Documente Academic
Documente Profesional
Documente Cultură
Cranio
Încărcat de
Gianna RamosDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Cranio
Încărcat de
Gianna RamosDrepturi de autor:
Formate disponibile
Craniopharyngioma is a type of brain tumor derived from pituitary gland embryonic tissue, most commonly in children but also
in men and women in their 50s and 60s.
[2]
[1]
that occurs
It arises from nests of
odontogenic (tooth-forming) epithelium within the suprasellar/diencephalic region and, therefore, contains deposits of calcium, which are evident on an x-ray. Histologically, craniopharyngiomas
resemble adamantinomas (the most common tumors of the tooth). Patients may present with bitemporal inferior quadrantanopia leading to bitemporal hemianopia, as the tumor may compress the optic chiasm. It has a point prevalence of approximately 2/100,000.
[3]
Craniopharyngiomas are also known as Rathke pouch tumors, hypophyseal duct tumors, or adamantinomas. Craniopharyngiomas are typically very slow growing tumors. They arise from the cells along the pituitary stalk. They are classified by histology as benign;
[4]
however, as with many brain tumors, their treatment
can be difficult, and significant morbidities are associated with both the tumor and treatment. Craniopharyngioma is a rare, usually suprasellar
[5]
neoplasm, which may be cystic, that develops from Rathke's pouch is an embryonic precursor of the
rests of epithelium derived fromRathke's pouch. anterior pituitary.
[6][7]
The most common presenting symptoms are headache (55-86%), endocrine dysfunction (66-90%), and visual disturbances (37-68%). Headache is slowly progressive, dull, continuous, and positional; it becomes severe in most patients when endocrine symptoms become obvious. On presentation, 40% of patients have symptoms of hypothyroidism (eg, weight gain, fatigue, cold intolerance, constipation). Almost 25% have associated signs and symptoms of adrenal failure (eg, orthostatic hypotension, hypoglycemia, hyperkalemia, cardiac arrhythmias, lethargy, confusion, anorexia, nausea and vomiting), and 20% have diabetes insipidus (eg, excessive fluid intake and urination). Most young patients present with growth failure and delayed puberty.[17
Neurologic examination
Signs suggestive of increased intracranial pressurehorizontal double vision (unilateral/bilateral) and papilledema (unilateral/bilateral)should be sought in any patient suspected of having an intracranial mass. Visual field examination may reveal various patterns of visual loss (most frequently bitemporal hemianopsia) suggestive of involvement (ie, compression) of the optic chiasma and/or tracts. Visual fields should be tested further with formal testing.
General examination
This may reveal signs relating to different endocrinopathies Hypothyroidism Symptoms of hypothyroidism include the following: Puffiness and nonpitting edema Slow return phase of deep tendon reflexes Long-standing effects on organ systems
Hypoventilation and decrease in cardiac output Pericardial and pleural effusions Constipation Anemia - Ie, normochromic normocytic Decreased mental function Psychiatric changes Adrenal insufficiency Cortisol deficiency results in hypotension, which is often orthostatic. Gastrointestinal symptoms include anorexia, nausea, and vomiting; other signs and symptoms include weight loss, hypoglycemia, lethargy, confusion, psychosis, and intolerance to stress. The signs and symptoms of aldosterone deficiency include the following:
Hypovolemia Decreased cardiac output Decreased renal blood flow with azotemia Fatigue Weight loss Cardiac arrhythmias due to hyperkalemia HYPOTHYROIDISM (basta gets?)
What is adrenal insufficiency?
Adrenal insufficiency is an endocrine-or hormonal-disorder that occurs when the adrenal glands do not produce enough of certain hormones. The adrenal glands are located just above the kidneys. Adrenal insufficiency can be primary or secondary. Primary adrenal insufficiency, also called Addison's disease, occurs when the adrenal glands are damaged and cannot produce enough of the hormone cortisol and often the hormone aldosterone. Addison's disease affects one to four of every 100,000 people, in all age groups and both sexes.
1
Secondary adrenal insufficiency occurs when the pituitary gland-a bean-sized organ in the brain-fails to produce enough adrenocorticotropin (ACTH), a hormone that stimulates the adrenal glands to produce cortisol. If ACTH output is too low, cortisol production drops. Eventually, the adrenal glands can shrink due to lack of ACTH stimulation. Secondary adrenal insufficiency is much more common than Addison's disease.
1
Munver R, Volfson IA. Adrenal insufficiency: diagnosis and management. Current Urology Reports. 2006;7:8085.
[Top]
What do adrenal hormones do?
