Documente Academic
Documente Profesional
Documente Cultură
GI Operations
Încărcat de
jgcriste100%(5)100% au considerat acest document util (5 voturi)
656 vizualizări19 paginiEach year more than 500,000 Americans have gallbladder surgery. Appendectomy is performed because of probable appendicitis. The appendix is the small worm-like appendage of the colon.
Descriere originală:
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PPT, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentEach year more than 500,000 Americans have gallbladder surgery. Appendectomy is performed because of probable appendicitis. The appendix is the small worm-like appendage of the colon.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPT, PDF, TXT sau citiți online pe Scribd
100%(5)100% au considerat acest document util (5 voturi)
656 vizualizări19 paginiGI Operations
Încărcat de
jgcristeEach year more than 500,000 Americans have gallbladder surgery. Appendectomy is performed because of probable appendicitis. The appendix is the small worm-like appendage of the colon.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPT, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 19
Jeffrey Eric Criste
Removal by surgery of the appendix, the
small worm-like appendage of the colon
(the large bowel). An appendectomy is
performed because of probable appendicitis
, inflammation of the wall of the appendix
generally associated with infection.
Appendicitis usually is suspected because
of the medical history and physical
examination. The pain of developing
appendicitis is at first diffuse and poorly
localized (not confined to one spot) but, as
the inflammation extends through the
appendix to its outer covering and then to
the lining of the abdomen, the pain changes
and becomes localized to one small area
between the front of the right hip bone and
the belly button. The exact point is named
after Dr. Charles McBurney - McBurney's
point. If the appendix ruptures and infection
spreads throughout the abdomen, the pain
becomes diffuse again as the entire lining
of the abdomen becomes inflamed.
Ultrasonography and computerized
tomography also may be helpful in
diagnosis.
Due to the varying size and location of the
appendix and the proximity of other organs
to the appendix, it may be difficult to
differentiate appendicitis from other intra-
abdominal diseases.
The treatment for appendicitis is antibiotics
and surgical removal of the appendix
Is the surgical removal of the gallbladder.
Despite the development of non-surgical
techniques, it is the most common method
for treating symptomatic gallstones,
although there are other reasons for having
this surgery done. Each year more than
500,000 Americans have gallbladder
surgery. Surgery options include the
standard procedure, called laparoscopic
cholecystectomy, and an older more
invasive procedure, called open
cholecystectomy. A cholecystectomy is
performed when attempts to treat gallstones
with ultrasound to shatter the stones or
medications to dissolve them have not
proved feasible.
One common complication of
Cholecystectomy is an anomaly known as
Ducts of Luschka, occurring in 33% of the
population, is non-problematic until the gall
bladder is removed, and the tiny
supravesicular ducts may be incompletely
cauterized or remain unobserved, leading to
biliary leak post operatively. The patient will
develop biliary peritonitis within 5 to 7 days
following surgery, and will require a
temporary biliary stent. It is important that
the clinician recognize the possibility of bile
peritonitis early and confirm diagnosis via
HIDA scan to lower morbidity rate.
Aggressive pain management and antibiotic
therapy should be initiated as soon as
Large bowel resection is surgery to A bowel resection may be performed as
remove part of your large bowel. a traditional "open" procedure or as a
The large bowel connects the small minimally invasive
intestine to the anus. It is also laparoscopic procedure .
called the large intestine or colon. Indications:
Alternative Names: Large Large bowel resection is used to treat a
intestine surgery; Colon resection; variety of conditions, including:
Resection of part of large intestine;
Colectomy; Proctocolectomy Colon cancer
Description: Diverticular disease
In most cases, your bowel is A block in the intestine due to scar
cleaned before the surgery with tissue
enemas and medication. Convalescence:
The surgery is performed while you Most patients will stay in the hospital
are under general anesthesia. This for 5 to 7 days. Complete recovery from
means you are unconscious and surgery may take 2 months. During the
pain-free. A cut is made in your first few days after surgery, eating is
abdomen. The diseased part of the restricted.
large bowel is removed and the
two healthy ends of the bowel are Laparoscopic bowel resection for colon
sewn back together (resected). cancer may result in a faster recovery
The cut is closed. If the entire time than traditional open surgery.
colon and rectum is removed, it is
called a proctocolectomy.
