Documente Academic
Documente Profesional
Documente Cultură
Antiprotozoal Drugs: Blood and Tissue Protozoa
Încărcat de
Luciano Rodrigues SimoesDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Antiprotozoal Drugs: Blood and Tissue Protozoa
Încărcat de
Luciano Rodrigues SimoesDrepturi de autor:
Formate disponibile
Antiprotozoal Drugs
BLOOD AND TISSUE PROTOZOA
MALARIA
Etiology: Four Plasmodium species are responsible for human malaria, P. falciparum, P.ivax, P. ovale P. malariae. Epidemiology: There are about 200 million estimated global cases of malaria with a mortality of more than one million. P. falciparum (malignant tertian malaria) and P. malariae (quartan malaria) are the most common species and are found in Asia and Africa. P. vivax (benign tertian malaria) predominates in Latin America, India and Pakistan, whereas, P. ovale (ovale tertian malaria) is almost exclusively found in Africa.
The malaria parasite life cycle involves two hosts. During a blood meal, a malaria-infected female Anopheles mosquito inoculates sporozoites into the human host. After initial replication in the liver (exoerythrocytic schizogony), the parasites undergo asexual multiplication in the erythrocytes (erythrocytic schizogony). Multiplication of the blood stage parasites is responsible for the clinical manifestations of the disease. In the blood, some parasites differentiate into sexual erythrocytic stages (gametocytes). The gametocytes, after ingestion by an Anopheles mosquito during a blood meal, undergo a sporogonic cycle yielding sporozoites.?Inoculation of the sporozoites into a new human host perpetuates the malaria life cycle. Of note, in P. vivax and P. ovale, a dormant stage (hypnozoites) can persist in the liver and cause relapses by invading the bloodstream weeks, or even years later
Symptoms: The symptomatology of malaria depends on parasitemia, the presence of the organism in different organs and the parasite burden. The incubation period varies generally between 10-30 days. As the parasite load becomes significant, the patient develops headache, lassitude, vague pains in the bones and joints, chilly sensations and fever. As the disease progresses, the chills and fever become more prominent. The chill and fever follows a cyclic pattern (paroxysm) with the symptomatic period lasting 8-12 hours. In between the symptomatic period, there is a period of relative normalcy, the duration of which depends upon the species of the infecting parasite. This interval is about 34-36 hours in the case of P. vivax and P. ovale (tertian malaria), and 58-60 hours in the case of P. malariae (quartan malaria). Classical tertian paroxysm is rarely seen in P.alciparum: persistent spiking or a daily paroxysm is more usual. The malarial paroxysm is most dramatic and frightening: it begins with chilly sensation which progresses to teeth chattering overtly shaking chill, peripheral vasoconstriction resulting in cyanotic lips and nails (cold stage) which lasts for about an hour. At the end of this period the body temperature begins to climb and reaches 103-106 degrees F (39- 41degrees C). Fever is associated with severe headache, nausea (vomiting) and convulsions. The patient experiences euphoria, and profuse perspiration and the temperature begins to drop. Within a few hours the patient feels exhausted but symptomless and remains symptomatic until the next paroxysm. Each paroxysm is due to the rupture of infected erythrocytes and release of parasites
Without treatment, all species of human malaria may ultimately result in spontaneous cure except with P. falciparum which becomes more severe progressively and results in death. This organism causes sequestration of capillary vasculature in the brain, gastrointestinal and renal tissues. Chronic malaria results in splenomegaly, hepatomegaly and nephritic syndromes.
Pathology and immunology: Symptoms of malaria are due to release of massive number of merozoites into circulation. Infection results in the production of antibodies which are effective in containing the parasite load. These antibodies are against merozoites and schizonts. The infection also results in the activation of the reticuloendothelial system (phagocytes). The activated macrophages help in the destruction of infected (modified) erythrocytes and antibody coated merozoites. Cell mediated immunity also may develop and help in the elimination of infected erythrocytes. Malarial infection is associated with immunosuppression.
Diagnosis: Diagnosis is based on symptoms and detection of parasite in Giemsa stained blood smears. Treatment and Control: Treatment is effective with various quinine derivatives (quinine sulphate, chloroquine, meflaquine and primaquine, etc.). Drug resistance, particularly in P. falciparum and to some extent in P. vivax is a major problem. Control measures are eradication of infected anopheline mosquitos. Vaccines are being developed and tried but none is available ye for routine use.
