Documente Academic
Documente Profesional
Documente Cultură
Postpartal Pueperal Infection
Încărcat de
Irish Jane Bayle CubilloDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Postpartal Pueperal Infection
Încărcat de
Irish Jane Bayle CubilloDrepturi de autor:
Formate disponibile
Irish Jane B.
Cubillo
III BSN-1
The postpartum period is a time of increased
physiologic stress and major psychological
transition. Energy depletion and fatigue of late
pregnancy and labor, soft-tissue trauma from
delivery, and blood loss increase the womans
vulnerability to complications.
The potential seriousness of many postpartum
complications; associated pain, procedures and
medications; frequent need to be isolated or
separated from the newborn; emotionally
disruptive effects of the physiologic
malfunction can interfere with the maternal-
newborn bonding process.
Postpartum Puerperal Infection
Postpartum infections of the genital tract
associated with childbirth; usually are the result
of bacteria ascending from the genital tract.
Often remain localized, but they extend along
vascular or lymphatic pathways to produce
extensive pelvic and systemic infections.
One of the most common causes of morbidity in the
postpartum period.
The course of the illness varies according to:
the size of the bacterial inoculum
virulence of the organism
the pelvic tissues affected
the hosts defense mechanisms including general
health and immunologic status
Fever: principal sign
Etiology
Idiopathic
Risk factors:
Related to general infection risk
Related to labor events
Related to operative risk factors
Related to general infection risk
- Anemia
- Nutritional deficiencies
- Lack of prenatal care
- Obesity
- Low socioeconomic status
- Sexual intercourse after rupture of membranes
- Immunosuppression
Related to labor events
- Prolonged labor
- Prolonged rupture of membranes
- Chorioamionitis
- Greater number of vaginal examinations
- Hemorrhage
Related to operative risk factors
- Cesarean delivery
- General anesthesia
- Urgency of operation
- Breaks in operative techniques
- Manual placental removal
- Forceps delivery
- Episiotomy
- Lacerations
Causative agents:
Anaerobic (not requiring oxygen for growth): gram
negative bacilli- Bacteroides species
Aerobic (requiring oxygen for growth): most
common; gram positive cocci- Streptococcus species
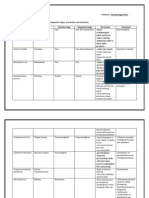
Nursing Assessment
Focuses on early identification of signs and
symptoms;
Monitor progress and physiologic function
including uterine involution
Note needs for comfort and education
Identify emotional reactions and needs
Vital Signs
Assess:
Condition of the perineum and uterus
Character of lochia
Condition of extremities and breasts
Status of bladder
Bowel function
Nursing Intervention
Prompt diagnosis and treatment of the
postpartum infection to minimize serious
sequelae and reduce their effects on the clients
ability to function are essential.
Antibiotic Therapy
Specimen collection
Wound debridement or cleansing
Analgesic administration and monitoring
Comfort measures for pain relief
Health teaching about the infectious process
Prevention of Infection
Avoid possible sources of infection
Careful hand washing
Standard precautions
Endometritis
A localized infection of the inner uterine wall
Begins at the placental site and may spread to
involve the entire endometrium
Bacteria gain access to the uterus through the
vagina and enter the uterus either at the time of
birth or during the post partal period
Following vaginal delivery, about 2%-3%
develop endometritis
may occur with any birth, but the infection is
usually associated with chorioamnionitis and
cesarean birth
Clinical Manifestations
benign temperature elevation (first post partal
day)
increase in white blood cells
increase in oral temperature to more than 38 C
for two consecutive 24-hour periods
Chills
loss of appetite
Clinical Manifestations
general malaise
uterus not well contracted and painful to touch
lochia is dark brown and has foul odor
if the infection is accompanied by high fever, lochia
may be scant or absent
if the infection is caused by hemolytic
Streptococcus, the lochia usually is odorless
Diagnostic Procedures
Ultrasound: to confirm the
presence of placental fragments
that are a possible cause of the
infection
Lochia culture
Hysterosalpingogram
Nursing Management
Emotional support
Fowlers position or walking: promote
lochial drainage
Hand washing technique
Monitor:
progress of uterine involution
fundal height and firmness
tenderness
characteristics of lochia
Increased fluid intake(3L-4L/day)
Well-balanced diet
Advise mother to avoid breast-
feeding if necessary
Treatment
Antibiotics:
Clindamycin (Cleocin)
Metronidazole
Gentamicin
Aztreonam
Aminoglycoside
Wound Infection
Also known as infection of the
perineum
If a woman has a suture line on her
perineum from an episiotomy or a
laceration repair, a portal of entry
exists for bacterial invasion.