A colostomy is an incision (cut) into the
colon (large intestine) to create an artificial
opening or "stoma" to the exterior of the
abdomen. This opening serves as a
substitute anus through which the
intestines can eliminate waste products
until the colon can heal or other corrective
surgery can be done. The bowel
movements fall into a collection pouch.
Our ostomy nursing staff will teach you
skin care and how to change the bag.
When is a colostomy needed?
A colostomy may be needed to divert intestinal contents in
conditions such as necrotizing enterocolitis ( an acute
inflammatory disease of the bowel), imperforate anus
(absence of anal opening) or Hirschsprung's Disease (a
condition in which the nerves controlling bowel function are
abnormal). Each one of these conditions will be explained in
detail by your pediatric surgeon.
How is a colostomy created?
an abdominal opening is created
the intestines are brought out through the skin
the intestine is sutured to the skin
Gastrectomy is the surgical removal of all or part of the
stomach.
Purpose
Gastrectomy is performed for several reasons, most commonly
to remove a malignant tumor or to cure a perforated or
bleeding stomach ulcer.
Description
Gastrectomy for cancer
Removal of the tumor, often with removal of surrounding
lymph nodes, is the only curative treatment for various forms
of gastric (stomach) cancer. For many patients, this entails
removing not just the tumor but part of the stomach as well.
The extent to which lymph nodes should also be removed is a
subject of some debate, but some studies show additional
survival benefit associated with removal of a greater number
of lymph nodes.
Gastrectomy, either total or subtotal (also called partial), is
the treatment of choice for gastric adenocarcinomas, primary
gastric lymphomas (originating in the stomach), and the rare
leiomyosarcomas (also called gastric sarcomas).
Adenocarcinomas are by far the most common form of
stomach cancer and are less curable than the relatively
uncommon lymphomas, for which gastrectomy offers good
After gastrectomy, the surgeon may "reconstruct" the
altered portions of the digestive tract so that it continues to
function. Several different surgical techniques are used, but,
generally speaking, the surgeon attaches any remaining
portion of the stomach to the small intestine.
Gastrectomy for gastric cancer is almost always done by the
traditional "open" surgery technique, which requires a wide
incision to open the abdomen. However, some surgeons use
a laparoscopic technique that requires only a small incision.
The laparoscope is connected to a tiny video camera that
projects a picture of the abdominal contents onto a monitor
for the surgeon's viewing. The stomach is operated on
through this incision.
The potential benefits of laparoscopic surgery include less
postoperative pain, decreased hospitalization, and earlier
return to normal activities. The use of laparoscopic
gastrectomy is limited, however. Only patients with early
stage gastric cancers or those whose surgery is only
intended for palliation-pain and symptomatic relief rather
than cure-should be considered for this minimally invasive
technique. It can only be performed by surgeons
This procedure involves dissecting the gall
bladder off of the liver, making a hole in the gall
bladder and sewing it to a hole made in the small
intestine
This allows bile to flow from the liver to gall
bladder, then directly to the intestine - this is in
essence a by-pass for bile so that it no longer
needs to flow through the common bile duct
Indications for cholecystoduodenostomy
scarred or constricted common bile duct which
does not allow bile to pass through to the
intestine
tumor of the common bile duct
pancreatitis which causes the common bile duct
to swell shut
A colectomy is surgery to remove all or part of the
colon, which is the large intestine, measuring about 5
feet (150 centimeters) long. The colon stores and
mobilizes waste until it is eliminated from the body. It
extends from the small intestine to the rectum, which
is the lower 6 inches (15 centimeters) or so of the
large intestine. A hemicolectomy (removal of about
one-half of the colon) is the primary treatment for
colorectal cancer. The amount of colon removed during
the procedure depends on how extensive the cancer
has penetrated the wall of the bowel. It also depends
on whether or not the cancer has metastasized
(spread) to the lymph nodes or other areas of the
body.
Most people have a good outcome following a colectomy.
Statistics reveal no recurrence of cancer in more than 80
percent of early-stage patients more than four years after
surgery, according to the American Academy of Family
Physicians.
The types of colectomies include:
Total colectomy. The entire colon is removed.
Right hemicolectomy. Right part of the colon is removed.
This procedure is called ileocolectomy when the lower small
intestine is removed as well.
Left hemicolectomy. Left portion of the colon is removed.
Segmental resections or partial colectomies. Smaller colon
segments are removed.