DRUG CLASSIFICATION Several classes of antimalarial drugs are available
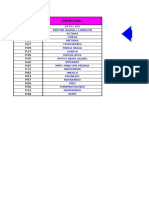
Table 53-1. Major antimalarial drugs. Drug
Chloroquine Amodiaquine1 Quinine Quinidine Mefloquine Primaquine Sulfadoxine -pyrimethamine (Fansidar) Proguanil1 Doxycycline Halofantrine Artemisinins
Class
4-Aminoquinoline 4-Aminoquinoline Quinoline methanol Quinoline methanol Quinoline methanol 8-Aminoquinoline
Use
Treatment and chemoprophylaxis of infection with sensitive parasites Treatment of infection with some chloroquine-resistant P falciparum strains Oral treatment of infections with chloroquine-resistant P falciparum Intravenous therapy of severe infections with P falciparum Chemoprophylaxis and treatment of infections with P falciparum Radical cure and terminal prophylaxis of infections with P vivax and P ovale
Folate antagonist combination
Treatment of infections with some chloroquine-resistant P falciparum
Folate antagonist
Chemoprophylaxis (with chloroquine)
Tetracycline Treatment (with quinine) of infections with P falciparum; chemoprophylaxis Phenanthrene methanol Sesquiterpene lactone endoperoxides Treatment of infections with some chloroquine-resistant P falciparum Treatment of infection with multidrug-resistant P falciparum
Atovaquone-proguanil (Malarone) Quinone-folate antagonist combination
Treatment and chemoprophylaxis of P falciparum infection
Structures of the major drugs.
CHLOROQUINE Chemistry & Pharmacokinetics Chloroquine is a synthetic 4-aminoquinoline formulated as the phosphate salt for oral use. It is rapidly and almost completely absorbed from the gastrointestinal tract, reaches maximum plasma concentrations in about 3 hours, and is rapidly distributed to the tissues. The complex pharmacokinetics of chloroquine necessitate the use of a loading dose to rapidly achieve effective serum concentrations . It has a very large apparent volume of distribution of 100-1000 L/kg and is slowly released from tissues and metabolized. Chloroquine is principally excreted in the urine with an initial half-life of 3-5 days but a much longer terminal elimination half-life of 1-2 months. Antimalarial Action & Resistance A. Antimalarial Action: Chloroquine is a highly effective blood schizonticide and remains the principal antimalarial drug in much of the world. It is also moderately effective against gametocytes of P vivax, P ovale, and P malariae but not against those of P falciparum. Chloroquine is not active against liver stage parasites. B. Mechanism of Action: The mechanism of action remains controversial. Chloroquine probably acts by concentrating in parasite food vacuoles, preventing the polymerization of the hemoglobin breakdown product, heme, into hemozoin and thus eliciting parasite toxicity due to the buildup of free heme. C. Resistance: Resistance to chloroquine is now very common among strains of P falciparum and uncommon but increasing for P vivax. Clinical Uses A. Treatment: Chloroquine is the drug of choice for the treatment of nonfalciparum and sensitive falciparum malaria. B. Chemoprophylaxis: Chloroquine is the preferred chemoprophylactic agent in malarious regions without resistant falciparum malaria. Eradication of P vivax and P ovale requires a course of primaquine to clear hepatic stages. C. Amebic Liver Abscess Adverse Effects : Pruritus is common, primarily in Africans. Nausea, vomiting, abdominal pain, headache, anorexia, malaise, blurring of vision, and urticaria are uncommon. The long-term administration of high doses of chloroquine for rheumatologic diseases can result in irreversible ototoxicity, retinopathy, myopathy, and peripheral neuropathy etc.
AMODIAQUINE Amodiaquine is closely related to chloroquine, and it probably shares mechanisms of action and resistance with that drug. Amodiaquine has been widely used to treat malaria in many countries because of its low cost, limited toxicity, and, in some areas, effectiveness against chloroquine-resistant strains of P falciparum. QUININE & QUINIDINE Introduction
Quinine and quinidine remain first-line therapies for falciparum malariaspecially severe diseasehough toxicity concerns complicate therapy. Resistance to quinine is uncommon but increasing.
