Documente Academic
Documente Profesional
Documente Cultură
Puerperium Seminar
Încărcat de
Mariam Abdul Rashid100%(3)100% au considerat acest document util (3 voturi)
350 vizualizări79 paginiPuerperium Seminar
Drepturi de autor
© Attribution Non-Commercial (BY-NC)
Formate disponibile
PPT, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentPuerperium Seminar
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca PPT, PDF, TXT sau citiți online pe Scribd
100%(3)100% au considerat acest document util (3 voturi)
350 vizualizări79 paginiPuerperium Seminar
Încărcat de
Mariam Abdul RashidPuerperium Seminar
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca PPT, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 79
Puerperium
Zayed Faheem Prof. Supervised by:
Dwayyat Rana Done by:
Tasneem Awad
Asma Abdeen
Definition
The period following delivery of the baby and
placenta to about 6-8 weeks postpartum.
During that the reproductive organs and the
maternal physiology return toward the non-
pregnant status
Physiological changes during
peurperium
physiological General physiological Local
changes including: changes including:
Uterus
Cervix
Vagina
Ovaries
Perineum
Abdominal
wall
Weight
Tempreture
Breast
Bowel habit
Blood
Urine
CVS
Local Physiological Changes
1- Uterine involution as the following :-
- autolysis of excess muscle fibers - Structure
- - obliteration & thrombosis of blood vessels, then
degeneration & transformation into elastic tissue
- separation of the decidua
- gm 100 - 70 into - after delivery - gm 1000 reduced from - Weight
by the end of puerperium
cm and felt 20 after delivery the length of the uterus is - Size
at the level of umbilicus
- after one week it is midway between umbilicus and
symphysis pubis
- after 2 weeks it is at the level of symphysis
- by the end of the 6th week it is 7.5 cm long
are involuted and subinvolution - Uterine ligaments
predisposes to prolapse and retroversion
>>Most of the reduction in size occurs during the first 2 wks
The endometrial lining rapidly regenerates, so that by the 7th
day the endometrial glands will be evident. By the 16th day,
the endometrium is restored throughout the uterus, except at
the placental site .
The contractions of the arterial smooth muscle and
compression of the vessels by contraction of the myometrium
result in homeostasis. The size of the placental bed decreases
by half, and the changes in the placental bed result in the
quantity and quality of the lochia that is experienced .
j Lochia )
Postpartum, large amount of red blood initially flows from the
uterus as the contraction phase rapidly occurs, then the volume
rapidly decreases
is the bloodstained uterine discharge that is Lochia .. SO
composed of cervical mucous, vaginal transudate, and products of
necrosis and sloughing of the superficial layer of the decidua
consists mainly of blood and decidua. It lasts Lochia rubra (red): -
for 5 days .
due to relative decrease in RBCs and Lochia serosa (pale): -
predominance of leukocytes. It lasts for 5 days .
consists mainly of leukocytes and mucus. It Lochia alba (white): -
lasts for 5 days .
- Persistence of red lochia means subinvolution .
- Offensive lochia means infection .
- In severe infection with septicaemia, lochia is scanty and
not offensive
- The period of time the lochia can last varies, although it
averages approximately 5 weeks
- Often, women experience an increase in the amount of
bleeding at 7-14 days secondary to the sloughing of the
eschar on the placental site .
2- Cervical changes
The cervix begins to rapidly revert to a non-pregnant
state (less elastic, more firm) but it never returns to the
nulliparous state. By the end of the first week, the
external os is closed to the extent that a finger could not
be easily introduced.
By the end of the second week the internal os should be
closed.
3- Vaginal changes
In the first few days the streched vagina is smooth &
edematous, but by the end of the third week rugae begin
to appear, but never completely return to its pre-pregnant
size .
4- Ovaries
The resumption of normal function by the ovaries is
highly variable and is greatly influenced by breastfeeding
the infant. The woman who breastfeeds her infant has a
longer period of amenorrhea and anovulation than the
mother who chooses to bottle-feed. The mother who does
not breastfeed may ovulate as early as 27 days after
delivery. Most women have a menstrual period by 12
weeks; the mean time to first menses is 7-9 weeks.