Cortisol
Cortisol belongs to a class of hormones called glucocorticoids, which affect almost every organ and tissue in the body. Cortisol's most important job is to help the body respond to stress. Among its many vital tasks, cortisol helps maintain blood pressure and cardiovascular function slow the immune system's inflammatory response maintain levels of glucose-a form of sugar used for energy-in the blood regulate the metabolism of proteins, carbohydrates, and fats
The amount of cortisol produced by the adrenals is precisely balanced. Like many other hormones, cortisol is regulated by the brain's hypothalamus and the pituitary gland. First, the hypothalamus releases a "trigger" hormone called corticotropin-releasing hormone (CRH) that signals the pituitary gland. The pituitary responds by sending out ACTH, which in turn stimulates the adrenal glands. The adrenal glands respond by producing cortisol. Completing the cycle, cortisol then signals back to both the pituitary and hypothalamus to decrease these trigger hormones.
The hypothalamus sends CRH to the pituitary, which responds by sending out ACTH. ACTH then causes the adrenals to release cortisol into the bloodstream.
[Top]
Aldosterone
Aldosterone belongs to a class of hormones called mineralocorticoids, also produced by the adrenal glands. Aldosterone helps maintain blood pressure and water and salt balance in the body by helping the kidneys retain sodium and excrete potassium. When aldosterone production falls too low, the kidneys are not able to regulate water and salt balance, leading to a drop in both blood volume and blood pressure. [Top]
What are the symptoms of adrenal insufficiency?
The symptoms of adrenal insufficiency usually begin gradually. The most common symptoms are chronic, worsening fatigue muscle weakness loss of appetite weight loss Other symptoms can include nausea vomiting diarrhea low blood pressure that falls further when standing, causing dizziness or fainting irritability and depression
a craving for salty foods due to salt loss hypoglycemia, or low blood glucose headache sweating in women, irregular or absent menstrual periods
Hyperpigmentation, or darkening of the skin, can occur in Addison's disease but not in secondary adrenal insufficiency. This darkening is most visible on scars; skin folds; pressure points such as the elbows, knees, knuckles, and toes; lips; and mucous membranes such as the lining of the cheek. Because the symptoms progress slowly, they are often ignored until a stressful event like an illness or accident causes them to worsen. Sudden, severe worsening of symptoms is called an Addisonian crisis, or acute adrenal insufficiency. In most cases, symptoms of adrenal insufficiency become serious enough that people seek medical treatment before a crisis occurs. However, sometimes symptoms first appear during an Addisonian crisis. Symptoms of an Addisonian or "adrenal" crisis include sudden, penetrating pain in the lower back, abdomen, or legs severe vomiting and diarrhea dehydration low blood pressure loss of consciousness If not treated, an Addisonian crisis can be fatal.
What causes secondary adrenal insufficiency?
Secondary adrenal insufficiency can be traced to a lack of ACTH. Without ACTH to stimulate the adrenal glands, the adrenals' production of cortisol drops. Aldosterone production is not usually affected. A temporary form of secondary adrenal insufficiency may occur when a person who has been taking a synthetic glucocorticoid hormone such as prednisone for a long time stops taking the medication, either abruptly or gradually. Glucocorticoid hormones, which are often used to treat inflammatory illnesses such as rheumatoid arthritis, asthma, and ulcerative colitis, block the release of both CRH and ACTH. As a result, the adrenals may begin to atrophyor shrinkfrom lack of ACTH stimulation and then fail to secrete sufficient levels of cortisol. A person who stops taking a synthetic glucocorticoid hormone may have enough ACTH to function when healthy. However, when a person is under the stress of an illness, accident, or surgery, the person's body may not have enough ACTH to stimulate the adrenal glands to produce cortisol. Another cause of secondary adrenal insufficiency is surgical removal of the noncancerous, ACTHproducing tumors of the pituitary gland that cause Cushing's disease. Cushing's disease is another disorder that leads to excess cortisol in the body. In this case, the source of ACTH is suddenly removed and replacement hormone must be taken until normal ACTH and cortisol production resumes.
Less commonly, adrenal insufficiency occurs when the pituitary gland either decreases in size or stops producing ACTH. These events can result from tumors or infections of the area loss of blood flow to the pituitary radiation for the treatment of pituitary tumors surgical removal of parts of the hypothalamus surgical removal of the pituitary gland
How is adrenal insufficiency treated?
