Documente Academic
Documente Profesional
Documente Cultură
Osteomyelitis
Încărcat de
Ankit Agur100%(1)100% au considerat acest document util (1 vot)
280 vizualizări147 paginiOstemyelitis of all the bones
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PPTX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentOstemyelitis of all the bones
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPTX, PDF, TXT sau citiți online pe Scribd
100%(1)100% au considerat acest document util (1 vot)
280 vizualizări147 paginiOsteomyelitis
Încărcat de
Ankit AgurOstemyelitis of all the bones
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPTX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 147
Osteomyelitis
Nelaton (1834) : coined osteomyelitis
The root words osteon (bone) and myelo (marrow)
are combined with itis (inflammation) to define
the clinical state in which bone is infected with
microorganisms.
Definition
Osteomyelitis is defined as an inflammation of the
bone caused by an infecting organism.
The infection may be limited to a single portion of the
bone or may involve numerous regions, such as the
marrow, cortex, periosteum, and the surrounding soft
tissue.
The infection generally is due to a single organism,
but polymicrobial infections can occur.
- Osteomyelitis is divided into:
Acute osteomyelitis
Subacute osteomyelitis
Chronic osteomyelitis
There are certain types of named osteomyelitis;
Brodie's abscess
Chronic multifocal osteomyelitis
Sclerosing osteomyelitis of Garr
Classification
Based on duration of symptoms :
Acute, subacute , chronic (6 weeks)
Exogenous - open fractures, surgery (iatrogenic), or
contiguous spread from infected local tissue.
Hematogenous blood spread
Pyogenic and non pyogenic
Acute hematogenous osteomyelitis
Mainly a disease of children.
Adults are affected , when their resistance is lowered.
More common in males
Age distribution in children in bimodal
Younger than 2 yrs and 8-12 yrs.
History
First written documentation by hindu surgeons ,
charaka and sushrutha in 2500 B.C.
Hippocrates described the extrusion of sequestrum
Term OSTEOMYELITIS was coined by NELATON in
1834.
Etiology
May follow slight trauma
Infection from distant site like tonsils,lungs, middle
ear, septic tooth.
Excoriations , wounds, small suppurative infections of
skin, boils
Small pox, malaria, scarlet fever, measles, typhoid,
diptheria.
Infected umbilical cord in newborn.
In adults - urethral catheter, an indwelling arterial line
or a dirty needle and syringe.
Bacteriology
Staph aureus ( most common )
Streptococcus pyogenes
S.pneumoniae ( chronic skin infections)
Hemophilus influenzae (1-4 yrs)
Kingella kingae
E.coli, proteus
Pseudomonas ( IV drug abusers)
Salmonella typhi ( sickle cell disease)
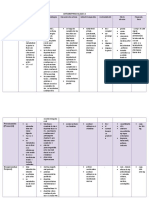
MOST COMMON CLINICAL
ASSOCIATION
MICROORGANISM
Frequent microorganism in any type of
osteomyelitis
Staph. aureus
Common in nosocomial infection Enterobacteriaceae, Pseudomonas
aeruginosa, candida spp.
Foreign bodyassociated infection Coagulase-negative staphylococci or
other skin flora, atypical
mycobacteria
Decubitus ulcers Streptococci and/or anaerobic
bacteria
Populations in which tuberculosis is
prevalent
Mycobacterium tuberculosis
Exposure to kittens Bartonella henselae
Immunocompromised patients
Aspergillus spp., Candida albicans, or
Mycobacteria spp.
Microorganisms Isolated from Patients with Osteomyelitis
Site
Bones of lower extremity are more
often affected.
Upper end tibia is most common
site
In femur, lower end is more prone.
In children, infection usually starts
at the metaphysis.
In children younger
than 2 years, some
blood vessels cross the
physis and may allow
the spread of infection
into the epiphysis.
Older children , physis
effectively acts as barrier
for the spread of
infection
Why metaphysis
Due to peculiar arrangement of the
blood vessels in that area
The non-anastomosing terminal
branches of the nutrient artery twist
back in hairpin loops before entering
the large network of sinusoidal veins;
the relative vascular stasis
consequent lowered oxygen tension
metaphysis has relatively fewer
phagocytic cells than the physis or
diaphysis.
Pathogenesis
In the metaphysis, nutrient arteries branch into
non-anastomosing capillaries under the
physis make a sharp loop before entering
venous sinusoids draining into the marrow (
Hair-pin Ends)
Blood flow, sluggish and provides an ideal
environment for bacterial seeding
Relative paucity of phagocytic cells in this area
Pathogenesis
Characteristic progression marked by inflammation,
suppuration, bone necrosis, reactive new bone
formation and, ultimately, resolution and healing or
else intractable chronicity.