5- Perineum
The perineum has been stretched and traumatized, and
sometimes torn or cut, during the process of labor and delivery.
The swollen and engorged vulva rapidly resolves, and swelling
and engorgement are completely gone within 1-2 weeks.
Most of the muscle tone is regained by 6 weeks, with more
improvement over the following few months. The muscle tone
may or may not return to normal, depending on the extent of
injury
6- Abdominal wall
The abdominal wall remains soft and poorly toned for many
weeks. The return to a prepregnant state depends greatly on
exercise
j About Menses
In the breastfeeding woman, the resumption of menses is
highly variable and depends on a number of factors,
including how much and how often the baby is fed and
whether the baby's food is supplemented with formula.
The delay in the return to normal ovarian function in the
lactating mother is caused by the suppression of ovulation
due to the elevation in prolactin. Half to three fourths of
women who breastfeed return to periods within 36 weeks
of delivery.
General Physiological Changes
1- Weight
Decreased due to - evacuation of uterine content.
- more fluids loss through urine and sweat
2- Temperature
A reactionary increase may occur following difficult
delivery, but it does not exceed 38C and drops within 24
hours
A slight rise may occur in the 3rd day due to breast
engorgement
3- Breast changes
The changes to the breast that prepare the mother for
breastfeeding occur throughout pregnancy
- Lactogenesis is triggered initially by the delivery of
placenta
- Falling level of Estrogen and Progesterone
- Continue presence of Prolactin
- If the mother is not lactating, the Prolactin level decreases
and return to normal within 2-3 weeks .
- Colostrum is secreted during the first 3 days
Yellowish, high protein concentration (IgA)
Protects against infection
Colostrum replaced by milk at the 3rd-4th day postpartum
- Engorgement of the breast
- Large and painful breast
But, suckling relieve the discomfort
Suckling-Prolactin- milk secretion+Oxytoxin- milk
ejection
4- Bowel changes
constipate s tendency to There -
- Causes : - Atony of the intestine
- Laxity of abdomen and perineum
- Aneroxia
- Loss of fluids
- Fear of evacuation; pain from stretched
perineum,prolapse hemorrhoid, or anal fissure
5- Blood changes
Increase coagulability of blood continue during the first 2 weeks
despite of decrease in a number of coagulation factor
This may increase incidence of PE and DVT
Hemoglobin concentration tends to fall in the first 2-3 days
6- Urine
Increase in urine production by the 2nd-4th day
Retention of urine is not uncommon
Causes: - Atony of bladder neck
- Laxity of abdomen
- Compression of urethra by vulval edema or hematoma
7- Cardiovascular changes
- Immedietely following delivery, there is marked increase
in peripheral vascular resistance due to the removal of the
low-pressure utero-placental circulatory shunt
- The cardiac output and plasma volume gradually return
to normal during the first two weeks of puerperium
- Pulse is normal but may increase if there is infection or
hemorrhage
Observation E
- Pulse, T, BP
- Breast, lochia, urine output, bowel motion
Rest and Exercise E
- Rest in bed for 2 days after uncomplicated
vaginal delivery
- Complicated/ operation needs a few days longer
- Movement in and outside the bed are advised to
minimized the risk of DVT
Management
Diet E
Food rich in proteins, vitamins, mineral and fluid
Care of the breast E
Wash the nipple and areola with warm water and soap before
and after each feed
Local Aseptic E
The vulva and perinuem are washed with antiseptic lotion
after each micturation and defecation
Then, use sterile vulval pad
Add local antibiotic if perineal stitch is present
Care of the bladder E
- Patient is encouraged to micturate frequently
- If retention present, catheter is applied under aseptic
condition
Care of the bowel E
- Uptake of vegetables are highly advisable to prevent
constipation
-Sufficient fluid intake and the use of glycerine
suppositories if needed
*Postpartum hemorrhage.
