Documente Academic
Documente Profesional
Documente Cultură
Managing Co-Morbidities in End of Life Care - DR Lim Zee Nee Revised
Încărcat de
malaysianhospicecouncil6240Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Managing Co-Morbidities in End of Life Care - DR Lim Zee Nee Revised
Încărcat de
malaysianhospicecouncil6240Drepturi de autor:
Formate disponibile
Dr Lim Zee Nee MBChB(UK) MRCP(UK) Palliative Care Physician, Hospis Malaysia 2nd June 2012 10th Malaysian
Hospice Congress
Prevalence and types of co-morbidities Impact of co-morbidities Case study General guidance on managing comorbidities at the end of life Conclusion
A case study of 15,626 patients with cancer 1984-1992 in Detroit (Ogle KS 2000et al): 1. 68.7% had co-morbidity 2. 32.6% had 2 co-morbidities 3. Co-morbidity more common in the elderly, smokers, African-American, lower socioeconomic status
COPD
Diabetes Mellitus
Osteoporosis
Co-morbidities
Arthritis
Heart disease Hypercholesterolaemia Hypertension Stroke
Depression Dementia Schizophrenia
World
Deaths in millions 7.25 6.15 3.46 3.28 2.46
% of deaths 12.8% 10.8% 6.1% 5.8% 4.3%
Ischaemic heart disease
Stroke and other cerebrovascular disease Lower respiratory infections Chronic obstructive pulmonary disease Diarrhoeal diseases
HIV/AIDS
Trachea, bronchus, lung cancers Tuberculosis Diabetes mellitus Road traffic accidents
1.78 1.39
1.34 1.26 1.21
3.1% 2.4%
2.4% 2.2% 2.1%
morbidity and mortality Affects clinical presentation of the illness and recognition of clinical syndromes Affects cancer treatment
Both cancer and presence of co-morbidity are independently associated with greater symptom burden Symptom burden with the number of comorbidities
Psychological impact 1. Depression is linked to a variety of comorbidities (21.5% in heart failure, 30% in stroke, 20% in dementia) 2. It is prevalent among cancer patients with multiple co-morbidities
Little guidance for health care professionals Disease-specific / subspecialty care model does not address the complexity of problems encountered at the end of life
Mr. GP, 85 year old gentleman Diagnosed with Lung Cancer, metastases to bone and brain Comorbidities (prior to diagnosis of cancer) 1. Hypertension 2. Ischaemic heart disease (ejection fraction 34%) 3. Stroke 4. Upper GI bleed 5. End stage renal failure (on dialysis for 2 yrs)
Changes take place at the end of life Polypharmacy risk of drug interactions (risk > 80% with > 7 drugs prescribed) Withdrawal of drugs or continuation of drugs may lead to problems
Formulating a prognosis is difficult It improves treatment decision at the end of life Different disease trajectory Different models of prognosis
Murray S A et al. BMJ 2005;330:1007-1011
How does this disease behave with and without intervention ? How does this disease usually progress over time ?
Is the course of the disease (either cancer or comorbidity) influenced by current interventions ? What is the risk of acute deterioration if treatment for co-morbidity is reduced or withdrawn ?
Number needed to treat (NNT) can be used to decide about starting treatment Number needed to harm (NNH) can be used to decide to stop treatment
What is the aim of treating comorbidities ? Primary, secondary or tertiary prevention ? Are we achieving patients goals ? Are we improving or maintaining patients quality of life ?
Feelings of abandonment Fear of complications of the co-morbidity Further confrontation with mortality A sense of futility of previous efforts with compliance
Addressed physical symptoms Addressed patient and familys psychosocial and spiritual issues Assessed for depression Giving information to help improve familys understanding
Conflict resolution finding a common goal Medication benefit versus burden Addressed issue regarding artificial nutrition at the end of life PRN medications prescribed
Multidisciplinary approach to care Nursing care Preferred place of care - at home
Co-morbidity is common in advanced lifethreatening illnesses Assessment has to be individualized and multidimensional in order to achieve treatment decisions at the end of life, taking into considerations the patients goals of care and his quality of life
Management of co-morbidities at the end of life include good symptom control, reducing polypharmacy and addressing any psychosocial and spiritual issues concerning the patient and family