Treatment of adrenal insufficiency involves replacing, or substituting, the hormones that the adrenal glands are not making. Cortisol is replaced with a synthetic glucocorticoid such as hydrocortisone, prednisone, or dexamethasone, taken orally once to three times each day, depending on which medication is chosen. If aldosterone is also deficient, it is replaced with oral doses of a mineralocorticoid, called fludrocortisone acetate (Florinef), taken once or twice a day. Doctors usually advise patients receiving aldosterone replacement therapy to increase their salt intake. Because people with secondary adrenal insufficiency normally maintain aldosterone production, they do not require aldosterone replacement therapy. The doses of each medication are adjusted to meet the needs of the individual. During an Addisonian crisis, low blood pressure, low blood glucose, and high levels of potassium can be life threatening. Standard therapy involves intravenous injections of glucocorticoids and large volumes of intravenous saline solution with dextrose, a type of sugar. This treatment usually brings rapid improvement. When the patient can take fluids and medications by mouth, the amount of glucocorticoids is decreased until a maintenance dose is reached. If aldosterone is deficient, maintenance therapy also includes oral doses of fludrocortisone acetate. [Top]
What special problems can occur with adrenal insufficiency?
Surgery
Because cortisol is a "stress hormone," people with chronic adrenal insufficiency who need any type of surgery requiring general anesthesia must be treated with intravenous glucocorticoids and saline. Intravenous treatment begins before surgery and continues until the patient is fully awake after surgery and able to take medication by mouth. The "stress" dosage is adjusted as the patient recovers until the presurgery maintenance dose is reached. In addition, people who are not currently taking glucocorticoids but who have taken long-term glucocorticoids in the past year should tell their doctor before surgery. These people may have sufficient ACTH for normal events, but they may need intravenous treatment for the stress of surgery.
Illness
During illness, oral dosing of glucocorticoid may be adjusted to mimic the normal response of the adrenal glands to this stress on the body. Significant fever or injury may require triple oral dosing. Once recovery from the stress event is achieved, dosing is then returned to maintenance levels. People with adrenal
insufficiency should know how to increase medication during such periods of stress. Immediate medical attention is needed if severe infections, vomiting, or diarrhea occur. These conditions can precipitate an Addisonian crisis.
Points to Remember
Adrenal insufficiency is a disorder that occurs when the adrenal glands do not produce enough of certain hormones. Primary adrenal insufficiency, also called Addison's disease, occurs when the adrenal glands are damaged and cannot produce enough of the hormone cortisol and often the hormone aldosterone. Secondary adrenal insufficiency occurs when the pituitary gland fails to produce enough adrenocorticotropin (ACTH), a hormone that stimulates the adrenals to produce cortisol. If ACTH output is too low, cortisol production drops. The most common symptoms of adrenal insufficiency are chronic, worsening fatigue; muscle weakness; loss of appetite; and weight loss. Adrenal insufficiency is most often diagnosed through blood or urine tests. Imaging studies such as x rays, ultrasound, computerized tomography (CT), and magnetic resonance imaging (MRI) may also be used. Treatment of adrenal insufficiency involves replacing, or substituting, the hormones that the adrenal glands are not making. People with adrenal insufficiency should always carry identification stating their condition in case of an emergency.
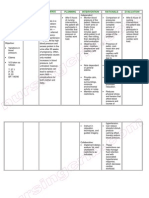
DIET: 1800/6equal feedings, 300ml feeding CBG: 8am/12nn MEDS:
7am LEVOTHYROXINE
BRAND NAME(S): Levothroid, Levoxyl, Synthroid, Unithroid USES: Levothyroxine is used to treat an underactive thyroid (hypothyroidism). It replaces or provides more thyroid hormone, which is normally produced by the thyroid gland. Low thyroid hormone levels can occur naturally or when the thyroid gland is injured by radiation/medications or removed by surgery. Having enough thyroid hormone is important for maintaining normal mental and physical activity. In children, having enough thyroid hormone is important for normal mental and physical development.This medication is also used to treat other types of thyroid disorders (such as certain types of goiters, thyroid cancer).This medication should not be used to treat infertility unless it is caused by low thyroid hormone levels.
SIDE EFFECTS: Hair loss may occur during the first few months of treatment. This effect is usually temporary as your body adjusts to this medication. If this effect persists or worsens, tell your doctor or pharmacist promptly.Remember that your doctor has prescribed this medication because he or she has judged that the benefit to you is greater than the risk of side effects. Many people using this medication do not have serious side effects.Tell your doctor immediately if any of these unlikely but serious effects of high thyroid hormone levels occur: increased sweating, sensitivity to heat, mental/mood changes (such as nervousness, mood swings), tiredness, diarrhea, shaking (tremor), headache, shortness of breath.Get medical help right away if any of these rare but serious effects of high thyroid hormone levels occur: chest pain, fast/pounding/irregular heartbeat, swelling hands/ankles/feet, seizures.A very serious allergic reaction to this drug is rare. However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.
Symptoms of low thyroid hormone levels include tiredness, muscle aches, constipation, dry skin, weight gain, slow heartbeat, or sensitivity to cold. Tell your doctor if your condition worsens or persists after several weeks of taking this medication.
