Documente Academic
Documente Profesional
Documente Cultură
Role of Hyaluronic Acid and Laminin As Serum Markers For Predicting Significant Fibrosis in Patients With Chronic Hepatitis B
Încărcat de
Mamad Trihatmowidjoyo0 evaluări0% au considerat acest document util (0 voturi)
27 vizualizări18 paginiHyaluronic acid and laminin as serum markers for predicting significant fibrosis in patients with chronic hepatitis B. Liver biopsy has been considered the gold standard for staging and grading hepatic disease. HA is a glycosaminoglycan, which is mostly synthesized by liver stellate cells and degraded by sinusoidal endothelial cells.
Descriere originală:
Titlu original
20-10-2013.ppt
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PPT, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentHyaluronic acid and laminin as serum markers for predicting significant fibrosis in patients with chronic hepatitis B. Liver biopsy has been considered the gold standard for staging and grading hepatic disease. HA is a glycosaminoglycan, which is mostly synthesized by liver stellate cells and degraded by sinusoidal endothelial cells.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPT, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
27 vizualizări18 paginiRole of Hyaluronic Acid and Laminin As Serum Markers For Predicting Significant Fibrosis in Patients With Chronic Hepatitis B
Încărcat de
Mamad TrihatmowidjoyoHyaluronic acid and laminin as serum markers for predicting significant fibrosis in patients with chronic hepatitis B. Liver biopsy has been considered the gold standard for staging and grading hepatic disease. HA is a glycosaminoglycan, which is mostly synthesized by liver stellate cells and degraded by sinusoidal endothelial cells.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPT, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 18
Muhammad Trihatmowijoyo Bundjali
GASTRO ENTERO HEPATAL DIVISION
DEPARTMENT OF INTERNAL MEDICINE
AIRLANGGA UNIVERSITY SCHOOL OF MEDICINE-Dr SOETOMO HOSPITAL
SURABAYA
2013
Role of hyaluronic acid and laminin as
serum markers for predicting significant
fibrosis in patients with chronic hepatitis B
BRAZ J INFECT DIS. 2012;16(1):9-14
Feng Lia*, Chang-Lai Zhub, Hong Zhanga, Hua Huanga, Qun
Weia, Xiang Zhua, Xiao-Yang Chenga
Jounal Reading
The prognosis and clinical treatment of chronic liver disease
depends greatly on the progression of liver fibrosis, which is
resulted from the loss of normal liver cell function due to
disorganized over-accumulation of extra-cellular matrix (ECM)
components in the liver.
For many years, liver biopsy has been considered the gold
standard for staging and grading hepatic fibrosis and
inflammation. However, the procedure is associated with
complications such as bleeding, infection, damage to liver tissue,
etc,
Introduction
The ECM components in the liver include non-collagenous
glycoproteins such as hyaluronic acid (HA), laminin (LN) and
proteoglycans, etc.
HA is a glycosaminoglycan, which is mostly synthesized by hepatic
stellate cells and degraded by sinusoidal endothelial cells.
LN is synthesized by hepatocytes and sinusoidal cells, which is
one of the main glycoproteins of the basement membrane.
This study, we aimed to evaluate serum HA and LN levels as
potential indicators of significant fibrosis in patients with chronic
hepatitis B (CHB) according to the Metavir scoring-system.
Introduction
Subjects
87 patients from Affiliated Hospital of Nantong University with
chronic hepatitis B, positive serologic tests for serum HBsAg for at
least 6 months, 49 men and 38 women, median age 38.4.
These patients were with an indication for percutaneous liver
biopsy, for assessment of the severity of liver fibrosis.
Liver transplantation, gastrointestinal bleeding and other chronic
liver diseases were excluded.
19 blood donors Healthy subjects had normal serum levels of
regular biochemical parameters such as ALT, AST and ALP, etc, and
with no chronic liver disease was used as a control group.
Methodes
Histology
All liver biopsies were performed with a suction needle (18G,
Angiomed Corporation German).
All biopsy specimens were analyzed by an experienced
pathologist blinded to the clinical results of the patients.
Liver fibrosis stages were evaluated semi-quantitatively according
to the Metavir scoring-system.
Fibrosis was staged on a scale of 0 to 4: F0=no fibrosis, F1=portal
fibrosis without septa, F2=portal fibrosis and few septa,
F3=numerous septa without cirrhosis, F4=cirrhosis.