*Neurological Problems.
*Psychological problems.
*Endocrine problems.
*Miscellaneous problems.
*Puerperal Pyrexia & Sepsis.
*Infections.
*Pelvic septic thrombophlibitis.
*Thromboembolism.
Problems in the puerperium are:
Postpartum
heamorrhage
It is an excessive blood loss after delivery
First 24 h primary
Up to 6 weeks secondary
>500 mL at vaginal delivery and
>1000 mL at cesarean delivery.
Primary postpartum
hemorrhage
Causes:
-R.F: chorioaminionitis, multiple gestations,
macrosomic fetus, fibroid.
-Trt: massage and bimanual compression, then
oxytocin infusion, ergometrin, prostaglandin F2
-tIf bleeding persists despite uterine contraction
look for
cervical and vaginal lacerations.
Uterine atony
Genital tract trauma
*Secondary postpartum
hemorrhage
Causes:
Manegment:
Heavy bleedingIV infusion and X-match of blood.
Syntocinon (synthetic oxytocin).
Examination under anesthesia.
Evacuation of the uterus.
Antibiotics given if placental tissue is found,
even without evidence of overt infection
Retained products of conception
-if blood loss is not excesive, use pelvic US to
exclude retained products.
Endometritis , bleeding disorders.
Other causes:
Psychological problems
1
2
3
Postpartum Blues.
Postpartum Depression.
Postpartum Psychosis.
Postpartum Blues
Complicates50% of deliveries
mild, transient, self-limited disorder.
Mode swings, with change in appetite and
sleep.
first 2 weeks after delivery.
often resolves by postpartum
day 10.
no pharmacotherapy
is indicated.
Postpartum depression
-complicates 5% of pregnancies
-symptoms include sadness, fatigue, changes in sleeping and
eating patterns, reduced libido, crying episodes, anxiety,
and irritability.
-usually in the first few months, and may last up to several
months or even a year.
-Treatment is recommended
for 9-12 months beyond
remission of symptoms,
Postpartum psychosis
Rare but serious.
Symptoms include restless agitation,
confusion, delusions, hallucination, thoughts
of self harm.
Rarely presents before the 3d postpartum day
but usually does so before 4 weeks.
Recovery occurs over 4-6 weeks
The patient should be referred urgently to a
psychatrist and will usually reqiure admission
to a psychatric unit.
pathophysiology
Poorly undertood, but may be due to rapid
changes in estrogen, progesrtone and
prolactin in postpartum patients.
Stress
Responsibilities of child rearing
Postpartum thyroid dysfunction (psychiatric
disorders).
These psycological disorders are seen in
higher rates in patients with history of
depression or other mental illneses.
Endocrine disorders
1
3
2
Sheehans syndrome.
Postpartum Thyroiditis.
Postpartum Graves disease
Sheehans syndorme
O Anterior Pituitary gland enlarges during
pregnancy due to an increase in the size and
the number of prolactin secreting cells
O If significant hemorrhage occur during the
peripartum period ischemic necrosis of the
gland will happen.
The full picture is seen with destruction
of 95% of the gland.
Decreased prolactin
Decreased FSH & LH
causes Failed Lactation
(commonly the first symptom).
causes anovulation
& secondary amenorrhea.
1
2
Hypothyroidism
Decreased ACTH
causes bradycardia ,
cold intolerance, constipation,
causes hypotension & loss of weight.
3
4
Treatment
REPLACEMENT THERAPY
-cortisone & thyroxine for life.
-HMG for induction of ovulation IF
pregnancy is desired.
Transient destructive inflammation of Thyroid
gland occuring within the 1
st
year after
delivery.
it is believed to result from the modifications
to the immune system necessary in pregnancy
1. Thyrotoxicosis.
2. Hypothyroidism.
Postpartum Thyroiditis (PPT)
2 Phases:
The process is normally self-limiting, but
when conventional antibodies are found there
is a high chance of this proceeding to
permanent hypothyroidism.