8am Galvus
21
(vildagliptin)
Main use
Active ingredient
Manufacturer
Type 2 diabetes
Vildagliptin
Novartis
How does it work?
Galvus tablets contain the active ingredient vildagliptin, which is a type of medicine called a dipeptidyl peptidase-4 (DPP-4) inhibitor. It is used to treat type 2 or non-insulin dependent diabetes (NIDDM).
Vildagliptin works by increasing the amount of two incretin hormones found in the body, called glucagon-like peptide1 (GLP-1) and glucose-dependent insulinotropic peptide (GIP). These hormones are normally produced naturally by the body in response to food intake. Their function is to help control blood sugar (glucose) levels. GLP-1 and GIP have two main actions that help to control blood glucose. Firstly, they stimulate the pancreas to produce insulin in response to increasing levels of glucose in the blood. (Insulin is the main hormone responsible for controlling sugar levels in the blood. It causes cells in the body to remove sugar from the blood.) GLP-1 also reduces the production of glucagon. (Glucagon is a hormone that normally increases glucose production by the liver.) GLP-1 and GIP are normally broken down by an enzyme in the body called dipeptidyl peptidase-4 (DPP-4). Vildagliptin works by binding to this enzyme and preventing it from breaking down the GLP-1 and GIP. This increases the levels of these hormones in the body and so increases their effect on controlling blood sugar.
What is it used for?
Type 2 diabetes (non-insulin dependent diabetes). Galvus is used for people with type 2 diabetes whose blood sugar is not sufficiently controlled by other antidiabetic medicines. It can be added to treatment with metformin; a sulphonylurea, for example gliclazide; or another type of antidiabetic medicine known as a thiazolidinedione, for example pioglitazone or rosiglitazone.
Warning!
Hypoglycaemia (low blood glucose) has been commonly reported when this medicine is used in combination with metformin or sulphonylurea medicines, eg glimepiride. Symptoms of hypoglycaemia usually occur suddenly and may include cold sweats, cool pale skin, tremor, anxious feeling, unusual tiredness or weakness, confusion, difficulty in concentration, excessive hunger, temporary vision changes, headache, nausea and palpitations. You should talk to your doctor or diabetes specialist about this and make sure you know what to do if you experience these symptoms. Your ability to concentrate or react may be reduced if you have low blood sugar, and this can cause problems driving or operating machinery. You should take precautions to avoid low blood sugar when driving - discuss this with your doctor. This medicine may also cause dizziness or fatigue. If affected you should take care driving or operating machinery. People with diabetes have a higher risk of developing foot ulcers and blistering of the skin. It is therefore important to have a good foot care routine. Consult your doctor if you get any new blisters or ulcers while taking this medicine. Rare cases of inflammation of the liver (hepatitis) have been reported in people taking this medicine. For this reason, your liver function should be checked before starting treatment, every three months during the first year of treatment, and regularly thereafter. You should consult your doctor if you develop any of the following symptoms while taking this medicine, so that your liver can be checked: unexplained nausea, vomiting, abdominal pain, fatigue, loss of appetite, darkened urine or yellowing of the eyes or skin (jaundice).
Use with caution in
People with mild heart failure. People taking ACE inhibitor medicines, eg captopril.
Not to be used in
Type 1 diabetes. Diabetic ketoacidosis. Decreased liver function. Pregnancy. Breastfeeding. This medicine is not recommended for people receiving dialysis or who have moderate to severe kidney disease. This medicine is not recommended for people with severe heart failure. This medicine is not recommended for children and adolescents under 18 years of age because it has not been studied in this age group. This medicine contains lactose and should not be taken by people with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or glucose-galactose malabsorption.
This medicine should not be used if you are allergic to one or any of its ingredients. Please inform your doctor or pharmacist if you have previously experienced such an allergy. If you feel you have experienced an allergic reaction, stop using this medicine and inform your doctor or pharmacist immediately.
Pregnancy and breastfeeding
Certain medicines should not be used during pregnancy or breastfeeding. However, other medicines may be safely used in pregnancy or breastfeeding providing the benefits to the mother outweigh the risks to the unborn baby. Always inform your doctor if you are pregnant or planning a pregnancy, before using any medicine. The safety of this medicine for use during pregnancy has not been established. It should not be used during pregnancy. Diabetes mellitus is usually controlled using insulin during pregnancy, because this provides a more stable control of blood sugar. If you get pregnant while taking this medicine, or are planning a pregnancy, you should seek medical advice from your doctor. It is not known if this medicine passes into breast milk. The manufacturer states that it should not be used by breastfeeding mothers. Seek medical advice from your doctor.
Side effects
Medicines and their possible side effects can affect individual people in different ways. The following are some of the side effects that are known to be associated with this medicine. Just because a side effect is stated here does not mean that all people using this medicine will experience that or any side effect.