During a colectomy, the surgeon removes the part of the colon that
contains the cancer. A portion (margin) of surrounding normal
tissue is also removed to reduce the chances of stray cancer cells
remaining in the body. Nearby lymph nodes may be removed for
biopsy to determine if the cancer has spread.
The surgeon will then try to reconnect the healthy portions of the
colon or rectum. In some cases, this is not possible because of the
location of the cancer or other factors. In such situations, the
patient may need an operation known as a colostomy. This
procedure temporarily or permanently redirects body waste to an
opening created in the patient’s abdomen where it is drained from
the body into an attached bag.
Colectomy is also used to treat other medical disorders that may or
may not be related to colorectal cancer. For example, a rare,
inherited syndrome known as familial adenomatous polyposis
(FAP) sometimes requires removal of the entire colon and rectum.
This procedure is known as ileal pouch-anal anastomosis, in which
the surgeon usually constructs a pouch from the end of the small
intestine that attaches directly to the anus. Waste is then expelled
normally, although bowel movements frequently are watery.
Other conditions that may require a colectomy include:
Precancerous polyps
Diverticular disease
Intestinal blockage due to scar tissue
Chronic inflammatory bowel disease, such as ulcerative colitis or
Crohn's disease
Fecal incontinence
Traumatic injuries
A lobectomy is the removal of a lobe of one of the
organs, usually referring to the brain, the lung, or
the liver.
Purpose
Lobectomies are usually performed to prevent the
spread of cancer from part of one organ to other
parts of the organ or other parts of the body.
Lobectomies are also performed on patients with
severe seizure disorders (such as some forms of
epilepsy) to prevent further seizures. However, there
are differences in each of the three organs on which
lobectomies may be performed.
The liver has an amazing ability to repair itself. Even
if up to three-quarters of the liver is removed it will
start to re-grow very quickly, and may be back to
normal size within a few weeks.
Sometimes a lobe of the liver may be removed. This
is called lobectomy. If you have no underlying
medical problems with your liver (such as cirrhosis) it
is possible for the liver to grow back following
surgery and work normally. It is often possible to
remove fibrolamellar HCC, as this is more likely to
A splenectomy is a procedure that involves the removal of the spleen by
operative means.
The spleen, similar in structure to a large lymph node, acts as a blood filter.
Current knowledge of its purpose includes the destruction of old
red blood cells and platelets, and the detection and fight against certain
bacteria. It's also known to create new blood cells. The spleen is enlarged in
a variety of conditions such as malaria, mononucleosis and most commonly
in "cancers" of the lymphatics, such as lymphomas or leukemia.
It is removed under the following circumstances:
When it becomes very large such that it becomes destructive to platelets/red
cells
For diagnosing certain lymphomas
When platelets are destroyed in the spleen as a result of an auto-immune
process
When the spleen bleeds following physical trauma
Following spontaneous rupture
For long-term treatment of congenital erythropoietic porphyria (CEP) if
severe hemolytic anemia develops.
The classical cause of traumatic damage to the
spleen is a blow to the abdomen during a sporting
event. In cases where the spleen is enlarged due
to illness (mononucleosis), the smallest things
such as leaning over a counter or straining at
stool can cause it to rupture.
Procedure
Vaccination for pneumococcus, H. influenza and
meningococcus should be given pre-operatively if
possible. In general, spleens are removed by
laparoscopy (minimal access surgery) when the
spleen is not too large and when the procedure is
elective. It is performed by open surgery for
trauma or large spleens. Both methods are major
surgeries, and are performed under
general anesthesia. The spleen is located and
disconnected from its arteries. The ligaments
holding the spleen in place are dissected and the
spleen is removed. When indicated a drain is left
in place and the incision(s) is closed. If necessary,
tissue samples are sent to a laboratory for
A laparotomy is a large incision made into the abdomen.
Exploratory laparotomy is used to visualize and examine
the structures inside of the abdominal cavity.
Purpose
Exploratory laparotomy is a method of abdominal
exploration, a diagnostic tool that allows physicians to
examine the abdominal organs. The procedure may be
recommended for a patient who has abdominal pain of
unknown origin or who has sustained an injury to the
abdomen. Injuries may occur as a result of blunt trauma
(e.g., road traffic accident) or penetrating trauma
(e.g., stab or gunshot wound). Because of the nature of
the abdominal organs, there is a high risk of infection if
organs rupture or are perforated. In addition, bleeding
into the abdominal cavity is considered a medical
emergency. Exploratory laparotomy is used to determine
the source of pain or the extent of injury and perform
repairs if needed.