+ Less common than PPT.
+ Similar to Graves disease in other settings.
+ Autoimmune antibodies against TSH receptors
leading to excess production of thyroid
hormones .
+ Needs treatment, like any other graves disease.
Postpartum Graves disease
Nurological problems
Nurological problems
Condition by which one or both of the lower limbs
may develop signs & symptoms of motor and/or
sensory neuropathy following delivery.
-May be due to:
1- compression or stretching of the lumbosacral plexus as it
crosses the sacroiliac joint during decent of the fetal head.
2 -Herniation of the lumbosacral discs (L4/L5) may also occur
in the exaggerated lithotomy position and during
instrumental delivery.
Obstetric Palsy
-Most cases resolve
spontaneously in a matter
of days or weeks,
or Managed orthopaedically.
Features include:
-sciatic pain.
-unilateral foot drop.
-hypoaesthesia.
-muscle wasting.
Bladder function
problems
Bladder problems
*Urinary retention, voiding difficulty, and bladder
over-distension are common.
*The baby's exit may have traumatized it leading
to temporary paralysis.
*loss of bladder sensation due to regional anesthesia.
*Swelling and pain in the perineal area.
*psychological (fear) factors
Over-distention will lead to :
1. dampen bladder sensation, render it hypo-
contractile and lead to fibrous replacement of
smooth muscle.
2. Over flow incontinence.
It's important to urinate within (6) to (8) hours of
delivery.
This decrease rate of UTI and prevent any damage
and bleeding that can happen when your bladder
gets overly full.
If the female didnt urinate during this period, we
insert a catheter.
urinary incontinence
Vaginal delivery strongly implicated in the
development of stress incontinence.
*Delivery weakened muscles around the bladder and pelvis,
which make it harder to control when urine starts.
*Hormonal changes
Bowel function disorder
It is a common problem during puerperium periods.
There are three main causes:
*Interruption of normal diet, dehydration during labor.
*Fear of evacuation due to pain from sutured perineum,
prolapsed hemorrhoid, anal fissures.
*Atony of intestinal, abdominal, perineal muscles.
constipation
management
*adequate fluid intake and increase in fiber
intake.
*stool softener (laxatives) if necessary.
Laxatives:lactulose, ispaghula
Incontinence of stool and flatus are frequent complications
of childbirth.
Anal incontinence is associated with:
**Anal sphincter damage especially operative delivery.
**following repair of third or fourth degree tear.
Stool impaction.
**Development of the anovaginal or rectovaginal fistula.
**Pelvic floor dysfunction
Anal incontinence and fecal urgency
Thromboembolism
Thromboembolism
* The risk of thromboembolic disease rises 5 fold
during pregnancy
* The majority of deaths occur in the
puerperium and are more common after
caesarean section.
* If DVT or pulmonary embolism is suspected, a full
anticoagulant therapy should be commenced &
a bilateral venogram or lung scan should be
carried out within 24 48 hours.
Puerperal pyrexia
>>puerperal pyrexia is defined as a temperature of
38C or higher on any two of the first 10 days
postpartum, exclusive of the first 24h measured
orally by a standard technique
Causes of pyrexia
*genital tract infection; upper tract (bulky tender
uterus) , or perineal infection only
*urinary tract infection.
*Breast infections e.g. mastitis.
*respiratory tract infection - this is more common
after anesthesia.
*thrombophlebitis and deep vein thrombosis.
*wound infections ; Anemia.
*non-puerperal related causes e.g. appendicitis.
Endometritis, Mastitis, UTI
most prominent Infections are among the
puerperal complications .
remains the hallmark of puerperal Fever
infection , and the patient with fever can be
until genital infection assumed to have
proven otherwise.
Endometritis
Endometritis is an infection of the endometrium
or decidua, with extension into the
myometrium and parametrial tissues .
Usually develops on the 2
nd
or 3
rd
postpartum
day .
Etiology :
.PROM > 24 hours
Cesarean section .