Antimalarial Action & Resistance A. Antimalarial Action: Quinine is a rapidly acting, highly effective blood schizonticide against the four species of human malaria parasites. The drug is gametocidal against P vivax and P ovale but not P falciparum. It is not active against liver stage parasites. The mechanism of action of quinine is unknown. B. Resistance: Increasing in vitro resistance of parasites from a number of areas suggests that quinine resistance will be an increasing problem in the future Clinical Uses A. Parenteral Treatment of Severe Falciparum Malaria: B. Oral Treatment of Falciparum Malaria C. Malarial Chemoprophylaxis D. Babesiosis Adverse Effects : tinnitus, headache, nausea, dizziness, flushing, and visual disturbances, a constellation of symptoms termed cinchonism. Severe hypotension can follow too-rapid intravenous infusions of quinine or quinidine. Electrocardiographic abnormalities (QT prolongation) are fairly common with intravenous quinidine. Blackwater fever is a rare severe illness that includes marked hemolysis and hemoglobinuria in the setting of quinine therapy for malaria.
MEFLOQUINE Introduction Mefloquine is effective therapy for many chloroquine-resistant strains of P falciparum and against other species. Chemistry & Pharmacokinetics Mefloquine hydrochloride is a synthetic 4-quinoline methanol that is chemically related to quinine. It can only be given orally because severe local irritation occurs with parenteral use. It is well absorbed, and peak plasma concentrations are reached in about 18 hours. Mefloquine is highly protein-bound, extensively distributed in tissues, and eliminated slowly, allowing a single-dose treatment regimen. The terminal elimination half-life is about 20 days, allowing weekly dosing for chemoprophylaxis. With weekly dosing, steady state drug levels are reached over a number of weeks; this interval can be shortened to 4 days by beginning a course with three consecutive daily doses of 250 mg, though this is not standard practice. Mefloquine and acid metabolites of the drug are slowly excreted, mainly in the feces. The drug can be detected in the blood for months after the completion of therapy. Antimalarial Action & Resistance A. Antimalarial Action: Mefloquine has strong blood schizonticidal activity against P falciparum and P vivax, but it is not active against hepatic stages or gametocytes. The mechanism of action of mefloquine is unknown. B. Resistance: Sporadic resistance to mefloquine has been reported from many areas. At present, resistance appears to be uncommon except in regions of Southeast Asia with high rates of multidrug resistance (especially border areas of Thailand). Mefloquine resistance appears to be associated with resistance to quinine and halofantrine but not with resistance to chloroquine. Clinical Uses A. Chemoprophylaxis B. Treatment: Mefloquine is effective in treating most falciparum malaria, but the drug has not been approved by the FDA for this purpose. The drug is not appropriate for treating individuals with severe or complicated malaria since quinine and quinidine are more rapidly active and drug resistance is less likely with those agents.
PRIMAQUINE Introduction Primaquine is the drug of choice for the eradication of dormant liver forms of P vivax and P ovale. Antimalarial Action & Resistance A. Antimalarial Action: Primaquine is active against hepatic stages of all human malaria parasites. It is the only available agent active against the dormant hypnozoite stages of P vivax and P ovale.. Primaquine acts against erythrocytic stage parasites, but this activity is too weak to play an important role. The mechanism of antimalarial action is unknown. B. Resistance: Some strains of P vivax in New Guinea, Southeast Asia, and perhaps Central and South America are relatively resistant to primaquine. Liver forms of these strains may not be eradicated by a single standard treatment with primaquine and may require repeated therapy with increased doses (eg, 30 mg base daily for 14 days) for radical cure. Clinical Uses C. D. E. Therapy (Radical Cure) of Acute Vivax and Ovale Malaria Terminal Prophylaxis of Vivax and Ovale Malaria Chemoprophylaxis of Malaria. Gametocidal Action Pneumocystis carinii Infection.
Adverse Effects : nausea, epigastric pain, abdominal cramps, and headache, and these symptoms are more common with higher dosages and when the drug is taken on an empty stomach. More serious but rare adverse effects include leukopenia, agranulocytosis, leukocytosis, and cardiac arrhythmias. Standard doses of primaquine may cause hemolysis or methemoglobinemia (manifested by cyanosis), especially in persons with G6PD deficiency or other hereditary metabolic defects.