Laparotomy may be performed to determine the
cause of a patient's symptoms or to establish the
extent of a disease. For example, endometriosis is
a disorder in which cells from the inner lining of
the uterus grow elsewhere in the body, most
commonly on the pelvic and abdominal organs.
Endometrial growths, however, are difficult to
visualize using standard imaging techniques such
as x ray, ultrasound technology, or computed
tomography (CT) scanning. Exploratory
laparotomy may be used to examine the
abdominal and pelvic organs (such as the ovaries,
fallopian tubes, bladder, and rectum) for evidence
of endometriosis. Any growths found may then be
removed.
Exploratory laparotomy plays an important role in
the staging of certain cancers. Cancer staging is
used to describe how far a cancer has spread. A
laparotomy enables a surgeon to directly examine
the abdominal organs for evidence of cancer and
remove samples of tissue for further examination.
When laparotomy is used for this use, it is called
Description
The patient is usually placed under general anesthesia
for the duration of surgery. The advantages to general
anesthesia are that the patient remains unconscious
during the procedure, no pain will be experienced nor
will the patient have any memory of the procedure,
and the patient's muscles remain completely relaxed,
allowing safer surgery.
Incision
Once an adequate level of anesthesia has been
reached, the initial incision into the skin may be made.
A scalpel is first used to cut into the superficial layers
of the skin. The incision may be median (vertical down
the patient's midline), paramedian (vertical elsewhere
on the abdomen), transverse (horizontal), T-shaped, or
curved, according to the needs of the surgery. The
incision is then continued through the subcutaneous
fat, the abdominal muscles, and finally, the
peritoneum. Electrocautery is often used to cut
through the subcutaneous tissue as it has the ability to
stop bleeding as it cuts. Instruments called retractors
may be used to hold the incision open once the
abdominal cavity has been exposed.
S-ar putea să vă placă și
- Postoperative Nursing ManagementDocument7 paginiPostoperative Nursing Managementjgcriste100% (17)
- GitDocument302 paginiGitjgcriste100% (7)
- AnesthesiaDocument7 paginiAnesthesiajgcriste100% (9)
- Sutures and NeedlesDocument4 paginiSutures and Needlesjgcriste100% (4)
- Scrubbing, Gowning and GlovingDocument4 paginiScrubbing, Gowning and Glovingjgcriste85% (20)
- DrapingDocument1 paginăDrapingjgcriste92% (12)
- SterilizationDocument2 paginiSterilizationjgcriste67% (3)
- Cardiac NursingDocument26 paginiCardiac Nursingjgcriste95% (20)
- Principles of Asepsis and Sterile TechniquesDocument4 paginiPrinciples of Asepsis and Sterile Techniquesjgcriste93% (14)
- Respiratory System I. FunctionDocument6 paginiRespiratory System I. Functionjgcriste100% (3)
- Nursing Fluids and ElectrolytesDocument14 paginiNursing Fluids and Electrolytesaga1028100% (18)
- Computed Tomography (CT) and Magnetic Resonance Imaging (MRI)Document12 paginiComputed Tomography (CT) and Magnetic Resonance Imaging (MRI)jgcriste100% (9)
- Human BehaviorLec2Document25 paginiHuman BehaviorLec2jgcriste100% (4)
- Introduction To Human Behavior: By: Jeffrey Eric CristeDocument38 paginiIntroduction To Human Behavior: By: Jeffrey Eric Cristejgcriste100% (6)
- Infection and InflammationDocument14 paginiInfection and Inflammationjgcriste100% (5)
- Concepts of StressDocument9 paginiConcepts of Stressdexter100% (4)
- Health, Wellness and IllnessDocument16 paginiHealth, Wellness and Illnessjgcriste98% (44)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Management Guide Commercial Cage English Vs L0260-6Document88 paginiManagement Guide Commercial Cage English Vs L0260-6Juliana de Souza Granja BarrosÎncă nu există evaluări
