine KangÎncă nu există evaluări
- HaematologyDocument25 paginiHaematologyMenziPhiwokuhleSukatiÎncă nu există evaluări
- ImmunodeficiencyDocument33 paginiImmunodeficiencyIqra ShaheenÎncă nu există evaluări
- 8 - Autoimmune DiseasesDocument20 pagini8 - Autoimmune Diseasesvirag.patilÎncă nu există evaluări
- Autoimmune Diseases of The Oral CavityDocument143 paginiAutoimmune Diseases of The Oral CavityMohammed ShaikhÎncă nu există evaluări
- Allergy&Immunology: Irritant Contact Dermatitis (Icd)Document11 paginiAllergy&Immunology: Irritant Contact Dermatitis (Icd)Orlando PiñeroÎncă nu există evaluări
- Photo QuizDocument21 paginiPhoto Quizabas_maytham1021100% (3)
- Patho of Hema Q&aDocument141 paginiPatho of Hema Q&akamaluÎncă nu există evaluări
- Sthapylococcus Selain AureusDocument5 paginiSthapylococcus Selain AureusTotalenesya Reforrent SutiknoÎncă nu există evaluări
- SleDocument33 paginiSleZaira HussainÎncă nu există evaluări
- Hema Patho Q&aDocument24 paginiHema Patho Q&akamaluÎncă nu există evaluări
- Literature ReviewDocument31 paginiLiterature ReviewArdi PratamaÎncă nu există evaluări
- Sigal Immuno DeficiencyDocument61 paginiSigal Immuno DeficiencyClaire HendersonÎncă nu există evaluări
- Immunodeficiency Disorders: DR - Kumaran GanesanDocument58 paginiImmunodeficiency Disorders: DR - Kumaran Ganesanvivek chavhanÎncă nu există evaluări
- Pathology of AnemiaDocument3 paginiPathology of AnemiaNesma AdelÎncă nu există evaluări
- Kidney NewDocument4 paginiKidney NewParth BhayanaÎncă nu există evaluări
- Obstructive Sleep Apnea Case Study: Shirin Shafazand, MD, MS Neomi Shah, MD August 2014Document15 paginiObstructive Sleep Apnea Case Study: Shirin Shafazand, MD, MS Neomi Shah, MD August 2014Vimal NishadÎncă nu există evaluări
- Pharmacology Test 1Document39 paginiPharmacology Test 1Niki BolinÎncă nu există evaluări
- AGAINST COVID Vaccines: Follow Protocol C For at Least 21 Days + Protocol K at The Place of The InjectionDocument11 paginiAGAINST COVID Vaccines: Follow Protocol C For at Least 21 Days + Protocol K at The Place of The Injectionearl-e-birdÎncă nu există evaluări
- Iron-Refractory Iron Deficiency Anemia May Not Lead To Neurocognitive Dysfunction: A Case ReportDocument6 paginiIron-Refractory Iron Deficiency Anemia May Not Lead To Neurocognitive Dysfunction: A Case ReportwitwiiwÎncă nu există evaluări
- Yoga & ArthritisDocument24 paginiYoga & Arthritistttt45Încă nu există evaluări
- DigestionpracticetestDocument41 paginiDigestionpracticetestRennik McCaigÎncă nu există evaluări
- The Sketch of Indonesia Medicine: Sugma AP, MD, MARSDocument42 paginiThe Sketch of Indonesia Medicine: Sugma AP, MD, MARSRaja Friska YulandaÎncă nu există evaluări
- Trauma in Early Childhood: A Neglected PopulationDocument20 paginiTrauma in Early Childhood: A Neglected PopulationFrancisca AldunateÎncă nu există evaluări
- "The Effects of Interpersonal Crime On Victims": Reporter: Michel O. Espinosa Bs-Psychology Code: 3175Document6 pagini"The Effects of Interpersonal Crime On Victims": Reporter: Michel O. Espinosa Bs-Psychology Code: 3175Ezri Mariveles Coda Jr.Încă nu există evaluări
- Home Visit PlanDocument2 paginiHome Visit Planako at ang exoÎncă nu există evaluări
- Contact Nummular (Discoid) Eczema From Depilating Cream: Case ReportDocument2 paginiContact Nummular (Discoid) Eczema From Depilating Cream: Case ReportMorindaÎncă nu există evaluări
- Restoration of The Worn Dentition. Part 2Document7 paginiRestoration of The Worn Dentition. Part 2Isharajini Prasadika Subhashni GamageÎncă nu există evaluări
- Cmca at RiskDocument11 paginiCmca at RiskAyanami PascuaÎncă nu există evaluări
- Breast Cancer - DZMEDocument6 paginiBreast Cancer - DZMEMarife CompraÎncă nu există evaluări
- Hypernatremia From HarrisonDocument3 paginiHypernatremia From HarrisonNobel LaureateÎncă nu există evaluări
- 2014 @nucproflib Helen Ryder, GiorgioDocument128 pagini2014 @nucproflib Helen Ryder, Giorgioe'Rfan k'AguyaÎncă nu există evaluări
- BernottiDocument44 paginiBernottiAlexandra Alexandra100% (2)
- Existing Restoration - Clinical Status: Secondary Caries Marginal Integrity Biomechanical FormDocument47 paginiExisting Restoration - Clinical Status: Secondary Caries Marginal Integrity Biomechanical FormDaniel WangÎncă nu există evaluări
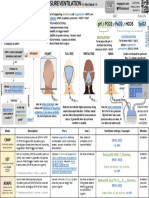
- ICU One Pager NIPPVDocument1 paginăICU One Pager NIPPVNicholas HelmstetterÎncă nu există evaluări