Depending on virulence of organism the disease may
take three courses :
Patient displays good resistance mild infection , no
suppuration , organisms eradicated.
Organisms are more virulent a chronic abscess may
be formed.
Classical sequence of pyogenic inflammation,
suppuration and sequestration.
acute inflammatory reaction with vascular congestion, exudation of fluid
Infiltration of polymorphonuclear leucocytes
Rise in intraosseous pressure causing intense pain, obstruction to blood
flow and intravascular thrombosis.
By the second or third day, pus forms within the bone and forces its way
along the Volkmann canals
Infection spreads through haversian canals to periosteum forming a
SUBPERIOSTEAL abscess.
Infection spreads to the medullary canal and subsequently entire shaft.
Microscopic bone death due to vascular compromise, bacterial toxins and
leucocytic enzymes.
Pieces of dead bone may separate as sequestra varying in size from mere
spicules to large necrotic segments of the cortex
Combination of phagocytosis and osteoclastic resorption.
A small focus in cancellous bone may be completely resorbed
cortico-cancellous sequestrum will remain entombed, inaccessible to either
final destruction or repair.
new bone starts forming on viable surfaces in the bone and from the deep
layers of the stripped periosteum.
this new bone thickens to form a casement, or involucrum,
enclosing the sequestrum and infected tissue.
Persistant infection discharge of pus and spicules
through perforations (CLOACAE) in involucrum.
Sinus formation and chronic osteomyelitis.
In infants.
infection spreads to the epiphysis and from there into
the adjacent joint.
Physeal damage leading to retarded growth
Joint destruction and deformity
Exuberant periosteal reaction
Bizarre new bone formation.
In adults.
Usually follows an open injury, surgery or spread from
contiguous site.
True hematogenous uncommon usually affects
vertebra.
Infection spreads through vertebral end plate, discs
and adjacent vertebra.
In long bones, entire medullary cavity is spread
eroding the cortex.
Periosteal new bone formation is less than children.
Risk of fracture due to weak cortex.
Clinical features
Children :
Typically the child looks ill and feverish.
Pulse rate is high with fever
Severe pain and malaise
Refuse to use the limb
recent history of infection: a septic toe, a boil, a sore
throat or a discharge from the ear.
The hallmark of osteomyelitis is fever plus localised
bony tenderness
Clinical features
Tenderness in the joint
joint movement is restricted (pseudoparalysis).
Local redness and edema are late signs.
Clinical features - infants
Fails to thrive
Drowsy but irritable
Metaphyseal tenderness
Resistance to joint motion
Clinical features - adults
The commonest site for haematogenous infection is
the thoracolumbar spine.
history of some urological procedure followed by a
mild fever and backache.
Local tenderness is not very marked.
X-ray
During first week no bony abnormality.
soft tissue swelling and loss of fascial planes.
Earliest sign by second week
a faint extra-cortical outline due to periosteal new
bone formation.
Later periosteal thickening.
Regional osteoporosis
Localized segment of apparently increased density
Typical early bony changes include:
lytic lesions,
periosteal thickening
endosteal scalloping,
osteopenia,
loss of trabecular architecture,
and new bone apposition
- The destructive lytic lesion, usually occurs within 7 to 10
days .
- Followed by elevation of periosteum and layered new
bone formation after 3 to 6 weeks.
- The dead bone (i.e. sequestrum formation) occurs at 3-8
weeks.
Technitium scan
Highly sensitive
can confirm the diagnosis 24 to 48 hours after onset in
90% to 95% of patients.
Increased activity in both perfusion phase and bone
phase.
Can be used in conjunction with Gallium scans and
indium-111labeled leukocyte scans
Ultrasound
Can detect features of osteomyelitis several days earlier Xray
(predominately in children).
Acute osteomyelitis is recognized by elevation of the
periosteum by a hypoechoic layer
Soft tissue abscesses
hypoechoic or anechoic fluid collections, which may extend
around the bony contours.
Finally, cortical erosions can become apparent on US
MRI
CT
Delineate intramedullary and soft tissue involvement.
On MRI a
penumbra
sign has been
described on T1
spin-echo
images. This
probably
represents a
layer of
granulation
tissue. It is
strongly
suggestive of
osteomyelitis
Lab investigations
Elevated WBC counts.
Elevated CRP (within 12 24 hrs)
Elevated ESR (within 24 48 hrs)
Decreased Hb%
ASO titres may be raised.
Aspiration of pus or fluid for c/s
Blood cultures
Diagnosis
Children with acute bone pain and systemic signs of
sepsis should be considered to have acute
hematogenous Osteomyelitis until proved otherwise.