S-ar putea să vă placă și
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (894)
- Heart SoundDocument29 paginiHeart Sounddianpratiwirahim100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- University of Al-Ameed College of Medicine: Hematopathology Lecture PlanDocument226 paginiUniversity of Al-Ameed College of Medicine: Hematopathology Lecture PlanYousif AlaaÎncă nu există evaluări
- Case 4Document5 paginiCase 4Bikash ShresthaÎncă nu există evaluări
- Tah BsoDocument27 paginiTah BsoCephradine DolienteÎncă nu există evaluări
- Nursing Care Plan For AIDS/HIVDocument3 paginiNursing Care Plan For AIDS/HIVderic81% (16)
- The Complete Hematopathology GuideDocument113 paginiThe Complete Hematopathology GuideJenny SÎncă nu există evaluări
- Acute Respiratory Failure For StudentDocument41 paginiAcute Respiratory Failure For Studentapi-379952350% (4)
- PERKENI (2021) - Konsensus DM Tipe 2Document119 paginiPERKENI (2021) - Konsensus DM Tipe 2Ammalia RachmiÎncă nu există evaluări
- Challenges For Care at Home - DR Lim Zee Nee RevisedDocument16 paginiChallenges For Care at Home - DR Lim Zee Nee Revisedmalaysianhospicecouncil6240Încă nu există evaluări
- Continuing Education - DR SylviaDocument35 paginiContinuing Education - DR Sylviamalaysianhospicecouncil6240100% (1)
- Bulletin Jan 2013Document12 paginiBulletin Jan 2013malaysianhospicecouncil6240Încă nu există evaluări
- Bulletin July 2012Document12 paginiBulletin July 2012malaysianhospicecouncil6240Încă nu există evaluări
- Are Elderly Cancer Patients Wrongly Labelled As Palliative - DR Lesley YoungDocument32 paginiAre Elderly Cancer Patients Wrongly Labelled As Palliative - DR Lesley Youngmalaysianhospicecouncil6240Încă nu există evaluări
- Triage in Palliative Care Setting - DR Joseph NinanDocument23 paginiTriage in Palliative Care Setting - DR Joseph Ninanmalaysianhospicecouncil6240Încă nu există evaluări
- Oxygen Concentrator1Document19 paginiOxygen Concentrator1malaysianhospicecouncil6240Încă nu există evaluări
- Wound Management - PCN KrisnaDocument35 paginiWound Management - PCN Krisnamalaysianhospicecouncil6240Încă nu există evaluări
- Stoma Care - PCN KrisnaDocument52 paginiStoma Care - PCN Krisnamalaysianhospicecouncil6240Încă nu există evaluări
- Should PCN Prescribe Drugs - Dato' Seri DR T DevarajDocument16 paginiShould PCN Prescribe Drugs - Dato' Seri DR T Devarajmalaysianhospicecouncil6240Încă nu există evaluări
- Oxy Conc Breathlessness2Document13 paginiOxy Conc Breathlessness2malaysianhospicecouncil6240Încă nu există evaluări
- STATUTORY BENEFITS - WE SHOULD BE PROACTIVE - Dato'Seri DR T DevarajDocument26 paginiSTATUTORY BENEFITS - WE SHOULD BE PROACTIVE - Dato'Seri DR T Devarajmalaysianhospicecouncil6240100% (2)
- Oxy Conc Maintenance3Document11 paginiOxy Conc Maintenance3malaysianhospicecouncil6240Încă nu există evaluări
- Nourishment More Than Nutrition - DR Yeat Choi LingDocument65 paginiNourishment More Than Nutrition - DR Yeat Choi Lingmalaysianhospicecouncil6240Încă nu există evaluări
- Seamless Care - DR SH LeungDocument38 paginiSeamless Care - DR SH Leungmalaysianhospicecouncil6240Încă nu există evaluări
- CARE CENTRES - A ROLE FOR PALLIATIVE CARE - Dato' Seri DR T DevarajDocument29 paginiCARE CENTRES - A ROLE FOR PALLIATIVE CARE - Dato' Seri DR T Devarajmalaysianhospicecouncil6240Încă nu există evaluări
- Palliative Care Delirium - DR Lesley YoungDocument43 paginiPalliative Care Delirium - DR Lesley Youngmalaysianhospicecouncil6240100% (1)
- Caring For Caregivers - DR SylviaDocument25 paginiCaring For Caregivers - DR Sylviamalaysianhospicecouncil6240Încă nu există evaluări
- Palliative Care Intervention in The Management of Diabetes - DR Steve JonesDocument30 paginiPalliative Care Intervention in The Management of Diabetes - DR Steve Jonesmalaysianhospicecouncil6240Încă nu există evaluări
- Unspoken Needs KrisnamalDocument26 paginiUnspoken Needs Krisnamalmalaysianhospicecouncil6240Încă nu există evaluări
- Communicating With Distress Patient and Family - DR Loh Ee ChinDocument20 paginiCommunicating With Distress Patient and Family - DR Loh Ee Chinmalaysianhospicecouncil6240100% (1)
- Awareness of Cultural Diversity For Good Care - DR Loh Ee ChinDocument9 paginiAwareness of Cultural Diversity For Good Care - DR Loh Ee Chinmalaysianhospicecouncil6240Încă nu există evaluări