.Chorioamnionitis
.Excessive number of digital pelvic examination
.Prolonged labor > 12 hour
.Low socioeconomic status .
.Toxemia .
.intrauterine monitoring devices .
.pre-existing vaginitis and cervicitis
Signs & Symptoms
:
Body temp. >38c in two occasion 6h apart or once >38.5
abdominal pain Lower
: more profuse, Foul smelling or Lochia Change in
purulent
which may be difficult to interrupt Leukocytosis
because of the physiological leukocytosis seen
postpartum
Bacteriological finding
*Anaerobic streptococci .
*Gram negative coliforms
*Bacteroid spp.
*Aerobic streptococci
*Chlamydia and Mycoplasma ( difficult to
culture )
Differential Diagnosis
-Urinary tract infection.
-Acute pyelonephritis.
-Lower genital tract infection.
-Wound infection.
-Atelectasis.
-Pneumonia.
-Thrombophlebitis.
-Mastitis.
-Appendicitis
Management
.Admit to hospital.
.Evacuation of retained products of conception
under antibiotics cover.
.Parenteral broad-spectrum antibiotics, usually
stopped once the patient is afebrile for 24-48
hours, tolerating a regular diet, and
ambulating without difficulty.
Mastitis
Definition
. Inflammation of the mammary gland
Could be :
-Congestive mastitis ( breast engorgement).
-Infectious mastitis
Both are more common in Primigravidas
Infectious mastitis and breast abscess are uncommon
complications of the breastfeeding .
Almost certainly occur as a result of trauma to the
nipple and the subsequent introduction of the
Organisms from the infants nostrils .
Staph.aureus is the most common causative agent.
Infectious mastitis breast engorgment
1 wk or more after delivery.
Usually one breast is involved.
Tender, redness, swollen and hot .
Pt is febrile and appears ill .
Purulent discharge may be present .
Usually occur on the 2
nd
or 3
rd
postpartum day .
Breast are swollen, tender, tense
and warm .
Patient tempreture may be mildly
elevated.
Axillary adenopathy can be seen
treatment
>> isolation of the mother & baby
>>ceasing breast feeding from affected breast.
>>Expression of milk either manually or by electric pump.
>> microbiological culture & sensitivity of a sample of milk.
>>flucloxacillin can be commenced while awaiting
sensitivity result.
>>10% of woman with mastitis develop breast abcess which
need surgical incision & drainage under general
anesthesia.
Urinary tract infection
incidence
of women develop UTI postpartum . % 4 - 2 Approximately
During and Following delivery:
. the bladder and the lower urinary tract remains somewhat
hypotonic .
.Catheterization .
.Birth trauma .
.Conduction anesthesia
.Frequent pelvic examination
The commonest organisms are E.coli and proteus spp.
.
.Dysuria.
.Frequency of micturition.
.Loin pain if pyelonephritis occurs.
.Systemic symptoms such as pyrexia and
tachycardia.
.May be asymptomatic and recognized on routine mid-
stream urine (MSU) sample.
(This should be performed on all patients who have been
catheterized in labor)
Examination
-Raised temperature.
-Supra-pubic and/or renal angle tenderness .
Investigation
-MSU.
-White cell count.
-Nitrites and leucocytes on dipstick.
management
Broad-spectrum antibiotics until the results of
culture and sensitivity are known, then be specific
.
Bed rest .
High fluid, light solid diet .