INHIBITORS OF FOLATE SYNTHESIS Introduction Inhibitors of enzymes involved in folate metabolism are used, generally in combination regimens, for the treatment and prevention of malaria. Chemistry & Pharmacokinetics Pyrimethamine is a 2,4-diaminopyrimidine related to trimethoprim Proguanil is a biguanide derivative Antimalarial Action & Resistance A. Antimalarial Action: Pyrimethamine and proguanil act slowly against erythrocytic forms of susceptible strains of all four human malaria species.. B. Mechanism of Action: Pyrimethamine and proguanil selectively inhibit plasmodial dihydrofolate reductase, a key enzyme in the pathway for synthesis of folate. Sulfonamides and sulfones inhibit another enzyme in the folate pathway, dihydropteroate synthase. C. Resistance: In many areas, resistance to folate antagonists and sulfonamides is common for P falciparum and less common for P vivax. Resistance is due, at least in part, to mutations in dihydrofolate reductase and dihydropteroate synthase. Because different mutations may mediate resistance to different agents, cross-resistance is not uniformly seen. Clinical Uses C. Chemoprophylaxis: Treatment of Chloroquine-Resistant Falciparum Malaria Presumptive Treatment of Falciparum Malaria Toxoplasmosis Pneumocystosis
ANTIBIOTICS Tetracycline and doxycycline are active against erythrocytic schizonts of all human malaria parasites. Clindamycin is slowly active against erythrocytic schizonts and can be used in conjunction with quinine or quinidine in those for whom doxycycline is not recommended, such as children and pregnant women. Azithromycin also has antimalarial activity and is now under study as an alternative chemoprophylactic drug. Antimalarial activity of fluoroquinolones has been demonstrated, but efficacy for the therapy or chemoprophylaxis of malaria has been suboptimal. Antibiotics also are active against other protozoans. ATOVAQUONE Atovaquone, a hydroxynaphthoquinone was initially developed as an antimalarial but has been approved by the FDA for the treatment of mild to moderate P carinii pneumonia. The drug is only administered orally. Atovaquone is an alternative therapy for P carinii infection, though its efficacy is lower than that of trimethoprimsulfamethoxazole. HALOFANTRINE Halofantrine hydrochloride, a phenanthrene-methanol related to quinine, is effective against erythrocytic stages of all four human malaria species. It is not active against hepatic stages or gametocytes. Halofantrine is rapidly effective against most chloroquine-resistant strains of P falciparum, but its use is limited by irregular absorption and cardiac toxicity. In addition, cross-resistance with mefloquine may occur. ARTEMISININ & ITS DERIVATIVES Artemisinin (qinghaosu) is a sesquiterpene lactone endoperoxide , Artemisinin and analogs are very rapidly acting blood schizonticides against all human malaria parasites. Artemisinin has no effect on hepatic stages. Artemisinin-resistant P falciparum has not yet been identified. The antimalarial activity of artemisinin probably results from the production of free radicals that follows the iron-catalyzed cleavage of the artemisinin endoperoxide bridge in the parasite food vacuole.
S-ar putea să vă placă și
- Alert Medical Series: Emergency Medicine Alert I, II, IIIDe la EverandAlert Medical Series: Emergency Medicine Alert I, II, IIIÎncă nu există evaluări
- Antiprotozoal Drugs: Blood and Tissue ProtozoaDocument12 paginiAntiprotozoal Drugs: Blood and Tissue ProtozoaStefan HutsonÎncă nu există evaluări
- Adult Infectious Disease Bulletpoints HandbookDe la EverandAdult Infectious Disease Bulletpoints HandbookEvaluare: 4.5 din 5 stele4.5/5 (9)