- Spiritual Self-Care - 1062012 - SR Geraldine TanDocument15 paginiSpiritual Self-Care - 1062012 - SR Geraldine Tanmalaysianhospicecouncil6240Încă nu există evaluări
- Care Providers Culture - DR Ibrahim AzizDocument68 paginiCare Providers Culture - DR Ibrahim Azizmalaysianhospicecouncil6240Încă nu există evaluări
- Patient Rights in EOL Care-MHC - DR Wu Huei YawDocument39 paginiPatient Rights in EOL Care-MHC - DR Wu Huei Yawmalaysianhospicecouncil6240Încă nu există evaluări
- Managing Interpersonal Conflict in EOLC - DR Ranjit Mathew OommenDocument22 paginiManaging Interpersonal Conflict in EOLC - DR Ranjit Mathew Oommenmalaysianhospicecouncil6240Încă nu există evaluări
- Nausea and Vomiting - DR Lam Chee LoongDocument13 paginiNausea and Vomiting - DR Lam Chee Loongmalaysianhospicecouncil6240Încă nu există evaluări
- Management of Dyspnoea - DR Yeat Choi LingDocument40 paginiManagement of Dyspnoea - DR Yeat Choi Lingmalaysianhospicecouncil6240Încă nu există evaluări
- Managing Incident Pain - DR Ong Eng EngDocument60 paginiManaging Incident Pain - DR Ong Eng Engmalaysianhospicecouncil6240Încă nu există evaluări
- Influenza PATHOPHYSIOLOGYDocument3 paginiInfluenza PATHOPHYSIOLOGYElle RosalesÎncă nu există evaluări
- Final Drug StudyDocument81 paginiFinal Drug StudyMinaÎncă nu există evaluări
- Fisa de Disciplina - ENG - Reumatologie - 2019 - 2020Document4 paginiFisa de Disciplina - ENG - Reumatologie - 2019 - 2020flo108Încă nu există evaluări
- Report Employee Training IPCDocument11 paginiReport Employee Training IPCDandi RawhideÎncă nu există evaluări
- An Approach To The Diagnostic Study On Annavaha Srotodusti in Urdwaga Amlapitta WSR To Oesophagogastroduodenoscopic ChangesDocument4 paginiAn Approach To The Diagnostic Study On Annavaha Srotodusti in Urdwaga Amlapitta WSR To Oesophagogastroduodenoscopic ChangesEditor IJTSRDÎncă nu există evaluări
- Value To Strategic PartnersDocument23 paginiValue To Strategic PartnersScottAndrewJordanÎncă nu există evaluări
- Emerging Re-Emerging Infectious Disease 2022Document57 paginiEmerging Re-Emerging Infectious Disease 2022marioÎncă nu există evaluări
- Safety in Sports: Made By: Shrreya Swaarnim Class: XD Roll No.: 40Document5 paginiSafety in Sports: Made By: Shrreya Swaarnim Class: XD Roll No.: 40Shrreya SwaarnimÎncă nu există evaluări
- Patient Anita NCPDocument15 paginiPatient Anita NCPJoshoua MalanaÎncă nu există evaluări
- Gastrointestinal and Abdominal Problems 3.LfDocument68 paginiGastrointestinal and Abdominal Problems 3.LfapocruÎncă nu există evaluări
- Leukemias Nursing ManagementDocument20 paginiLeukemias Nursing ManagementAnusha Verghese100% (5)
- Intranasal Steroids in PediatricsDocument39 paginiIntranasal Steroids in PediatricsKishore ChandkiÎncă nu există evaluări
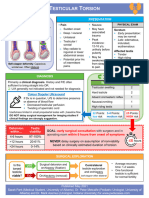
- Testicular Torsion, Peds Cases NotesDocument1 paginăTesticular Torsion, Peds Cases NotesdzalhcÎncă nu există evaluări
- Substance-Related Disorders: Ms. Jocelyn Alcera Nazario, RN MANDocument149 paginiSubstance-Related Disorders: Ms. Jocelyn Alcera Nazario, RN MAN102680Încă nu există evaluări
- NCP HeadDocument11 paginiNCP Headann-lisel-manahan-7670100% (2)
- Horner Syndrome: DescriptionDocument3 paginiHorner Syndrome: DescriptionMeike WinataÎncă nu există evaluări
- Elsharnoby Pediatric PDFDocument160 paginiElsharnoby Pediatric PDFMohammed Al-hammadiÎncă nu există evaluări
- The Effectiveness of Health Programs in Barangay Quezon, Arevalo, Iloilo CityDocument30 paginiThe Effectiveness of Health Programs in Barangay Quezon, Arevalo, Iloilo CityuhrlizÎncă nu există evaluări
- Triads in Surgery ListDocument2 paginiTriads in Surgery ListTalha AnwarÎncă nu există evaluări
- Neuroanatomical Changes After Eye Movement Desensitization and Reprocessing (EMDR) Treatment in Posttraumatic Stress DisorderDocument2 paginiNeuroanatomical Changes After Eye Movement Desensitization and Reprocessing (EMDR) Treatment in Posttraumatic Stress DisorderClaudio PeñafielÎncă nu există evaluări
- Past Quiz QuestionsDocument4 paginiPast Quiz QuestionsAbubakar AbdhooÎncă nu există evaluări
- ECMO For COVID 19 Updated 2021 Guidelines From.98326Document42 paginiECMO For COVID 19 Updated 2021 Guidelines From.98326risanataliasiburianÎncă nu există evaluări