Usually remains localized
Clinical Manifestations
Pain
Heat
Feeling of pressure
May or may not have elevated temperature
Inflammation on the suture line
Suture line may be open with
presence of purulent discharge
Diagnostic Procedures
Culture of the discharge using a sterile cotton-
tipped applicator
Nursing Intervention
Nurse-midwife may remove the perineal suture to
allow drainage
Packing, such as iodoform gauze may be placed in
the open lesion
Systemic or topical antibiotics
Analgesics to alleviate discomfort
Sitz bath
Moist warm compress
Hubbard tank treatment
Remind patient to change perineal pad
frequently
Wipe front to back after bowel movement
Urinary Tract
Infection
A woman who is catheterized at
the time of childbirth or during
the postpartal period is prone to
development of a urinary tract
infection, because bacteria may be
introduced into the bladder at the
time of catheterization
Physiologic urinary stasis, dilatation of the
ureters and vesicoureteral reflux that occur
during pregnancy persist for several months after
delivery
Occurs 5% of postpartum client and are usually
caused by coliform bacteria (E. coli, enterococci,
Klebsiella pneumonia)
Postpartum urinary retention and incomplete
emptying of the bladder are common because of
increased bladder capacity, decreased tone and
decreased perception of the urge to void caused
by perineal trauma.
If client is unable to empty the bladder fully, the
remaining urine is a culture medium for the
bacterial growth, often leading to cystitis
(inflammation of the bladder) or
pyelonephritis (inflammation of the renal
pelvis).
Risk factors
Cesarean birth
Use of forceps or vacuum extraction
Epidural anesthesia
And catheterization during labor
Clinical Manifestations
Burning on urination
Blood in the urine (hematuria)
Feeling of frequency in urinating
Sharp pain on urinating
Low grade fever
Lower abdominal pain
Diagnostic Procedures
Physical examination
Urinalysis: Obtain a clean-catch urine specimen;
examine the following:
Leukocytosis
Red blood cells
Bacteria
Nursing Interventions
Encourage a woman:
to drink large amounts of fluid
to perform proper perineal care
to use of cotton underclothing
to void frequently
to void before and after the
intercourse
Broad -spectrum antibiotic
Amoxicillin
Ampicillin
Oral analgesic: to reduce
the pain of urination
Acetaminophen (Tylenol)
References
Maternal and Child Nursing by Adele Pillitteri
6
th
Ed. (pg. 682~690)
Maternity Nursing family, Newborn and
Womens Health Care 8
th
Ed. (pg.1028~1041)
THANK YOU!