- Antimalarial DrugsDocument33 paginiAntimalarial DrugsPinakin Dhirajlal Jadav100% (1)
- Pha 402 AntimalarialDocument22 paginiPha 402 AntimalarialTemitopeÎncă nu există evaluări
- Pugud Samodro Bag/SMF Ilmu Penyakit Dalam FKIK Unsoed/ RSUD ProfDocument68 paginiPugud Samodro Bag/SMF Ilmu Penyakit Dalam FKIK Unsoed/ RSUD ProfpugudÎncă nu există evaluări
- Antiprotozoals Part IDocument46 paginiAntiprotozoals Part IAYO NELSONÎncă nu există evaluări
- Clinical Aspect of MalariaDocument68 paginiClinical Aspect of MalariaselviaÎncă nu există evaluări
- Antiprotozoal Drugs NotesDocument22 paginiAntiprotozoal Drugs NotesMae Lislie Canonigo - FloresÎncă nu există evaluări
- Malaria: Michelle Carandang-Cuvin, M.D. FPPS, Fpidsp Pediatric Infectious Disease ConsultantDocument77 paginiMalaria: Michelle Carandang-Cuvin, M.D. FPPS, Fpidsp Pediatric Infectious Disease ConsultantHanako AranillaÎncă nu există evaluări
- Epidemiology & Control of Tropical DiseaseDocument38 paginiEpidemiology & Control of Tropical DiseaseMazinÎncă nu există evaluări
- Malaria MettyDocument13 paginiMalaria MettySiti Qomariah AnisaÎncă nu există evaluări
- GROUP A1 (A) Topic 5Document37 paginiGROUP A1 (A) Topic 5KhaiÎncă nu există evaluări
- Antimalarial DrugsDocument45 paginiAntimalarial DrugsDeribe BekeleÎncă nu există evaluări
- Lapkas Malaria FixDocument35 paginiLapkas Malaria FixWinson ChitraÎncă nu există evaluări
- Anti-Malarial DrugsDocument58 paginiAnti-Malarial Drugs88AKKÎncă nu există evaluări
- Malaria: Michael Aguilar, RMTDocument27 paginiMalaria: Michael Aguilar, RMTFrankenstein MelancholyÎncă nu există evaluări
- MalariDocument36 paginiMalariUmashankar SharmaÎncă nu există evaluări
- Typhi EpiDocument13 paginiTyphi EpiMaria PavlovaÎncă nu există evaluări
- Malaria: Dr. Dwi HandayaniDocument53 paginiMalaria: Dr. Dwi Handayanidebieyolanda_7180456Încă nu există evaluări
- Malaria Is A Parasitic Disease That Involves High Fevers, Shaking Chills, Flu-Like Symptoms, and AnemiaDocument6 paginiMalaria Is A Parasitic Disease That Involves High Fevers, Shaking Chills, Flu-Like Symptoms, and AnemiaMarrylane GamisÎncă nu există evaluări
- Artesunate For The Treatment of Severe Falciparum Malaria: Philip J. Rosenthal, M.DDocument7 paginiArtesunate For The Treatment of Severe Falciparum Malaria: Philip J. Rosenthal, M.DbadshahytÎncă nu există evaluări
- 1.anti MalariaDocument118 pagini1.anti MalariaRaka PradewaÎncă nu există evaluări
- Disease Caused by ProtozoansDocument21 paginiDisease Caused by ProtozoansBrijesh KumarÎncă nu există evaluări
- Malariappt 110313053826 Phpapp01Document12 paginiMalariappt 110313053826 Phpapp01spiderind2Încă nu există evaluări
- 微生物與疾病Document22 pagini微生物與疾病super longhairÎncă nu există evaluări
- Malaria, P.Vivax and P.Falciparum AntigenDocument1 paginăMalaria, P.Vivax and P.Falciparum AntigenRohanJainÎncă nu există evaluări
- MalariaDocument12 paginiMalariasaxebe7427Încă nu există evaluări
- Rome TineDocument2 paginiRome TineKristine Monforte Coma UritaÎncă nu există evaluări
- Farmakologi 4 (Antimalaria)Document7 paginiFarmakologi 4 (Antimalaria)Gifanichan MvpshawolandromedaÎncă nu există evaluări
- Malaria: DR Sulaiman Conteh Medical StudentsDocument36 paginiMalaria: DR Sulaiman Conteh Medical StudentsAbubakar JallohÎncă nu există evaluări
- Antiprotozoa 14Document60 paginiAntiprotozoa 14adilaÎncă nu există evaluări
- Antimalarial Drug CologyDocument15 paginiAntimalarial Drug CologyManthan ChauhanÎncă nu există evaluări