Common (affect between 1 in 10 and 1 in 100 people)
Tremor (when used with metformin or a sulphonylurea). Headache (when used with metformin or a sulphonylurea). Dizziness (when used with metformin or a sulphonylurea). Low blood sugar levels (when used with metformin or a sulphonylurea). Nausea (when used with metformin). Feeling weak (when used with a sulphonylurea). Weight gain (when used with a glitazone). Swelling of the legs and ankles due to excess fluid retention (when used with a glitazone).
Uncommon (affect between 1 in 100 and 1 in 1000 people)
Fatigue (when used with metformin). Constipation (when used with a sulphonylurea). Headache (when used with a glitazone). Feeling weak (when used with a glitazone).
Rare (affect between 1 in 1000 and 1 in 10,000 people)
Changes in liver function. Inflammation of the liver (hepatitis). Allergic reaction called angioedema, which may involve swelling of the face, tongue or throat, difficulty swallowing or breathing, rash or hives (stop taking this medicine and consult your doctor immediately if you experience these symptoms).
Very rare (affects less than 1 in 10,000 people)
Inflammation of the nose and throat, causing a blocked or runny nose and sore throat (nasopharyngitis). The side effects listed above may not include all of the side effects reported by the medicine's manufacturer. For more information about any other possible risks associated with this medicine, please read the information provided with the medicine or consult your doctor or pharmacist.
How can this medicine affect other medicines?
It is important to tell your doctor or pharmacist what medicines you are already taking, including those bought without a prescription and herbal medicines, before you start treatment with this medicine. Similarly, check with your doctor or pharmacist before taking any new medicines while taking this one, to ensure that thecombination is safe.
Medicines that increase blood sugar levels as a side effect may make this medicine, and other antidiabetic medicines, less effective at controlling blood sugar. Medicines that can increase blood sugar levels include the following:
, prednisone
GENERIC NAME: prednisone
BRAND NAME: Deltasone, Orasone, Prednicen-M, Liquid Pred
DRUG CLASS AND MECHANISM: Prednisone is an oral, synthetic (man-made) corticosteroid used for suppressing the immune system and inflammation. It has effects similar to other corticosteroids such as triamcinolone (Kenacort), methylprednisolone (Medrol), prednisolone(Prelone) and dexamethasone (Decadron). These synthetic corticosteroids mimic the action of cortisol (hydrocortisone), the naturally-occurring corticosteroid produced in the body by the adrenal glands. Corticosteroids have many effects on the body, but they most often are used for their potent antiinflammatory effects, particularly in those conditions in which the immune system plays an important role. Such conditions include arthritis, colitis, asthma, bronchitis, certain skin rashes, and allergic or inflammatory conditions of the nose and eyes. Prednisone is inactive in the body and, in order to be effective, first must be converted to prednisolone by enzymes in the liver. Therefore, prednisone may not work as effectively in people with liver disease whose ability to convert prednisone to prednisolone is impaired PRESCRIPTION: yes GENERIC AVAILABLE: yes PREPARATIONS: Tablets of 2.5, 5, 10, 20, and 50 mg. Oral solution or syrup of 5mg/5ml STORAGE: Store at room temperature 20-25C (68-77F), and keep away from moisture. PRESCRIBED FOR: Prednisone is used in the management of inflammatory conditions or diseases in which the immune system plays an important role. Since prednisone is used in so many conditions, only the most common or established uses are mentioned here. Prednisone most often is used for treating several types of arthritis, ulcerative colitis, Crohn's disease,systemic lupus, allergic reactions, asthma and severe psoriasis. It also is used for treating leukemias, lymphomas, idiopathic thrombocytopenic purpura and autoimmune hemolytic anemia. Corticosteroids, including prednisone, are commonly used to suppress the immune system and prevent the body from rejecting transplanted organs. Prednisone is used as replacement therapy in patients whose adrenal glands are unable to produce sufficient amounts of cortisol. DOSING: The initial dose of prednisone varies depending on the condition being treated and the age of the patient. The starting dose may be from 5 to 60 mg per day and often is adjusted based on the response of the condition being treated. Corticosteroids typically do not produce immediate effects and must be used for several days before maximal effects are seen. It may take much longer before conditions respond to treatment. Prolonged therapy with prednisone causes the adrenal glands to atrophy and stop producing cortisol. When prednisone is discontinued after a period of prolonged therapy, the dose of prednisone must be tapered (lowered gradually) to allow the adrenal glands time to recover. (See side effects.) It is recommended that prednisone be taken with food.