S-ar putea să vă placă și
- Elizabeth G. Querubin BSN 3E1-9 - Group 195 A Ectopic PregnancyDocument16 paginiElizabeth G. Querubin BSN 3E1-9 - Group 195 A Ectopic PregnancyLizeth Querubin97% (38)
- Bleeding During PregnancyDocument69 paginiBleeding During PregnancyMohnnad Hmood AlgaraybhÎncă nu există evaluări
- Dementia: College of NursingDocument47 paginiDementia: College of NursingIrish Jane Bayle CubilloÎncă nu există evaluări
- The Secret of LaughterDocument5 paginiThe Secret of LaughterlastrindsÎncă nu există evaluări
- Abnormal PuerperiumDocument21 paginiAbnormal PuerperiumNatukunda DianahÎncă nu există evaluări
- Female Uterine Disorders (Sy 2008-09)Document150 paginiFemale Uterine Disorders (Sy 2008-09)Jasmine Faye D. MadrigalÎncă nu există evaluări
- Rinary Ract Nfections: Classification Pathophysiology Risk Factors Clinical Manifestation DiagnosticsDocument27 paginiRinary Ract Nfections: Classification Pathophysiology Risk Factors Clinical Manifestation DiagnosticsDARYmagpantayÎncă nu există evaluări
- ENDOMETRITISDocument6 paginiENDOMETRITISKhrisna ParamaarthaÎncă nu există evaluări
- High Risk PregnancyDocument10 paginiHigh Risk PregnancyRoy Mujeres CabueñasÎncă nu există evaluări
- Presentation On: Pueperal Sepsis: Submitted To: Sandhya Maam Submitted By: Dhana BC Kismita Rai BSC 3 YearDocument31 paginiPresentation On: Pueperal Sepsis: Submitted To: Sandhya Maam Submitted By: Dhana BC Kismita Rai BSC 3 YearRumi Maharjan100% (1)
- Unit X - Abnormalities During Postnatal Period Assessment and Management of Women With Postnatal Complications Total: 4 HoursDocument73 paginiUnit X - Abnormalities During Postnatal Period Assessment and Management of Women With Postnatal Complications Total: 4 Hourssoumya satheshÎncă nu există evaluări
- Barangay Peace and Order and Public Safety PlanDocument3 paginiBarangay Peace and Order and Public Safety PlanPeter Fritz Boholst100% (1)
- UConn Prosthodontics Clinic Manual 12-13Document69 paginiUConn Prosthodontics Clinic Manual 12-13lippincott2011Încă nu există evaluări
- Postpartum Complications: Donald G. Camatura, RNDocument96 paginiPostpartum Complications: Donald G. Camatura, RNDonald Garcesa Camatura100% (4)
- Urinary Tract Infection FinalllllllllDocument55 paginiUrinary Tract Infection FinalllllllllBinita ShakyaÎncă nu există evaluări
- GlargineDocument22 paginiGlargineAgus SuwiryawanÎncă nu există evaluări
- Red Hill ComplaintDocument109 paginiRed Hill ComplaintHonolulu Star-AdvertiserÎncă nu există evaluări
- Puerperal SepsisDocument34 paginiPuerperal SepsisSanthosh.S.UÎncă nu există evaluări
- Mmda V Concerned Citizens of Manila Bay (GR No 171947) DigestDocument2 paginiMmda V Concerned Citizens of Manila Bay (GR No 171947) DigestJose Ramon Ampil83% (6)
- Nursing TheoriesDocument50 paginiNursing TheoriesIrish Jane Bayle Cubillo80% (5)
- Pelvic Inflammatory DiseaseDocument20 paginiPelvic Inflammatory DiseaseDeniela Jamaicy Herbert100% (1)
- Purperal InfectionsDocument69 paginiPurperal InfectionsBeulah DasariÎncă nu există evaluări
- SGC Resolution TemplateDocument3 paginiSGC Resolution Templatehendrix100% (3)
- Postpartal Pueperal Infection: Irish Jane B. Cubillo Iii Bsn-1Document10 paginiPostpartal Pueperal Infection: Irish Jane B. Cubillo Iii Bsn-1Irish Jane Bayle CubilloÎncă nu există evaluări