D
S-ar putea să vă placă și
- Puerperium and Its Management 1Document35 paginiPuerperium and Its Management 1Elvis100% (2)
- New NORMAL PUERPERIUMDocument21 paginiNew NORMAL PUERPERIUMvarshaÎncă nu există evaluări
- Normal PuerperiumDocument23 paginiNormal Puerperiumnaga maniÎncă nu există evaluări
- Manual Removal of The PlacentaDocument2 paginiManual Removal of The PlacentavalpretlÎncă nu există evaluări
- Post Partum HemorhageDocument7 paginiPost Partum HemorhageLithiya JoseÎncă nu există evaluări
- Uterine Malformations PDFDocument6 paginiUterine Malformations PDFsaritha OrugantiÎncă nu există evaluări
- Polyhydramnios and OlygohydramniosDocument32 paginiPolyhydramnios and Olygohydramniosafifurrahman_rizalÎncă nu există evaluări
- Abruption PacentaDocument6 paginiAbruption PacentaKondapavuluru JyothiÎncă nu există evaluări
- Vesicular MoleDocument46 paginiVesicular Moledhisazainita0% (1)
- Normal DeliveryDocument41 paginiNormal DeliveryAliÎncă nu există evaluări
- HydramniosDocument31 paginiHydramniosSpandana DepuruÎncă nu există evaluări
- Abortion II ND Yr MSC NursingDocument121 paginiAbortion II ND Yr MSC Nursingesthereugenia100% (1)
- Management of LabourDocument16 paginiManagement of LabourAlbert MusinguziÎncă nu există evaluări
- Physiology of Normal LabourDocument29 paginiPhysiology of Normal LabournamitaÎncă nu există evaluări
- Genital Tract InjuriesDocument19 paginiGenital Tract InjuriesMarvella Nongkhar100% (1)
- Augmentation and IOLDocument22 paginiAugmentation and IOLvani reddyÎncă nu există evaluări
- Retained Placenta After Vaginal Birth and Length of The Third Stage of Labor - UpToDateDocument19 paginiRetained Placenta After Vaginal Birth and Length of The Third Stage of Labor - UpToDateHartanto Lie100% (1)
- Malpresentation and Malposition - ShoulderDocument5 paginiMalpresentation and Malposition - ShoulderNishaThakuri100% (1)
- Maternal, Morbidity, Mortality and Fertility RatesDocument18 paginiMaternal, Morbidity, Mortality and Fertility Ratesmadhu.BÎncă nu există evaluări
- Partograph DR OdofinDocument61 paginiPartograph DR OdofinEkiran BabajideÎncă nu există evaluări
- Perineal TearsDocument44 paginiPerineal TearsMagic_OverÎncă nu există evaluări
- Induction of LabourDocument18 paginiInduction of LabourNihal ZaidiÎncă nu există evaluări
- Antepartum HaemorrhageDocument18 paginiAntepartum HaemorrhageOjambo Flavia100% (1)
- Prolonged LabourDocument36 paginiProlonged LabourQuay Kar Ying100% (3)
- Malpresentation and Malposition - BreechDocument21 paginiMalpresentation and Malposition - BreechNishaThakuri100% (1)
- Minor Disorders of PregnancyDocument28 paginiMinor Disorders of PregnancyAbdullahi Suleiman Maka100% (1)
- Ectopic PregnancyDocument10 paginiEctopic PregnancyXo Yem0% (1)
- Physiological Changes During Second Stage of LabourDocument44 paginiPhysiological Changes During Second Stage of LabourTami SelviÎncă nu există evaluări
- 26a. Post Partum HemorrhageDocument35 pagini26a. Post Partum HemorrhageAubrey100% (1)
- PuerperiumDocument28 paginiPuerperiumZarlyn MirafloresÎncă nu există evaluări
- Postpartum ComplicationsDocument26 paginiPostpartum ComplicationsSharinah Ainee Sabalburo PasandalanÎncă nu există evaluări
- Abortion: TH THDocument36 paginiAbortion: TH THdimlyÎncă nu există evaluări