SIDE EFFECTS: Side effects of prednisone and other corticosteroids range from mild annoyances to serious, irreversible damage, and they occur more frequently with higher doses and more prolonged treatment. Side effects include retention of sodium (salt) and fluid, weight gain, high blood pressure, loss of potassium, headache and muscle weakness. Prednisone also causes puffiness of the face (moon face), growth of facial hair, thinning and easy bruising of the skin, impaired wound healing, glaucoma, cataracts, ulcers in the stomach and duodenum, worsening of diabetes, irregular menses, rounding of the upper back ("buffalo hump"), obesity, retardation of growth in children, convulsions, and psychiatric disturbances. The psychiatric disturbances include depression, euphoria, insomnia, mood swings, personality changes, and even psychotic behavior.
, caltrate plus
Drug Name: CALTRATE PLUS CALTRATE PLUS DESCRIPTION: CALCIUM SUPPLEMENT WITH VITAMIN D - ORAL COMMON CALTRATE PLUS BRAND NAME(S): Citracal + D, Os-Cal, Oyster Shell + D CALTRATE PLUS SIDE EFFECTS: CALTRATE PLUS is generally well tolerated. Constipation may occur. Notify your doctor if you experience nausea, vomiting, stomach cramps, dry mouth, increased thirst or increased urination while taking CALTRATE PLUS. If you notice other effects not listed above, contact your doctor or pharmacist. HOW TO USE CALTRATE PLUS: CALTRATE PLUS: Take CALTRATE PLUS orally as directed. It is best taken with or just after a meal to improve absorption. Take each dose with a full glass of water. CALTRATE PLUS USES: Calcium plays a critical role in the body. It is essential for normal functioning of nerves, cells, muscle and bone. Vitamin D improves the absorption of calcium into the body. Calcium supplements are used to treat or prevent low blood calcium levels. Calcium may be prescribed for treatment of osteoporosis (bone loss), osteomalacia (brittle bones), rickets, tetany, parathyroid disease. Calcium supplements are often used to ensure an adequate dietary intake in conditions such as pregnancy, nursing, kidney disease, pancreatitis or during therapy with anti-seizure medications. CALTRATE PLUS PRECAUTIONS: Tell your doctor if you have any pre-existing heart disease or kidney stones. CALTRATE PLUS should be used as directed during pregnancy or while breast-feeding. CALTRATE PLUS DRUG INTERACTIONS: Tell your doctor of any over-the-counter or prescription medication you may take especially digoxin and tetracycline antibiotic. Avoid taking any tetracycline antibiotic within 1 to 2 hours of taking calcium since calcium may interfere with the absorption of tetracycline. Do not start or stop any medicine without doctor or pharmacist approval. CALTRATE PLUS OVERDOSE: If overdose is suspected, contact your local poison control center or emergency room immediately. Symptoms of overdose may include nausea and vomiting, severe drowsiness, dry mouth, loss of appetite, metallic taste, stomach cramps, unconsciousness, diarrhea, weakness, headache, constipation, dizziness, or irritability.
CALTRATE PLUS NOTES: Calcium supplements are available in different forms which vary in the amount of calcium they contain. Ask your doctor or pharmacist to help select the best product for you. Follow any dietary guidelines recommended. MISSED CALTRATE PLUS DOSE: If you miss a dose, take it as soon as remembered; if it is near the time for the next dose, take both the missed dose and the regular scheduled dose then resume your usual dosing schedule. CALTRATE PLUS STORAGE: Store tablets and capsules at room temperature between 59 and 86 degrees F (15 to 30 degrees C) away from heat and light. Do not store in the bathroom.
10am: mannitol prep 12nn: domperidone NGT>> domperidone-oral
Take the Tummy Trouble Quiz Digestive Disease Myths Slideshow Pictures Heartburn? Foods to Eat, Foods to Avoid Slideshow
GENERIC NAME: DOMPERIDONE - ORAL (dom-PAIR-eh-doan)
Medication Uses | How To Use | Side Effects | Precautions | Drug Interactions | Overdose | Notes |Missed Dose | Storage USES: This medication increases movement through the digestive system. It is used to treat symptoms of stomach disorders. It may also be used to prevent nausea and vomiting caused by certain medications. Due to safety concerns, this medication is not to be used by breast-feeding women to increase production of breast milk. HOW TO USE: Take this medication by mouth as prescribed usually 30 minutes before meals and at bedtime. Do not increase your dose or take this more often than directed. Your condition will not improve any faster but the risk of side effects will be increased. SIDE EFFECTS: Headache, dizziness, dry mouth, nervousness, flushing, or irritability may occur the first several days as your body adjusts to the medication. Trouble sleeping, stomach cramps, hot flashes and leg cramps have also been reported. If any of these effects continue or become bothersome, inform your doctor. Notify your doctor immediately if you develop: chest pain, slow/fast/irregular heartbeat, swelling of the feet or ankles, difficulty urinating, swelling of the breasts or discharge from the nipple in men or women, menstrual changes, sexual difficulties. If you notice other effects not listed above, contact your doctor or pharmacist. PRECAUTIONS: Tell your doctor your medical history, especially of: history of breast cancer, allergies. Limit your intake of alcoholic beverages. This medication should be used only if clearly
needed during pregnancy. Discuss the risks and benefits with your doctor. Domperidone passes into breast milk. Due to the potential risks to a nursing infant, breast-feeding while using this drug is not recommended. Consult your doctor before breast-feeding (see also Uses section). DRUG INTERACTIONS: Because this medication enhances movement in the digestive tract, it may affect the absorption and action of other medications. Therefore, it is important to tell your doctor of any nonprescription or prescription medication you may take, especially of: MAOIs (e.g., furazolidone, phenelzine, selegiline, tranylcypromine). Do not start or stop any medicine without doctor or pharmacist approval.