- Infections After DeliveryDocument33 paginiInfections After DeliveryErica P. ManlunasÎncă nu există evaluări
- Pelvic Inflammatory DiseaseDocument5 paginiPelvic Inflammatory DiseaseRahma Rafina100% (2)
- Puerperal InfectionsDocument53 paginiPuerperal InfectionsNeharika KumariÎncă nu există evaluări
- MCN II Puerperal Infection 1Document23 paginiMCN II Puerperal Infection 1Rafik LakhdarÎncă nu există evaluări
- Chorioamnionitis: Intra Amniotic Infection (Disease Study)Document7 paginiChorioamnionitis: Intra Amniotic Infection (Disease Study)Aprilyn ay-ayenÎncă nu există evaluări
- Infectious Conditions & Hyperemesis Gravidarium: WrightDocument26 paginiInfectious Conditions & Hyperemesis Gravidarium: WrightNathaniel AdjeiÎncă nu există evaluări
- 5-Pelvic Imflamatory DiseasesDocument10 pagini5-Pelvic Imflamatory DiseasesTouseeq ManzoorÎncă nu există evaluări
- Puerpral SepsisDocument5 paginiPuerpral SepsisPriscilla Sarah PayneÎncă nu există evaluări
- Midwifery 102 Module 1Document10 paginiMidwifery 102 Module 1WynJoy NebresÎncă nu există evaluări
- Handouts of Complications of PostnatalDocument12 paginiHandouts of Complications of PostnatalAshish GuptaÎncă nu există evaluări
- Presented By:: Lantaya, Decyre Clare R. Emia, Julie MaeDocument22 paginiPresented By:: Lantaya, Decyre Clare R. Emia, Julie MaeNiña Jean Tormis AldabaÎncă nu există evaluări
- NCM 109 Module 8Document45 paginiNCM 109 Module 8capoyljtÎncă nu există evaluări
- BY:-Shalini Joshi M.SC NURSING Ist Year S.C.O.N. DehradunDocument52 paginiBY:-Shalini Joshi M.SC NURSING Ist Year S.C.O.N. DehradunshravaniÎncă nu există evaluări
- WEEK 8-NCM 109 LECTURE-PPTX With Recorded DiscussionDocument35 paginiWEEK 8-NCM 109 LECTURE-PPTX With Recorded DiscussionMa. Isabel A. EnriquezÎncă nu există evaluări
- Abnormalpuerperium 190328060723 1Document126 paginiAbnormalpuerperium 190328060723 1Preeti ChouhanÎncă nu există evaluări
- Pathophysiology: EndometritisDocument8 paginiPathophysiology: EndometritisBrett StevensonÎncă nu există evaluări
- Puerperium:: Psychological DisordersDocument5 paginiPuerperium:: Psychological DisordersManisha ThakurÎncă nu există evaluări
- Preterm / Premature Labor: EtiologyDocument8 paginiPreterm / Premature Labor: EtiologyCheney BalbuenaÎncă nu există evaluări
- Seminar G2 (Early Trimester Pregnancy Vaginal Bleeding)Document47 paginiSeminar G2 (Early Trimester Pregnancy Vaginal Bleeding)Chalie MequanentÎncă nu există evaluări
- Puerperal SepsisDocument30 paginiPuerperal Sepsisjonaa2564Încă nu există evaluări
- Puerperial PyrexiaDocument4 paginiPuerperial PyrexiaSyaira TanjidÎncă nu există evaluări
- Definition-: Pelvic Inflammatory Disease (PID) Is A Sexually Transmitted Inflammatory Condition of TheDocument7 paginiDefinition-: Pelvic Inflammatory Disease (PID) Is A Sexually Transmitted Inflammatory Condition of TheanweshaÎncă nu există evaluări
- puerperium 安红敏(II)Document20 paginipuerperium 安红敏(II)sanjivdas100% (1)
- MiscarriageDocument38 paginiMiscarriagezianab aliÎncă nu există evaluări
- Utis in Pregnancy: Rachael Mweigwa NakimuliDocument55 paginiUtis in Pregnancy: Rachael Mweigwa NakimuliRuva Oscass JimmyÎncă nu există evaluări
- Presented By: Don Leo M Dela Pe A BSN Ii-BDocument17 paginiPresented By: Don Leo M Dela Pe A BSN Ii-BDon Leo Dela PeñaÎncă nu există evaluări
- Abnormalitie S of The PuerperiumDocument59 paginiAbnormalitie S of The PuerperiumVincent Maralit MaterialÎncă nu există evaluări