- Epidemiology Prevention & Control of Malaria: Dr. Neha Tyagi Assistant Professor Department of Community MedicineDocument29 paginiEpidemiology Prevention & Control of Malaria: Dr. Neha Tyagi Assistant Professor Department of Community MedicineShashi TyagiÎncă nu există evaluări
- Malaria LectureDocument32 paginiMalaria LectureNwosu Ogbonna GabrielÎncă nu există evaluări
- What Is MalariaDocument9 paginiWhat Is MalariaJoras Joy Yu Gregorio-AntojadoÎncă nu există evaluări
- Current Trends in The Management of MalariaDocument41 paginiCurrent Trends in The Management of Malariaghr9cjy5npÎncă nu există evaluări
- Examination Card 10Document9 paginiExamination Card 10FUTURE DOCTORÎncă nu există evaluări
- Malaria Cycle and Antimalarials PDFDocument22 paginiMalaria Cycle and Antimalarials PDFPreeti YadavÎncă nu există evaluări
- Antiparasitic Drugs (Antiprotozoal: DR John EgbagbaDocument37 paginiAntiparasitic Drugs (Antiprotozoal: DR John EgbagbaPrincewill SeiyefaÎncă nu există evaluări
- MalariaDocument32 paginiMalariaNajwa Amalia75% (4)
- PlasmodiumDocument99 paginiPlasmodiumCharlene SuliganÎncă nu există evaluări
- Anti MalariaDocument8 paginiAnti MalariaAini Nur Syafa'ahÎncă nu există evaluări
- Malaria Is An Acute and Chronic Parasitic Disease: Etiologic AgentDocument6 paginiMalaria Is An Acute and Chronic Parasitic Disease: Etiologic AgentStephanie Rae BaccayÎncă nu există evaluări
- MalariaDocument41 paginiMalariaMohiuddin AhmedÎncă nu există evaluări
- Antimalarial Drug Mefloquine Is A Possible CureDocument8 paginiAntimalarial Drug Mefloquine Is A Possible Curehuma javeriaÎncă nu există evaluări
- Malaria Is A Mosquito-Borne Infectious Disease Caused by A Eukaryotic Protist of The GenusDocument5 paginiMalaria Is A Mosquito-Borne Infectious Disease Caused by A Eukaryotic Protist of The GenusMichael PadamaÎncă nu există evaluări
- What Is MalariaDocument6 paginiWhat Is MalariaAnubhav SharmaÎncă nu există evaluări
- Malaria: Dr. Shree Narayan Yadav Internal Medicine Resident NamsDocument40 paginiMalaria: Dr. Shree Narayan Yadav Internal Medicine Resident Namsasyanadhikary18Încă nu există evaluări
- SEI - INEP - 0137469 - Projeto BásicoDocument29 paginiSEI - INEP - 0137469 - Projeto BásicoMARLOMbran HERRÎncă nu există evaluări
- Frank's Malaria in PregDocument54 paginiFrank's Malaria in PregifiokikpeÎncă nu există evaluări
- 'Mbbs Lecture Note Malaria - pptx2021-1Document56 pagini'Mbbs Lecture Note Malaria - pptx2021-1Noah OlumideÎncă nu există evaluări
- Medicine Lec.12 - Protozoal InfectionDocument60 paginiMedicine Lec.12 - Protozoal Infection7fefdfbea1Încă nu există evaluări
- Malaria Trans EditedDocument4 paginiMalaria Trans EditedSven OrdanzaÎncă nu există evaluări
- MalariaDocument5 paginiMalariasubhashreepal700Încă nu există evaluări
- Malaria Drugs 210Document66 paginiMalaria Drugs 210fombayÎncă nu există evaluări
- Malaria Treatment Guidelines WHO 2010Document211 paginiMalaria Treatment Guidelines WHO 2010emc27Încă nu există evaluări
- Unit 2 (C) Anti-Malarials, Educational PlatformDocument50 paginiUnit 2 (C) Anti-Malarials, Educational PlatformIzazÎncă nu există evaluări
- Farmakologi AntiparasitDocument119 paginiFarmakologi AntiparasitFitri Sri WulandariÎncă nu există evaluări
- Malaria: Symptoms When Symptoms AppearDocument6 paginiMalaria: Symptoms When Symptoms AppearrbacaracÎncă nu există evaluări
- RRC in Critical Care Lisa GemmellDocument6 paginiRRC in Critical Care Lisa GemmellFaldo Anshari IrzaÎncă nu există evaluări
- Microbiology - Exercise 3e AntibiogramDocument5 paginiMicrobiology - Exercise 3e Antibiogramapi-253346521Încă nu există evaluări
- ISHRS - GNaughton - HSC Clinical UpdateDocument26 paginiISHRS - GNaughton - HSC Clinical UpdateErin AguilarÎncă nu există evaluări