- Rockaway Times 122916Document44 paginiRockaway Times 122916Peter J. MahonÎncă nu există evaluări
- Stroke - Final ReportDocument16 paginiStroke - Final ReportgolokipokÎncă nu există evaluări
- South Carolina Maternal Morbidity and Mortality Review CommitteeDocument4 paginiSouth Carolina Maternal Morbidity and Mortality Review CommitteeABC15 NewsÎncă nu există evaluări
- Pathophysiology of Atherosclerosis 1Document26 paginiPathophysiology of Atherosclerosis 1jackÎncă nu există evaluări
- Endometriosis: Endometriosis: Symptoms, Treatment, DiagnosisDocument4 paginiEndometriosis: Endometriosis: Symptoms, Treatment, DiagnosisrizkiaautikasariÎncă nu există evaluări
- AntibioticsDocument22 paginiAntibioticsEllen Castillo MarianoÎncă nu există evaluări
- Anemia BloodDocument29 paginiAnemia BloodDalia EzzeddineÎncă nu există evaluări
- Information MSQ KROK 2 Medicine 2007 2021 PEDIATRICSDocument112 paginiInformation MSQ KROK 2 Medicine 2007 2021 PEDIATRICSReshma Shaji PnsÎncă nu există evaluări
- CASE STUDY PEDIA - SaavedraDocument15 paginiCASE STUDY PEDIA - SaavedraChryst Louise SaavedraÎncă nu există evaluări
- IAPHD Hand Book On Palliative Care PDFDocument37 paginiIAPHD Hand Book On Palliative Care PDFMohammed ArshadÎncă nu există evaluări
- DESSERTATIONDocument9 paginiDESSERTATIONKinjal VasavaÎncă nu există evaluări
- Paket B Soal Listening TO US MGMP B.Inggris DKI 2023Document14 paginiPaket B Soal Listening TO US MGMP B.Inggris DKI 2023X MIPA-E /10 Garnis Trie AdistyÎncă nu există evaluări
- DewormingDocument48 paginiDewormingJulie Ann Escartin80% (5)
- Committee Opinion: Preparing For Clinical Emergencies in Obstetrics and GynecologyDocument3 paginiCommittee Opinion: Preparing For Clinical Emergencies in Obstetrics and GynecologyMochammad Rizal AttamimiÎncă nu există evaluări
- Neuromuscular BlockersDocument25 paginiNeuromuscular BlockersAbdelrahman GalalÎncă nu există evaluări
- Pasteur Eng MiddleDocument4 paginiPasteur Eng MiddleRoykoÎncă nu există evaluări
- Endocrine Physiology - Part 3 Parathyroid GlandDocument30 paginiEndocrine Physiology - Part 3 Parathyroid GlandTerrence Beniasi CharumbiraÎncă nu există evaluări
- Referentne Laboratorije Engleski Jan2021Document5 paginiReferentne Laboratorije Engleski Jan2021Laki SreckoÎncă nu există evaluări
- Australian Biology Olympiad 2009Document41 paginiAustralian Biology Olympiad 2009Science Olympiad Blog100% (1)
- ComplianceDocument13 paginiCompliancextremist2001Încă nu există evaluări
- 2016 AEIS Instructions To Candidates PDFDocument4 pagini2016 AEIS Instructions To Candidates PDFThomasÎncă nu există evaluări
- Monobind Assay Technical GuideDocument16 paginiMonobind Assay Technical GuideDaNny XaVierÎncă nu există evaluări
- Legal Med - DeathDocument42 paginiLegal Med - DeathRoy Angelo BellezaÎncă nu există evaluări
- Johnsons BabyDocument1 paginăJohnsons BabyManpreetaa50% (2)
- Cells - 1 V2 (Euks, Proks & Viruses)Document9 paginiCells - 1 V2 (Euks, Proks & Viruses)mormerodÎncă nu există evaluări
- Subacute and Chronic MeningitisDocument8 paginiSubacute and Chronic MeningitisLucky PuspitasariÎncă nu există evaluări
- Rheumatology: With Kartik Rangaraj MDDocument39 paginiRheumatology: With Kartik Rangaraj MDNailahRahmahÎncă nu există evaluări
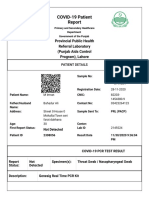
- Https Covid-19.Pshealthpunjab - Gov.pk PublicSampleResults PatientPublicSampleResultDocument2 paginiHttps Covid-19.Pshealthpunjab - Gov.pk PublicSampleResults PatientPublicSampleResultmuhammad imranÎncă nu există evaluări
- PhototherapyDocument8 paginiPhototherapyNylia AtibiÎncă nu există evaluări