Methodes
Determination of Serum Specimens
Liver function indexes were measured by an automatic
biochemistry analyzer, including ALT, AST, ALP, total bilirubin, -
glutamyltransferase (GGT) and albumin (ALB).
Methodes
Statistical Analysis
Independent-samples t-test was used for analysis of the
differences between two groups.
Subgroups (five stages of liver fibrosis) and healthy controls.
Correlations were assessed by Spearmans correlation coefficient.
The ROC curves were constructed to study the absence and
presence of significant fibrosis (F 2). The cut-off values were
determined with ROC curve procedure.
Methodes
According to the Metavir scoring-system, the fibrosis stages on
liver biopsy was
F0 in 13 patients (14.9%),
F1 in 17 (19.5%),
F2 in 25 (28.7%),
F3 in 23 (26.4%), and
F4 in 9 (10.3%) in this study.
Thus, a total of 57 patients (65.5%) had significant fibrosis ( F2).
Results
The results through box plots showed that serum HA and LN concentrations
increased significantly with the stage of hepatic fibrosis (Figs. 1 and 2), and
the highest values of HA and LN were all found in cirrhotic patients.
For significant fibrosis (F 2), Figs. 3 and 4 show the distribution of HA and LN concentrations
in controls and CHB patients by fibrosis stage (F0-F1, F2-F4), respectively. Significant
differences of serum HA and LN levels were found in F2-F4 group in comparison with those in
F0-F1 group (p < 0.001) and controls (p < 0.001), respectively.
To predict significant fibrosis
(F 2), the area under the
curve (AUC) for serum HA
and LN was 0.909 (95% CI:
0.8470.971) and 0.815 (95%
CI: 0.7120.917), respectively
(Fig. 5).
Results
Fig. 6 was an In/In plot of
serum HA levels vs. serum LN
concentration for all 87 CHB
patients. In Fig. 6, the
capability of two variables to
discriminate completely
between F2-F4 group and F0-
F1 group was readily
appreciable.
Results
Details were shown in Table 1, in which the performance of combinations of
HA and LN by serial and parallel tests has also been shown respectively.
Serial tests showed a perfect specificity and PPV of 100%, but at the same
time sensitivity declined to 63.2% and LR+ increased to 18.9. Parallel tests
revealed a good sensitivity of 94.7%, NPV to 86.4%, while LR- declined to
0.08.
Results
In Table 2, some serum biochemical indexes were chosen as the predictors
of significant fibrosis, none of which had shown high diagnostic
performance.
Results
Liver biopsy fails to satisfy the more and more pronounced need
for a rapid, safe and repeatable tool to monitor the fibrogenic
progression of chronic liver disease
We found that as liver fibrosis progresses, there is a significantly
increase of serum HA and LN concentrations, and the highest
values of HA and LN were all found in cirrhotic group (F=4).
In addition, HA and LN levels showed positive correlation with the
stages of liver fibrosis in CHB patients (HA: r = 0.875, p < 0.001;
LN: r = 0.610, p < 0.001).
Discussion
The increased of serum HA and LN levels, components of ECM,
might indicate of chronic liver injury, leading to architectural
changes the liver parenchyma that causes liver fibrosis eventually.
HA has been described as a single parameter or as a major
member of several fibrosis indexes for the noninvasive
assessment of fibrosis in various chronic liver diseases in the past
few years.
In our study, HA levels at its best cut-off value of 185.3 ng/mL for
predicting significant fibrosis showed a high diagnostic
performance, especially.
It suggested that HA as a biomarker could predict significant
fibrosis at its optimal cut-off value.
Discussion
Our results showed that serum LN concentrations was moderately
accurate at the diagnosis of significant fibrosis, which could be
unacceptable for excluding significant fibrosis.
The results of The performance of combined HA and LN for
predicting significant fibrosis showed a perfect specificity and
positive predictive value (PPV) of 100%, which could be
acceptable for the definite diagnosis of significant fibrosis.
In conclusion, increased serum HA and LN concentrations showed
positive correlation with the stages of liver fibrosis. Detection of
serum HA and LN in prediction of significant fibrosis showed good
diagnostic performance.