- Astrazeneca in China CaseDocument5 paginiAstrazeneca in China CaseSunil ChoudhuryÎncă nu există evaluări
- Pharmacuetics For The Students of Pharmacy Technicians (Category-B)Document45 paginiPharmacuetics For The Students of Pharmacy Technicians (Category-B)Naina's kitchencookingvediosÎncă nu există evaluări
- Analysis of Hypochlorite in Bleach: Experiment 8Document8 paginiAnalysis of Hypochlorite in Bleach: Experiment 8Nabilah HarisÎncă nu există evaluări
- Article On BA&BEDocument7 paginiArticle On BA&BENitin DhimanÎncă nu există evaluări
- Oxytocic & TocolyticDocument12 paginiOxytocic & TocolyticFahmi Dwika Hafiz TrionoÎncă nu există evaluări
- Bio AssayDocument20 paginiBio AssayNeha Tiwari100% (2)
- Alcohol in The Western WorldDocument6 paginiAlcohol in The Western WorldaubeyitÎncă nu există evaluări
- Advice and Information: ManagementDocument4 paginiAdvice and Information: ManagementAlvin Germo PasuquinÎncă nu există evaluări
- Progenitors (Convention: Mage The Ascension)Document7 paginiProgenitors (Convention: Mage The Ascension)Beth100% (2)
- Pharmacy Management SystemDocument4 paginiPharmacy Management SystemTaniya FernandoÎncă nu există evaluări
- Chapter 9 Import Operations and ActionsDocument96 paginiChapter 9 Import Operations and ActionsrogerÎncă nu există evaluări
- Antifungal Activity of Leaf Ethanolic Extract From Carmona Retusa (Tsaang Gubat) Against Candida AlbicansDocument36 paginiAntifungal Activity of Leaf Ethanolic Extract From Carmona Retusa (Tsaang Gubat) Against Candida AlbicansELIANA CARIS CABILDOÎncă nu există evaluări
- Drug StudyDocument13 paginiDrug StudyJaessa Feliciano50% (2)
- Futureof GCCPharmaceutical Industry 1Document4 paginiFutureof GCCPharmaceutical Industry 1shyamchepurÎncă nu există evaluări
- BRH Drug StudyDocument6 paginiBRH Drug StudyStephanie Dellera AgdanÎncă nu există evaluări
- Oral Lipid-Based Formulations: David J. HaussDocument10 paginiOral Lipid-Based Formulations: David J. HaussAna KovačevićÎncă nu există evaluări
- Industrial Process For Preparation of Levetiracetam.Document9 paginiIndustrial Process For Preparation of Levetiracetam.Drkrishnasarma pathy100% (4)
- 02A12002 PRC EditsDocument114 pagini02A12002 PRC EditsAndre BoscattoÎncă nu există evaluări
- Pharmacological Science Adverse Effects Pharmaceutical Products Etymological Adverse Drug Reactions Prophylaxis Medication ErrorsDocument27 paginiPharmacological Science Adverse Effects Pharmaceutical Products Etymological Adverse Drug Reactions Prophylaxis Medication ErrorsSuchita HenrageÎncă nu există evaluări
- List Produk PT - MBS (September)Document94 paginiList Produk PT - MBS (September)clara shinta dilapanga50% (2)
- IT Head DataDocument2 paginiIT Head DataTejas SuryawanshiÎncă nu există evaluări
- Dda Guideline NepalDocument3 paginiDda Guideline NepalImdadHussainOPositiveÎncă nu există evaluări
- Abbreviations Latin Meaning English Meaning Aa, Āā, ĀĀ AAA A.C. A.c.h.s., Ac&hs A.D. Ad., AddDocument18 paginiAbbreviations Latin Meaning English Meaning Aa, Āā, ĀĀ AAA A.C. A.c.h.s., Ac&hs A.D. Ad., AddKathleen GasparinÎncă nu există evaluări
- Laporan Stoc ObatDocument34 paginiLaporan Stoc ObatAyouItuYustirahayuÎncă nu există evaluări
- Job DescriptionDocument2 paginiJob DescriptionswethashakiÎncă nu există evaluări
- Drugs in Emergencies: DR U I HapuarachchiDocument31 paginiDrugs in Emergencies: DR U I HapuarachchiMaduka SanjeewaÎncă nu există evaluări
- Cost and Management Accounting in Practise: An Industry Specific PerspectiveDocument16 paginiCost and Management Accounting in Practise: An Industry Specific PerspectivediveshÎncă nu există evaluări