- Puerperal Infections Group Report CMCR LectureDocument44 paginiPuerperal Infections Group Report CMCR LectureFERRER, JENNYFER S.Încă nu există evaluări
- Topics Today: Normal Puerperium Diseases of Puerperium Ectopic Pregnancy AbortionDocument52 paginiTopics Today: Normal Puerperium Diseases of Puerperium Ectopic Pregnancy AbortionBitto_Singh_5952Încă nu există evaluări
- Puerperal InfectionDocument11 paginiPuerperal InfectionceceyusenaÎncă nu există evaluări
- Puerperal PyrexiaDocument4 paginiPuerperal PyrexiaLulano MbasuÎncă nu există evaluări
- AbortionDocument67 paginiAbortionaneley cherinetÎncă nu există evaluări
- Brief DescriptionDocument7 paginiBrief DescriptionPrincess Pilove GawongnaÎncă nu există evaluări
- Nursing Care of Clients With Reproductive Health ProblemsDocument100 paginiNursing Care of Clients With Reproductive Health ProblemsHassen ZabalaÎncă nu există evaluări
- Abnormalities of The PuerperiumDocument59 paginiAbnormalities of The PuerperiumVincent Maralit MaterialÎncă nu există evaluări
- Presentation Abnormal PuerperiumDocument52 paginiPresentation Abnormal PuerperiumTesfaye AbebeÎncă nu există evaluări
- AmysaDocument14 paginiAmysaawanisfauzi90Încă nu există evaluări
- Lecture 2 MidtermDocument65 paginiLecture 2 MidtermKyla Desiree BedienesÎncă nu există evaluări
- Obsetrics and GynaecologyDocument7 paginiObsetrics and GynaecologyAbedinego MalukaÎncă nu există evaluări
- ALTERED POST PARTUM Complications Nursing Lecture and Care PlanDocument13 paginiALTERED POST PARTUM Complications Nursing Lecture and Care PlanKristelle Joy Capili SicatÎncă nu există evaluări
- UTI in Pregnancy - 071923Document14 paginiUTI in Pregnancy - 071923allanfocus91Încă nu există evaluări
- Septicabortion 190712153248Document31 paginiSepticabortion 190712153248berhanu nathanielÎncă nu există evaluări
- Pelvic Inflammatory DiseaseDocument9 paginiPelvic Inflammatory DiseaseanweshaÎncă nu există evaluări
- DEFINITION: Abortion Is The Expulsion or Extraction From Its MotherDocument10 paginiDEFINITION: Abortion Is The Expulsion or Extraction From Its MothermOHAN.SÎncă nu există evaluări
- Female Urinary Tract Infections in Clinical PracticeDe la EverandFemale Urinary Tract Infections in Clinical PracticeBob YangÎncă nu există evaluări
- Proposal Letter SpiritualityDocument11 paginiProposal Letter SpiritualityIrish Jane Bayle CubilloÎncă nu există evaluări
- SpiritualityDocument3 paginiSpiritualityIrish Jane Bayle CubilloÎncă nu există evaluări
- CHNDocument1 paginăCHNIrish Jane Bayle CubilloÎncă nu există evaluări
- Chole CaseDocument35 paginiChole CaseIrish Jane Bayle CubilloÎncă nu există evaluări
- Entamoeba HistolyticaDocument6 paginiEntamoeba HistolyticaIrish Jane Bayle CubilloÎncă nu există evaluări
- Project in Microbiolog Y: Submitted To: Yolanda Ilagan Ph. D Submitted By: Irish Jane B. Cubillo BSN 2-2Document28 paginiProject in Microbiolog Y: Submitted To: Yolanda Ilagan Ph. D Submitted By: Irish Jane B. Cubillo BSN 2-2Irish Jane Bayle CubilloÎncă nu există evaluări
- Revise Ros, Pe & PathoDocument8 paginiRevise Ros, Pe & PathoIrish Jane Bayle CubilloÎncă nu există evaluări
- Patient AnalysisDocument6 paginiPatient AnalysisIrish Jane Bayle CubilloÎncă nu există evaluări