Discussion
THANK YOU
S-ar putea să vă placă și
- Bmri2019 3951574Document10 paginiBmri2019 3951574Anonymous 1EQutBÎncă nu există evaluări
- The Relation Between Liver Histopathology and GGT Levels in Viral Hepatitis: More Important in Hepatitis BDocument5 paginiThe Relation Between Liver Histopathology and GGT Levels in Viral Hepatitis: More Important in Hepatitis BTanveerÎncă nu există evaluări
- Pattern of Elevated Serum Alkaline Phosphatase (ALP) Levels in Hospitalized PatientsDocument7 paginiPattern of Elevated Serum Alkaline Phosphatase (ALP) Levels in Hospitalized PatientsDannyÎncă nu există evaluări
- Literature Collection FinalDocument11 paginiLiterature Collection FinalNatarajan NalanthÎncă nu există evaluări
- World Journal Of: HepatologyDocument12 paginiWorld Journal Of: HepatologywiwiÎncă nu există evaluări
- Factores Predict Ores en NASHDocument7 paginiFactores Predict Ores en NASHkukito77Încă nu există evaluări
- PAPAS Predict Liver FibrosisDocument7 paginiPAPAS Predict Liver Fibrosisemilya007Încă nu există evaluări
- Evaluation of Serum Hyaluronic Acid Level and Hyaluronidase Activity in Acute and Chronic Hepatitis CDocument7 paginiEvaluation of Serum Hyaluronic Acid Level and Hyaluronidase Activity in Acute and Chronic Hepatitis CRaja SharmaÎncă nu există evaluări
- Liver Function Tests and How To Relate ThemDocument82 paginiLiver Function Tests and How To Relate ThemG VenkateshÎncă nu există evaluări
- 1 s2.0 S097368831200031X MainDocument7 pagini1 s2.0 S097368831200031X MainNastitiÎncă nu există evaluări
- Changes in Urine Volume and Serum Albumin in Incident Hemodialysis PatientsDocument12 paginiChanges in Urine Volume and Serum Albumin in Incident Hemodialysis Patientsmelda lestari haidirÎncă nu există evaluări
- Alswaff 2012Document6 paginiAlswaff 2012Sri IriantiÎncă nu există evaluări
- Hepatic Steatosis and Fibrosis in Chronic Hepatitis C in TaiwanDocument5 paginiHepatic Steatosis and Fibrosis in Chronic Hepatitis C in TaiwansaadÎncă nu există evaluări
- Platelet Role in Liver FibrosisDocument6 paginiPlatelet Role in Liver FibrosisLaila Kurnia PramonoÎncă nu există evaluări
- ACG Abnormal Liver Chemistries Guideline SummaryDocument16 paginiACG Abnormal Liver Chemistries Guideline SummaryDanuÎncă nu există evaluări
- Liver Function TestsDocument70 paginiLiver Function TestsG Venkatesh100% (5)
- Newsletter10-1 SebiaDocument4 paginiNewsletter10-1 SebiaNidiam2100% (1)
- AGA DDSEP 10 Chapter 6 QA HepatologyDocument42 paginiAGA DDSEP 10 Chapter 6 QA HepatologyHima AlqahtaniÎncă nu există evaluări
- A - Fetoprotein Level-Dependent Early Hepatitis B Surface Antigen Decline During Entecavir Therapy in Chronic Hepatitis B With Hepatitis FlareDocument8 paginiA - Fetoprotein Level-Dependent Early Hepatitis B Surface Antigen Decline During Entecavir Therapy in Chronic Hepatitis B With Hepatitis FlareShrinivas YuvanÎncă nu există evaluări
- Clinical and Histologic Spectrum of Nonalcoholic Fatty Liver Disease Associated With Normal ALT ValuesDocument7 paginiClinical and Histologic Spectrum of Nonalcoholic Fatty Liver Disease Associated With Normal ALT ValuesndocÎncă nu există evaluări
- Ahmed 2004Document7 paginiAhmed 2004Sri IriantiÎncă nu există evaluări
- Etm 15 03 3074Document6 paginiEtm 15 03 3074Arini NurlelaÎncă nu există evaluări
- Secretory-Defect Distal Renal Tubular Acidosis Is Associated With Transporter Defect in H - Atpase and Anion Exchanger-1Document8 paginiSecretory-Defect Distal Renal Tubular Acidosis Is Associated With Transporter Defect in H - Atpase and Anion Exchanger-1Grace Antonette PatiÎncă nu există evaluări