- AbortionsDocument99 paginiAbortionsAGERI PUSHPALATHAÎncă nu există evaluări
- CPDDocument14 paginiCPDmaezuÎncă nu există evaluări
- Puerperal SepsisDocument45 paginiPuerperal SepsisKalo kajiÎncă nu există evaluări
- Effects of Maternal Drugs On The FetusDocument9 paginiEffects of Maternal Drugs On The FetusJennifer DixonÎncă nu există evaluări
- PuerperiumDocument36 paginiPuerperiumGirish WaruÎncă nu există evaluări
- Genital Tract InjuriesDocument37 paginiGenital Tract InjuriesShady Abdelbari83% (6)
- Post Partum ComplicationDocument29 paginiPost Partum ComplicationPutri Rizky AmaliaÎncă nu există evaluări
- Seminar On Minor DisorderDocument23 paginiSeminar On Minor Disorderpriti pallabi100% (1)
- P ArtographDocument7 paginiP ArtographMali KanuÎncă nu există evaluări
- Charateristics of NewbornDocument3 paginiCharateristics of NewbornRagupathyRamanjuluÎncă nu există evaluări
- LabourDocument39 paginiLabourSravanthi Karingula100% (1)
- Multiple PregnancyDocument20 paginiMultiple PregnancyNurul Fahmiza TumiranÎncă nu există evaluări
- Prolonged Labor and Labor InductionDocument28 paginiProlonged Labor and Labor InductionNovia RizqiÎncă nu există evaluări
- Purperal InfectionsDocument69 paginiPurperal InfectionsBeulah DasariÎncă nu există evaluări
- Ectopic PregnancyDocument26 paginiEctopic PregnancysandhyakrishnanÎncă nu există evaluări
- Version FinalDocument22 paginiVersion FinalsanthiyasandyÎncă nu există evaluări
- Multiple Pregnancy: Presented byDocument49 paginiMultiple Pregnancy: Presented byvarshasharma05Încă nu există evaluări
- Multiple PregnancyDocument16 paginiMultiple Pregnancyjane7arian7berzabalÎncă nu există evaluări
- Seminar MenopauseDocument51 paginiSeminar MenopauseKelvin SuÎncă nu există evaluări
- Procedure Assignment For ManagementDocument7 paginiProcedure Assignment For ManagementPatel Amee100% (1)
- Physiology of LactationDocument3 paginiPhysiology of LactationAswathy Chandran100% (1)
- Ante Partum HemorrhageDocument30 paginiAnte Partum Hemorrhagetanmai nooluÎncă nu există evaluări
- Hyperemesis GravidarumDocument16 paginiHyperemesis GravidarumGracy Casaña100% (2)
- FEOTAL MEASURE Clinical ParametersDocument13 paginiFEOTAL MEASURE Clinical Parameterssuman guptaÎncă nu există evaluări
- Obstructed Labour (OL)Document34 paginiObstructed Labour (OL)ruhulcoc1Încă nu există evaluări
- Ob Seminar Amniotic Fluid-1Document25 paginiOb Seminar Amniotic Fluid-1Aleena Davis100% (1)
- Fetal Physiological Measurements: Proceedings of the Second International Conference on Fetal and Neonatal Physiological MeasurementsDe la EverandFetal Physiological Measurements: Proceedings of the Second International Conference on Fetal and Neonatal Physiological MeasurementsPeter RolfeÎncă nu există evaluări
- Instruction Manual in Obstetrics: Volume OneDe la EverandInstruction Manual in Obstetrics: Volume OneÎncă nu există evaluări
- 3 Use Thyroid Gland Use TTDocument55 pagini3 Use Thyroid Gland Use TTMathy MtenjeÎncă nu există evaluări
- 10 Nutrients To Improve Thyroid FunctionDocument21 pagini10 Nutrients To Improve Thyroid FunctionsiesmannÎncă nu există evaluări
- Hyperthyroidism in Pregnancy: Jorge H. MDDocument23 paginiHyperthyroidism in Pregnancy: Jorge H. MDRashid HussainÎncă nu există evaluări