- Integumentary System: By: Kelieraine U. BonDocument48 paginiIntegumentary System: By: Kelieraine U. BonIrish Jane Bayle CubilloÎncă nu există evaluări
- Giant Cell Tumor of Bone - An Overview: Current Concepts ReviewDocument8 paginiGiant Cell Tumor of Bone - An Overview: Current Concepts ReviewDwi fitria nivaÎncă nu există evaluări
- Taylan Competency NeedsDocument32 paginiTaylan Competency NeedsLovejoice Cha NnelÎncă nu există evaluări
- Travel Nurse Pdf1Document2 paginiTravel Nurse Pdf1Med NetÎncă nu există evaluări
- K3 Bidang Pertanian ILO PDFDocument350 paginiK3 Bidang Pertanian ILO PDFSufyan StauriÎncă nu există evaluări
- 00 - 7565 SigmaTherm 350Document3 pagini00 - 7565 SigmaTherm 350Elcio VilanculoÎncă nu există evaluări
- Sps PPR CleaningDocument5 paginiSps PPR CleaningManutençãoTI TechÎncă nu există evaluări
- Nursing Skills ChecklistDocument8 paginiNursing Skills Checklistapi-353656227Încă nu există evaluări
- Reflection PaperDocument27 paginiReflection PaperBon Ryan LeonardoÎncă nu există evaluări
- Psychometric Properties of The Consensus Sleep Diary in Those With Insomnia DisorderDocument19 paginiPsychometric Properties of The Consensus Sleep Diary in Those With Insomnia DisorderMondlTÎncă nu există evaluări
- Coca Cola The Water Stewardship and Replanish Report1 2012Document80 paginiCoca Cola The Water Stewardship and Replanish Report1 2012CSRmedia.ro NetworkÎncă nu există evaluări
- Tinnitus Today September 1986 Vol 11, No 3Document8 paginiTinnitus Today September 1986 Vol 11, No 3American Tinnitus AssociationÎncă nu există evaluări
- Progressive Addition Lens Design and The Short of Stature (Shan-Yu, S.)Document3 paginiProgressive Addition Lens Design and The Short of Stature (Shan-Yu, S.)Valentina PereaÎncă nu există evaluări
- Trends in Diagnosed Chronic Hepatitis B in A US Health System Population, 2006-2015Document8 paginiTrends in Diagnosed Chronic Hepatitis B in A US Health System Population, 2006-2015farid ahmadÎncă nu există evaluări
- BW Health-5Document2 paginiBW Health-5Michael JaballasÎncă nu există evaluări
- Pandakaking-Puti: KampupotDocument10 paginiPandakaking-Puti: KampupotgosmileyÎncă nu există evaluări
- Share FORM 10 - Workplace Application Evaluation ToolDocument3 paginiShare FORM 10 - Workplace Application Evaluation ToolRocel Ann CarantoÎncă nu există evaluări
- Importance of An Active LifestyleDocument2 paginiImportance of An Active LifestyleDreamCatcher Insommia18Încă nu există evaluări
- Table Saw Safety FinalDocument24 paginiTable Saw Safety Finalvolatileyasser100% (1)
- Fistula in AnoDocument17 paginiFistula in Anoapi-216828341Încă nu există evaluări
- Medical Examiner'S Confidential ReportDocument2 paginiMedical Examiner'S Confidential ReportParesh BorboruahÎncă nu există evaluări
- S.N o Name of Drug Recommended Paediatrics Dose Strength 1.: CPM - 2 mg/5mlDocument3 paginiS.N o Name of Drug Recommended Paediatrics Dose Strength 1.: CPM - 2 mg/5mlmrs raamÎncă nu există evaluări
- Applying A Feminist Lens To Indias Foreign Policy A Compendium of EssaysDocument124 paginiApplying A Feminist Lens To Indias Foreign Policy A Compendium of EssaysRasced AliÎncă nu există evaluări
- Family Reunification Plan Template FINAL 8-31-17 Incl. Appendices Pages All PortraitDocument146 paginiFamily Reunification Plan Template FINAL 8-31-17 Incl. Appendices Pages All PortraitLloyd Angelo SobredillaÎncă nu există evaluări