, meropenem iv prep meropenem - injection, Merrem
Strep or Sore Throat Slideshow Pictures Take the MRSA Quiz!
Infectious Mononucleosis Slideshow Pictures
GENERIC NAME: MEROPENEM - INJECTION (mer-oh-PEN-um)
BRAND NAME(S): Merrem
Medication Uses | How To Use | Side Effects | Precautions | Drug Interactions | Overdose | Notes |Missed Dose | Storage USES: Meropenem is used to treat a wide variety of bacterial infections. This medication is known as a carbapenem-type antibiotic. It works by stopping the growth of bacteria. HOW TO USE: This medication is given by injection into a vein, usually every 8 hours or as directed by your doctor. The dosage is based on your medical condition and response to treatment.If you are giving this medication to yourself at home, learn all preparation and usage instructions from your health care professional. Before using, check this product visually for particles or discoloration. If either is present, do not use the liquid. Learn how to store and discard medical supplies safely.Antibiotics work best when the amount of medicine in your body is kept at a constant level. Therefore, use this drug at evenly spaced intervals.Continue to use this medication until the full prescribed treatment period is finished, even if symptoms disappear after a few days. Stopping the medication too early may allow bacteria to continue to grow, which may result in a return of the infection.Tell your doctor if your condition persists or worsens. SIDE EFFECTS: Swelling, redness, pain, or soreness at the injection site may occur. This medication may also infrequently cause upset stomach,headache, nausea, vomiting, constipation, or diarrhea. If any of these effects persist or worsen, tell your doctor or pharmacist promptly.Remember that your doctor has prescribed this medication because he or she has judged that the benefit to you is greater than the risk of side effects. Many people using this medication do
not have serious side effects.Tell your doctor right away if you have any serious side effects, including: easy bruising/bleeding, hearing changes (e.g., decreased hearing, ringing in the ears), mental/mood changes (e.g., confusion), swollen tongue.Get medical help right away if any of these rare but very serious side effects occur: seizures, unusual weakness.This medication may rarely cause a severe intestinal condition (Clostridium difficile-associated diarrhea) due to a type of resistant bacteria. This condition may occur weeks to months after treatment has stopped. Do not use anti-diarrhea products or narcotic pain medications if you have any of these symptoms because these products may make them worse. Tell your doctor immediately if you develop: persistent diarrhea, abdominal or stomach pain/cramping, blood/mucus in your stool.Use of this medication for prolonged or repeated periods may result in oral thrush or a new vaginal yeast infection. Contact your doctor if you notice white patches in your mouth, a change in vaginal discharge, or other new symptoms.A very serious allergic reaction to this drug is rare. However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.This is not a complete list of possible side effects. If you notice other effects not listed above, contact your doctor or pharmacist.In the US Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800FDA-1088.In Canada - Call your doctor for medical advice about side effects. You may report side effects to Health Canada at 1-866-234-2345.