- Diseases of Endocrine SystemDocument84 paginiDiseases of Endocrine SystemDuaa The PandaÎncă nu există evaluări
- Guidelines of The American Thyroid Association PREGNANCY PDFDocument47 paginiGuidelines of The American Thyroid Association PREGNANCY PDFIqra AnugerahÎncă nu există evaluări
- Obstetrics MCQ: Amanda Leow AFP NHS Lothian 20 Jan 2021Document62 paginiObstetrics MCQ: Amanda Leow AFP NHS Lothian 20 Jan 2021Amanda LeowÎncă nu există evaluări
- Hypothyroidism - Practice Essentials, Background, PathophysiologyDocument17 paginiHypothyroidism - Practice Essentials, Background, PathophysiologyprobowurÎncă nu există evaluări
- Thyroid Colloid Nodular GoiterDocument23 paginiThyroid Colloid Nodular Goitervahn025Încă nu există evaluări
- Summary of HyperthyroidismDocument8 paginiSummary of HyperthyroidismAbedinego MalukaÎncă nu există evaluări
- 1-Thyroid and Antithyroid Drugs (This)Document96 pagini1-Thyroid and Antithyroid Drugs (This)hamidÎncă nu există evaluări
- IEC Presentation PintuDocument25 paginiIEC Presentation PintuPintu MahtoÎncă nu există evaluări
- ENDOCRINE SYSTEM - REVIEWERDocument9 paginiENDOCRINE SYSTEM - REVIEWERVanya YeleniaÎncă nu există evaluări
- Down Syndrome Associated ComplicationsDocument3 paginiDown Syndrome Associated ComplicationsAlyssa Jean AlcoranÎncă nu există evaluări
- Nurul Nadia Noor Azlan - Syaza Izzati Zahari: Group 84Document52 paginiNurul Nadia Noor Azlan - Syaza Izzati Zahari: Group 84Nurul NadiaÎncă nu există evaluări
- MCQDocument21 paginiMCQNazaqat FarooqÎncă nu există evaluări
- Case StudyDocument4 paginiCase Studyllyryc100% (1)
- Thyroid DiseasesDocument5 paginiThyroid DiseasesSholehuddin MunajjidÎncă nu există evaluări
- (Endocrinology) Paolo Vitti, Laszlo Hegedus (Eds.) - Thyroid Diseases - Pathogenesis, Diagnosis and Treatment-Springer International Publishing PDFDocument478 pagini(Endocrinology) Paolo Vitti, Laszlo Hegedus (Eds.) - Thyroid Diseases - Pathogenesis, Diagnosis and Treatment-Springer International Publishing PDFOktahermoniza TanjungÎncă nu există evaluări
- Thyroid SolutionDocument58 paginiThyroid Solutionalbinuta100% (2)
- Thyroid DisordersDocument67 paginiThyroid DisordersMA 09Încă nu există evaluări
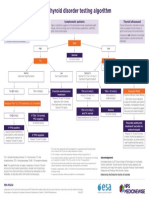
- NPS MedicineWise Thyroid Testing Algorithm v3Document1 paginăNPS MedicineWise Thyroid Testing Algorithm v3Mikhael JHÎncă nu există evaluări
- Drugs Affecting The Endocrine SystemDocument3 paginiDrugs Affecting The Endocrine SystemJerica Jaz F. VergaraÎncă nu există evaluări
- Tutorial On Goiter GadedDocument117 paginiTutorial On Goiter GadedhindabdalgadirÎncă nu există evaluări
- The Child With Endocrine DysfunctionDocument5 paginiThe Child With Endocrine Dysfunctionhenny1620Încă nu există evaluări
- 1987Document15 pagini1987hasnaÎncă nu există evaluări
- FUNDA0319Document11 paginiFUNDA0319Clarissa Guifaya50% (2)
- New Zealand Data Sheet: 1 Product NameDocument8 paginiNew Zealand Data Sheet: 1 Product NameAhmed Abd El HakimÎncă nu există evaluări
- Thyroid Function TestsDocument21 paginiThyroid Function TestsPraneeth TirumalasettyÎncă nu există evaluări
- Comlex Ii & Usmle Ii Cram Sheets - Gastroenterology Vitamins ObesityDocument31 paginiComlex Ii & Usmle Ii Cram Sheets - Gastroenterology Vitamins ObesitySolomon Seth Sallfors100% (1)