Diagnosis may be established if a patient fulfills two of
the following criteria:
1. Bone aspiration yield pus
2. Bacterial culture of bone or blood positive
3. Presence of the classical s/s of acute osteomyelitis
4. Radiographic changes typical for osteomyelitis.
Differential diagnosis
Cellulitis
Septic arthritis :
If CRP levels increase two to three fold after admission
constantly, suspect superseded septic arthritis.
Acute rheumatism.
Sickle cell crisis
Gauchers disease
Heamophilia
Prognosis
Organism : staph. Aureus infection is serious and
most common type.
Site : nearer to the trunk of the affected bone, more
serious is the prognosis.
Age : younger the child, outlook is grave.
Management
Supportive treatment for pain and dehydration.
Splintage of the affected part.
Appropriate antimicrobial therapy.
Surgical drainage.
General supportive treatment :
Analgesics for pain
Antipyretics
Adequate hydration
Splintage in comfortable position for joints.
Skin traction or plaster slab
Anti-microbial therapy
Blood and aspiration material are sent immediately for
examination and culture.
Neonates and infants up to 6 months of
age :
Against penicillin-resistant Staphylococcus aureus,
Group B streptococcus and Gram-negative organisms.
Drugs of choice are flucloxacillin plus a third-
generation cephalosporin like cefotaxime.
Children 6 months to 6 years of age :
Emperical treatment against H.influenzae.
combination of intravenous flucloxacillin and
cefotaxime or cefuroxime.
Older children and previously fit adults :
intravenous flucloxacillin and fusidic acid.
for a known streptococcal infection benzylpenicillin
allergic to penicillin :second- or third generation
cephalosporin.
Elderly and previously unfit patients :
risk of Gram-negative infections
combination of flucloxacillin and a second- or third-
generation cephalosporin.
Patients with sickle-cell disease :
salmonella and/or other Gram-negative organisms.
Chloramphenicol
Nowadays the antibiotic of choice is a third-generation
cephalosporin or a fluoroquinolone like ciprofloxacin.
Patients considered to be at risk of meticillin-resistant
Staphylococcus aureus (MRSA) infection :
intravenous vancomycin together with a third-
generation cephalosporin.
Drugs are administered intravenously until the
patients condition begins to improve and the CRP
values return to normal levels.
Normally it takes 2-4 weeks.
Oral antibiotic based upon sensitivity tests for another
3-6 weeks.
Prospective Evaluation of a Shortened Regimen of
Treatment for Acute Osteomyelitis and Septic Arthritis
in Children
Included 70 consecutive, eligible children aged 2 weeks to 14 years.
Staphylococci were the only organisms isolated in cases of
osteomyelitis
Found that 59% of children could be converted to oral therapy after
3 days of intravenous therapy and 86% after 5 days.
Established that 3 weeks of oral therapy was appropriate for those
patients who received 5 days or less intravenous treatment.
Journal of Pediatric Orthopaedics Issue: Volume 29(5), July/August 2009, pp 518-525
Surgery
The two main indications for surgery :
(1) the presence of an abscess requiring drainage
and
(2) failure of the patient to improve despite
appropriate intravenous antibiotic treatment.
Any abscess should be drained out.
any subperiosteal abscess : several small holes
should be drilled through the cortex into the
medullary canal.
Intramedullary abscess :
If intramedullary pus is found, a small window of bone
is removed.
The skin is closed loosely over drains
The limb is splinted.
The limb is protected for several weeks to prevent
pathological fracture.
Intravenous antibiotics should be continued
postoperatively.
Complications
Epiphyseal damage and altered bone growth.
Suppurative arthritis :
(1) in very young infants, in whom the growth disc is
not an impenetrable barrier;
(2) where the metaphysis is intracapsular, as in the
upper femur; or
(3) from metastatic infection.