HUMALOG
S-ar putea să vă placă și
- Upper Extremity Casting ProceduresDocument1 paginăUpper Extremity Casting ProceduresGianna RamosÎncă nu există evaluări
- CaseDocument8 paginiCaseGianna RamosÎncă nu există evaluări
- Linical Ounds Management Options For Women With Midtrimester Fetal Loss: A Case ReportDocument4 paginiLinical Ounds Management Options For Women With Midtrimester Fetal Loss: A Case ReportGianna RamosÎncă nu există evaluări
- Nursing Care Plan Pregnancy Induced Hypertension (PIH Preeclampsia and Eclampsia)Document2 paginiNursing Care Plan Pregnancy Induced Hypertension (PIH Preeclampsia and Eclampsia)deric91% (78)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (119)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- University of Wisconsin Proposal TemplateDocument5 paginiUniversity of Wisconsin Proposal TemplateLuke TilleyÎncă nu există evaluări
- 1 - Nature and Dev - Intl LawDocument20 pagini1 - Nature and Dev - Intl Lawaditya singhÎncă nu există evaluări
- Addendum Dokpil Patimban 2Document19 paginiAddendum Dokpil Patimban 2HeriYantoÎncă nu există evaluări
- De So 2 de Kiem Tra Giua Ki 2 Tieng Anh 8 Moi 1677641450Document4 paginiDe So 2 de Kiem Tra Giua Ki 2 Tieng Anh 8 Moi 1677641450phuong phamthihongÎncă nu există evaluări
- B2 WBLFFDocument10 paginiB2 WBLFFflickrboneÎncă nu există evaluări
- The Five Laws of Light - Suburban ArrowsDocument206 paginiThe Five Laws of Light - Suburban Arrowsjorge_calvo_20Încă nu există evaluări
- 5 6107116501871886934Document38 pagini5 6107116501871886934Harsha VardhanÎncă nu există evaluări
- Notes Socialism in Europe and RussianDocument11 paginiNotes Socialism in Europe and RussianAyaan ImamÎncă nu există evaluări
- Solidworks Inspection Data SheetDocument3 paginiSolidworks Inspection Data SheetTeguh Iman RamadhanÎncă nu există evaluări
- Sri Lanka Wildlife and Cultural TourDocument9 paginiSri Lanka Wildlife and Cultural TourRosa PaglioneÎncă nu există evaluări
- FM Stereo FM-AM Tuner: ST-SE500 ST-SE700Document64 paginiFM Stereo FM-AM Tuner: ST-SE500 ST-SE700al80al80100% (4)
- Unit I. Phraseology As A Science 1. Main Terms of Phraseology 1. Study The Information About The Main Terms of PhraseologyDocument8 paginiUnit I. Phraseology As A Science 1. Main Terms of Phraseology 1. Study The Information About The Main Terms of PhraseologyIuliana IgnatÎncă nu există evaluări
- Midgard - Player's Guide To The Seven Cities PDFDocument32 paginiMidgard - Player's Guide To The Seven Cities PDFColin Khoo100% (8)
- FSW School of Education Lesson Plan Template: E1aa06cb3dd19a3efbc0/x73134?path JavascriptDocument7 paginiFSW School of Education Lesson Plan Template: E1aa06cb3dd19a3efbc0/x73134?path Javascriptapi-594410643Încă nu există evaluări
- Joint School Safety Report - Final ReportDocument8 paginiJoint School Safety Report - Final ReportUSA TODAY NetworkÎncă nu există evaluări
- La TraviataDocument12 paginiLa TraviataEljona YzellariÎncă nu există evaluări
- Lost Temple of Forgotten Evil - Adventure v3 PDFDocument36 paginiLost Temple of Forgotten Evil - Adventure v3 PDFВячеслав100% (2)
- Tanroads KilimanjaroDocument10 paginiTanroads KilimanjaroElisha WankogereÎncă nu există evaluări
- Important TemperatefruitsDocument33 paginiImportant TemperatefruitsjosephinÎncă nu există evaluări
- 110 TOP Survey Interview QuestionsDocument18 pagini110 TOP Survey Interview QuestionsImmu100% (1)
- DLL - Science 6 - Q3 - W3Document6 paginiDLL - Science 6 - Q3 - W3AnatasukiÎncă nu există evaluări
- Pharmaceuticals CompanyDocument14 paginiPharmaceuticals CompanyRahul Pambhar100% (1)
- MM-18 - Bilge Separator - OPERATION MANUALDocument24 paginiMM-18 - Bilge Separator - OPERATION MANUALKyaw Swar Latt100% (2)
- Will You Be There? Song ActivitiesDocument3 paginiWill You Be There? Song ActivitieszelindaaÎncă nu există evaluări
- Microsoft Word - G10 Workbook - Docx 7Document88 paginiMicrosoft Word - G10 Workbook - Docx 7Pax TonÎncă nu există evaluări
- FCE Listening Test 1-5Document20 paginiFCE Listening Test 1-5Nguyễn Tâm Như Ý100% (2)
- PHEI Yield Curve: Daily Fair Price & Yield Indonesia Government Securities November 2, 2020Document3 paginiPHEI Yield Curve: Daily Fair Price & Yield Indonesia Government Securities November 2, 2020Nope Nope NopeÎncă nu există evaluări
- (Template) Grade 6 Science InvestigationDocument6 pagini(Template) Grade 6 Science InvestigationYounis AhmedÎncă nu există evaluări
- Mundane AstrologyDocument93 paginiMundane Astrologynikhil mehra100% (5)
- Database Interview QuestionsDocument2 paginiDatabase Interview QuestionsshivaÎncă nu există evaluări