- Alphafetoprotein: An Obituary: EditorialDocument3 paginiAlphafetoprotein: An Obituary: EditorialRaphael Moro Villas BoasÎncă nu există evaluări
- Hepatic Computed Tomography and Cholangiography by Use of Gadoxetic Acid in Healthy CatsDocument11 paginiHepatic Computed Tomography and Cholangiography by Use of Gadoxetic Acid in Healthy CatsAlejandro Estrada RiosÎncă nu există evaluări
- Performance of Non-Invasive Models of Fibrosis in Predicting Mild To Moderate Fibrosis in Patients With Non-Alcoholic Fatty Liver DiseaseDocument8 paginiPerformance of Non-Invasive Models of Fibrosis in Predicting Mild To Moderate Fibrosis in Patients With Non-Alcoholic Fatty Liver DiseaseChausarPutraBenagilÎncă nu există evaluări
- DR +Niket+Sonpal+-+Research+AbstractsDocument7 paginiDR +Niket+Sonpal+-+Research+AbstractsamiqtÎncă nu există evaluări
- The Level of Serum Albumin Is Associated With Renal Prognosis in Patients With Diabetic NephropathyDocument28 paginiThe Level of Serum Albumin Is Associated With Renal Prognosis in Patients With Diabetic NephropathyAdeÎncă nu există evaluări
- Serological Markers of Liver CancerDocument9 paginiSerological Markers of Liver Cancerrizqi_cepiÎncă nu există evaluări
- Journal Reading - FitaDocument22 paginiJournal Reading - FitaFita FitriantiÎncă nu există evaluări
- Noninvasive Evaluation of Liver FibrosisDocument70 paginiNoninvasive Evaluation of Liver FibrosisiriscelÎncă nu există evaluări
- Liver function tests, ultrasound, biopsy guide to interpreting resultsDocument14 paginiLiver function tests, ultrasound, biopsy guide to interpreting resultsshihochan100% (2)
- Ultrasound Spleen Morphology, But Not Vascular Liver Doppler MeasuresDocument1 paginăUltrasound Spleen Morphology, But Not Vascular Liver Doppler MeasuresdenisegmeloÎncă nu există evaluări
- Best of NAFLD Summit 2019Document25 paginiBest of NAFLD Summit 2019Med. TrackÎncă nu există evaluări
- EBGH Examination Gastroenterology Sample Questions Clinical QDocument52 paginiEBGH Examination Gastroenterology Sample Questions Clinical QPushpa DhruvÎncă nu există evaluări
- Caee Study For Clinical RotationsDocument8 paginiCaee Study For Clinical RotationseyesontheskyÎncă nu există evaluări
- Plasma Leptin Levels in Rats With PancreatitisDocument6 paginiPlasma Leptin Levels in Rats With PancreatitisAndykaYayanSetiawanÎncă nu există evaluări
- Phlebotomy Procedures and Clinical Analysis TestsDocument20 paginiPhlebotomy Procedures and Clinical Analysis TestsVera June RañesesÎncă nu există evaluări
- Low Alt CKDDocument5 paginiLow Alt CKDFebianti RukmanaÎncă nu există evaluări
- Afp 170422071501Document15 paginiAfp 170422071501ZaenNiasÎncă nu există evaluări
- Afp 170422071501Document15 paginiAfp 170422071501ZaenNiasÎncă nu există evaluări
- Bioscientific Review (BSR) : The Correlation Between Alpha-Fetoprotein and Liver Function TestsDocument10 paginiBioscientific Review (BSR) : The Correlation Between Alpha-Fetoprotein and Liver Function TestsUMT JournalsÎncă nu există evaluări
- Reduced Albumin Dosing During ParacentesisDocument6 paginiReduced Albumin Dosing During ParacentesisLuis Gerardo Alcalá GonzálezÎncă nu există evaluări
- Clase 7 Articulo Ejemplo 11-03-15Document8 paginiClase 7 Articulo Ejemplo 11-03-15Betzi HannlyÎncă nu există evaluări