- Upper GI Drugs (Pod Pharm 2023, Thatcher)Document39 paginiUpper GI Drugs (Pod Pharm 2023, Thatcher)8jm6dhjdcpÎncă nu există evaluări
- Cumulative Trauma DisordersDocument70 paginiCumulative Trauma DisordersBishal BistaÎncă nu există evaluări
- بنك الأسئلةDocument775 paginiبنك الأسئلةسماح صلاح100% (1)
- DdaDocument7 paginiDdahasyimahÎncă nu există evaluări
- GTG 37bDocument32 paginiGTG 37bKadelsy BristolÎncă nu există evaluări
- Grand Halad Sa Kapamilya: List of ServicesDocument2 paginiGrand Halad Sa Kapamilya: List of ServicesLeo LastimosaÎncă nu există evaluări
- Dietician Referral Ms SmithDocument3 paginiDietician Referral Ms SmithPrasoon Premraj0% (1)
- Patient Case PresentationDocument7 paginiPatient Case Presentationapi-613861196Încă nu există evaluări
- European Journal of Cardiovascular Prevention & Rehabilitation-2008-Binder-726-34Document9 paginiEuropean Journal of Cardiovascular Prevention & Rehabilitation-2008-Binder-726-34Julio Cesar TakeharaÎncă nu există evaluări
- Oral and Maxillofacial SurgeryDocument22 paginiOral and Maxillofacial SurgeryafheaÎncă nu există evaluări
- FCPS SurgeryDocument106 paginiFCPS Surgeryrehan hayderÎncă nu există evaluări
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)De la EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Evaluare: 3 din 5 stele3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDe la EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionEvaluare: 4 din 5 stele4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDe la EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsÎncă nu există evaluări
- The Age of Magical Overthinking: Notes on Modern IrrationalityDe la EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityEvaluare: 4 din 5 stele4/5 (32)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDe la EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisEvaluare: 4.5 din 5 stele4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDe la EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDEvaluare: 5 din 5 stele5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDe la EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeEvaluare: 2 din 5 stele2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDe la EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedEvaluare: 4.5 din 5 stele4.5/5 (82)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDe la EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryEvaluare: 4 din 5 stele4/5 (46)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDe la EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDe la EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsEvaluare: 4 din 5 stele4/5 (4)
- The Obesity Code: Unlocking the Secrets of Weight LossDe la EverandThe Obesity Code: Unlocking the Secrets of Weight LossEvaluare: 4 din 5 stele4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesDe la EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesEvaluare: 4.5 din 5 stele4.5/5 (1412)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDe la EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsEvaluare: 5 din 5 stele5/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.De la EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Evaluare: 4.5 din 5 stele4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDe la EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityEvaluare: 4 din 5 stele4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDe la EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsEvaluare: 4.5 din 5 stele4.5/5 (170)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDe la EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisEvaluare: 5 din 5 stele5/5 (8)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDe la EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisEvaluare: 3.5 din 5 stele3.5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDe la EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessEvaluare: 4.5 din 5 stele4.5/5 (328)
- Troubled: A Memoir of Foster Care, Family, and Social ClassDe la EverandTroubled: A Memoir of Foster Care, Family, and Social ClassEvaluare: 4.5 din 5 stele4.5/5 (27)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingDe la EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingEvaluare: 4 din 5 stele4/5 (1138)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDe la EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeEvaluare: 4.5 din 5 stele4.5/5 (254)