- Pathophysiology of Hypertrophic PyloricDocument9 paginiPathophysiology of Hypertrophic PyloricVașadi Razvan CristianÎncă nu există evaluări
- Elevation of The Glycated Albumin To Glycated Hemoglobin Atio To Glycated Hemoglobin Atio To Glycated Hemoglobin Atio During The Progression of Hepatitis C Virus Related Liver FibrosisDocument7 paginiElevation of The Glycated Albumin To Glycated Hemoglobin Atio To Glycated Hemoglobin Atio To Glycated Hemoglobin Atio During The Progression of Hepatitis C Virus Related Liver FibrosistrimardiyanaisyanÎncă nu există evaluări
- 10.1177 - 2050640618792819 Pubmed PDFDocument613 pagini10.1177 - 2050640618792819 Pubmed PDFZakiyyah PutriÎncă nu există evaluări
- 3.5. Diagnosis and StagingDocument2 pagini3.5. Diagnosis and StagingSarahÎncă nu există evaluări
- A Randomized, Controlled Trial of Maintenance Interferon Therapy For Patients With Chronic Hepatitis C Virus and PersisDocument9 paginiA Randomized, Controlled Trial of Maintenance Interferon Therapy For Patients With Chronic Hepatitis C Virus and Persisgrace liwantoÎncă nu există evaluări
- 2019 Article 1205Document6 pagini2019 Article 1205zahra h f aÎncă nu există evaluări
- AnnGastroenterol 30 217 PDFDocument8 paginiAnnGastroenterol 30 217 PDFhusni gunawanÎncă nu există evaluări
- IJSCR 109192 Session ReportDocument11 paginiIJSCR 109192 Session ReportFarhan ShahzadÎncă nu există evaluări
- Salmonella hepatitis analysisDocument3 paginiSalmonella hepatitis analysisWawan BwÎncă nu există evaluări
- PdyDocument9 paginiPdysike1977Încă nu există evaluări
- Polycythemia Vera With Extremely High Serum Erythropoietin: Case ReportDocument6 paginiPolycythemia Vera With Extremely High Serum Erythropoietin: Case ReportTia Amalia Puti RenaeryÎncă nu există evaluări
- New ALT Reference Intervals For Children and AdultsDocument2 paginiNew ALT Reference Intervals For Children and AdultsYang YuÎncă nu există evaluări
- Prevalence of Anaemia in Decompensated Chronic Liver DiseaseDocument5 paginiPrevalence of Anaemia in Decompensated Chronic Liver DiseaseElang SudewaÎncă nu există evaluări
- Significant Haemoglobinopathies: Guidelines For Screening and DiagnosisDocument15 paginiSignificant Haemoglobinopathies: Guidelines For Screening and DiagnosisFiky setiawanÎncă nu există evaluări
- Assesmentof Fibro Q Test, AAR & APRI Indices As Markers of Fibrosis in Chronic Liver DiseaseDocument5 paginiAssesmentof Fibro Q Test, AAR & APRI Indices As Markers of Fibrosis in Chronic Liver Diseaseferdinan goutamaÎncă nu există evaluări
- Complementary and Alternative Medical Lab Testing Part 8: UrologyDe la EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyEvaluare: 3 din 5 stele3/5 (1)
- Exercise Improves Cardiovascular Control in A Model of DislipidemiaDocument5 paginiExercise Improves Cardiovascular Control in A Model of DislipidemiaMamad TrihatmowidjoyoÎncă nu există evaluări
- The Anemia in Continuous Ambulatory Peritoneal DialysisDocument5 paginiThe Anemia in Continuous Ambulatory Peritoneal DialysisMamad TrihatmowidjoyoÎncă nu există evaluări
- Statins and Beyond Concurrent Strategies For Prevention of Cardiovascular Disease in Patients WiDocument17 paginiStatins and Beyond Concurrent Strategies For Prevention of Cardiovascular Disease in Patients WiMamad TrihatmowidjoyoÎncă nu există evaluări
- Judith Blaine (Eds.) - Proteinuria - Basic Mechanisms, Pathophysiology and Clinical Relevance-Springer International Publishing (2016)Document147 paginiJudith Blaine (Eds.) - Proteinuria - Basic Mechanisms, Pathophysiology and Clinical Relevance-Springer International Publishing (2016)Rubén Casas BenítezÎncă nu există evaluări
- The Spectrum of Red Blood CellDocument6 paginiThe Spectrum of Red Blood CellMamad TrihatmowidjoyoÎncă nu există evaluări
- Erythropoietin RequirementsDocument7 paginiErythropoietin RequirementsMamad TrihatmowidjoyoÎncă nu există evaluări
- Impact of Metabolic Syndrome and Its Severity On Microvascular ComplicationsDocument5 paginiImpact of Metabolic Syndrome and Its Severity On Microvascular ComplicationsMamad TrihatmowidjoyoÎncă nu există evaluări
- Statins and Beyond Concurrent Strategies For Prevention of Cardiovascular Disease in Patients WiDocument17 paginiStatins and Beyond Concurrent Strategies For Prevention of Cardiovascular Disease in Patients WiMamad TrihatmowidjoyoÎncă nu există evaluări
- Review of Linagliptin For The Treatment of Type 2 DiabetesDocument13 paginiReview of Linagliptin For The Treatment of Type 2 DiabetesMamad TrihatmowidjoyoÎncă nu există evaluări
- Latest Strategy in Renal Anemia Management in Peritoneal Dialysis PatientsDocument5 paginiLatest Strategy in Renal Anemia Management in Peritoneal Dialysis PatientsMamad TrihatmowidjoyoÎncă nu există evaluări
- Glucose Prediction, IatrogeDocument6 paginiGlucose Prediction, IatrogeMamad TrihatmowidjoyoÎncă nu există evaluări
- 90-Article Text-458-1-10-20170910Document4 pagini90-Article Text-458-1-10-20170910Mamad TrihatmowidjoyoÎncă nu există evaluări
- Exercise Improves Cardiovascular Control in A Model of DislipidemiaDocument5 paginiExercise Improves Cardiovascular Control in A Model of DislipidemiaMamad TrihatmowidjoyoÎncă nu există evaluări
- Positive Association of Residual KidneyDocument9 paginiPositive Association of Residual KidneyMamad TrihatmowidjoyoÎncă nu există evaluări
- Renal Association Clinical Practice Guideline On Anaemia of Chronic Kidney DiseaseDocument29 paginiRenal Association Clinical Practice Guideline On Anaemia of Chronic Kidney DiseasemelvinÎncă nu există evaluări
- 017791Document57 pagini017791Miguel Chávez AmaroÎncă nu există evaluări
- 09 - On Being A Scientist - Ethics PDFDocument83 pagini09 - On Being A Scientist - Ethics PDFanita_shar29Încă nu există evaluări
- 90-Article Text-458-1-10-20170910Document4 pagini90-Article Text-458-1-10-20170910Mamad TrihatmowidjoyoÎncă nu există evaluări
- 09 - On Being A Scientist - Ethics PDFDocument83 pagini09 - On Being A Scientist - Ethics PDFanita_shar29Încă nu există evaluări
- 09 - On Being A Scientist - Ethics PDFDocument83 pagini09 - On Being A Scientist - Ethics PDFanita_shar29Încă nu există evaluări
- Worksheet Guideline - AGREE AppraisalDocument2 paginiWorksheet Guideline - AGREE AppraisalRoel SamaÎncă nu există evaluări
- 09 - On Being A Scientist - Ethics PDFDocument83 pagini09 - On Being A Scientist - Ethics PDFanita_shar29Încă nu există evaluări
- 09 - On Being A Scientist - Ethics PDFDocument83 pagini09 - On Being A Scientist - Ethics PDFanita_shar29Încă nu există evaluări
- Tumor MarkersDocument54 paginiTumor MarkersMamad TrihatmowidjoyoÎncă nu există evaluări
- Mild Cognitive ImpairmentDocument1 paginăMild Cognitive ImpairmentMamad TrihatmowidjoyoÎncă nu există evaluări
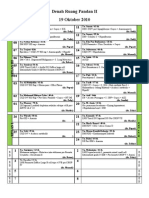
- Denah Ruang Pandan II Arsanto's Mode 101019Document2 paginiDenah Ruang Pandan II Arsanto's Mode 101019Mamad TrihatmowidjoyoÎncă nu există evaluări
- Pelatihan Dry NeedleDocument101 paginiPelatihan Dry NeedleAri SudarsonoÎncă nu există evaluări
- Tut 3Document3 paginiTut 3Bobet ReñaÎncă nu există evaluări
- Case StudyDocument6 paginiCase StudySarah McKayÎncă nu există evaluări
- Advance Airway MXDocument17 paginiAdvance Airway MXMardhiyah MusaÎncă nu există evaluări
- TabletDocument156 paginiTabletSiddharth Patel100% (2)
- PARAPHIMOSISDocument3 paginiPARAPHIMOSISEmmeline Dycangchon-GarmaÎncă nu există evaluări
- Jamapediatrics Baker 2023 Oi 220086 1677804711.8454Document8 paginiJamapediatrics Baker 2023 Oi 220086 1677804711.8454IKA 79Încă nu există evaluări
- Arti PDFDocument7 paginiArti PDFSuvidVijay FadanvisÎncă nu există evaluări
- Case Study Dr. Sisk LCA Gene Therapy MC 0005054 21NOV2022Document6 paginiCase Study Dr. Sisk LCA Gene Therapy MC 0005054 21NOV2022SALAH YOUNISÎncă nu există evaluări
- AcetazolamideDocument3 paginiAcetazolamidejeihanalkhairÎncă nu există evaluări
- Referat Cystoid Macular Edema Periode 17 Juni - 20 Juli 2019Document25 paginiReferat Cystoid Macular Edema Periode 17 Juni - 20 Juli 2019CharlotteGraceNusiferaÎncă nu există evaluări
- Europsko Istraživanje o Kvaliteti Vode Za KupanjeDocument28 paginiEuropsko Istraživanje o Kvaliteti Vode Za KupanjeIndex.hrÎncă nu există evaluări
- Ayurveda: The Ancient Science of LifeDocument23 paginiAyurveda: The Ancient Science of LifelavanyaÎncă nu există evaluări
- Australian Ironman Magazine July 2016 PDFDocument140 paginiAustralian Ironman Magazine July 2016 PDFgeorgeÎncă nu există evaluări
- Typical, Atypical Optic NeuritisDocument10 paginiTypical, Atypical Optic NeuritisScerbatiuc CristinaÎncă nu există evaluări
- Administering Intramuscular InjectionDocument11 paginiAdministering Intramuscular Injectionbwester2222Încă nu există evaluări
- NCP Deficient Fluid VolumeDocument5 paginiNCP Deficient Fluid VolumeCHRISTINE GRACE ELLOÎncă nu există evaluări
- RSBY Hospital Manual 28072010Document44 paginiRSBY Hospital Manual 28072010chimera03Încă nu există evaluări
- Gestational Trophoblastic DiseaseDocument37 paginiGestational Trophoblastic DiseaseOlisa 'phage' Onyebuchi100% (1)
- Clinical Management of Binocular Vision .24Document1 paginăClinical Management of Binocular Vision .24Ikmal ShahromÎncă nu există evaluări
- Discharge Planning and NCP SDocument8 paginiDischarge Planning and NCP SRainier RamosÎncă nu există evaluări
- Basal Cell Carcinoma - Pathophysiology and ManagementDocument6 paginiBasal Cell Carcinoma - Pathophysiology and ManagementReylan Garcia0% (1)
- Relational PsychotherapyDocument229 paginiRelational Psychotherapykhushi chopra 0050Încă nu există evaluări
- Approaches To Counselling: by Amala Mary JohnyDocument22 paginiApproaches To Counselling: by Amala Mary Johnyammu2805Încă nu există evaluări
- Nursing Care Plan: Priority No. 3Document2 paginiNursing Care Plan: Priority No. 3Pantaleon PacisÎncă nu există evaluări
- Indian Childhood CirrhosisDocument10 paginiIndian Childhood CirrhosisMona Morris89% (9)
- Vaayu Mudra-A Boon For Cerebral PalsyDocument9 paginiVaayu Mudra-A Boon For Cerebral PalsyDrRiitesh SinhaÎncă nu există evaluări
- Vancomycin Pharmacokinetics GuideDocument5 paginiVancomycin Pharmacokinetics GuidedrblondyÎncă nu există evaluări
- Proprioceptive Neuromuscular Facilitation: Vicky S. WardlawDocument44 paginiProprioceptive Neuromuscular Facilitation: Vicky S. WardlawPraneetha Nouduri100% (1)
- Coughlin CC Case Study IntroDocument3 paginiCoughlin CC Case Study Introapi-283315953100% (1)