Complications
Metastatic infection
Pathologic fracture
Chronic osteomyelitis
Bone abscess
Bacteremia
Overlying soft-tissue cellulitis
Draining soft-tissue sinus tracts
Growth disturbance
Subacute
osteomyelitis
Introduction
- It is a distinct type of osteomyelitis
- It has an insidious onset, mild symptoms, lack of systemic
reaction
- Its relative mildness is due to:
a) Organism being less virulent OR
b) Patient more resistant OR
c) (Both)
- Subacute osteomyelitis occurs in a much wider variety of
bones than acute osteomyelitis
- Most common site: Distal femur, Proximal & Distal Tibia
Causative Organism
a) Staphyloccocus aureus (30-60%)
b) Others (Streptococcus, Pseudomonas, Haemophilus
influenzae)
c) Pseudomonas aeruginosa (IV drug user)
d) Salmonella (patient with sickle cell anaemia)
Gram positive
Staphylococcus aureus
Clinical Features
a) Pain (several weeks / months)
b) Limping
c) Swelling & Local tenderness
d) Muscle wasting
e) Body temperature usually normal (no fever)
Modified Classification of Subacute Osteomyelitis
Type I Metaphyseal
Ia - punched-out central metaphyseal lesion
Ib - eccentric metaphyseal cortical erosion
Type II Diaphyseal
IIa - localized cortical and periosteal reaction
IIb - medullary abscess in the diaphysis without cortical destruction but
with onionskin periosteal reaction
Type III Epiphyseal
IIIa - primary epiphyseal osteomyelitis
IIIb - lesion that crosses the epiphysis and involves both the epiphysis
and the metaphysis
Type IV - Metaphyseal equivalent
IVa - vertebral body with an erosive or destructive process
IVb - involves the flat bones of the pelvis
IVc - involves the small bones, such as the tarsal bones
Sub acute osteomyelitis classification
Type Gledhill Classification Robert et al. Classification
I Solitary localized zone of
radiolucency surrounded by reactive
new bone formation
IaPunched-out radiolucency
IbPunched-out radiolucent
lesion with sclerotic margin
II Metaphyseal radiolucencies with
cortical erosion
III Cortical hyperostosis in diaphysis;
no onion skinning
Localized cortical and periosteal
reaction
IV Subperiosteal new bone and onion
skin layering
Onion skin periosteal reaction
V Central radiolucency in epiphysis
VI Destructive process involving
vertebral body
Robert et al classificatiomn
A: Type IA - punched-out metaphyseal
lesion
B: Type IB -similar to type IA, with
sclerotic cortex.
C: Type II erosion os metaphyseal
bone,
D: Type III -localized cortical and
periosteal reactions,
E: Type IV - produce onionskinlike
periosteal reactions in the diaphysis
F: Type V - epiphyseal erosions.
G: Type VI - involve the vertebral
bodies.
Investigation
a) X-ray (may resemble osteoid osteoma / malignant
bone tumour)
b) Biopsy
c) Fluid aspiration & culture
d) ESR raised
e) WBC may be normal
Classification-
Acute hematogenous Osteomyelitis
Subacute hematogenous Osteomyelitis
Parameters
Subacute Acute
WBC Frequently normal Frequently elevated
ESR Frequently elevated Frequently elevated
Blood Cultures Rarely Positive 50% Positive
Bone Cultures 60% Positive 90% Positive
Localization Diaphysis, metaphysis,
epiphysis, cross physis
Metaphysis
Pain Mild to Moderate Severe
Systemic Illness No Fever, malaise
Loss of function No or minimal Marked
Prior antibiotics 30%-40% Occasional
Initial radiograph Frequently abnormal Bone normal
Radiological Finding
Classic Brodies abscess
- Described by Brodie in 1832.
- it is an intraosseous abscess walled by reactive bone
- A circumscribed, round/oval cavity containing pus
and pieces of dead bone (sequestra) surrounded
sclerosis
- Most commonly seen in tibial / femoral metaphysis
*may occur in epiphysis / cuboidal bone (eg:
calcaneum)
- Deep boring pain, worse at night, relieved by rest
- Metaphyseal lesion cause no / little periosteal
reaction
- Diaphyseal lesion may be associated with
periosteal new bone formation and marked cortical
thickening
A circumscribed, oval cavity
surrounded by a zone of
sclerosis at the proximal
tibia (Brodies abscess)
This is a lateral view X-ray of left
tibia and fibula. There is a marked
periosteal reaction at the
diaphysis (Type IIb subacute OM)
Brodies abscess, central oval lucency surrounded
By reactive sclerosis usually within or close to the
Metaphysis and the lesion may extend across the
physis.
Treatment
Conservative (if the diagnosis is not in doubt)
a) Immobilization
b) Antibiotics (flucloxacillin + fusidic acid) for 6weeks
Surgical (if the diagnosis is in doubt / failed conservative
treatment)
a) Open biopsy
b) Perform curettage on the lesion
Chronic
osteomyelitis
Introduction
Definition:
A severe,persistent and incapacitating infection of
bone and bone marrow
Causes
- It can be due to:
progression / sequel / inadequate treatment of acute
osteomyelitis
open fracture
foreign implant (internal fixation)
Spread of pyogenic infections from neighbouring tissues
Punctured wounds
Complications of surgical procedures
Aetiological Agents
Usual organisms (with time there is always a mixed
infection)
Staph.aureus(commonest)
Staph.pyogenes
E.coli
Pseudomonas
Staph.epidermidis
(commonest in surgical implant)
Clinical Findings
Fever, malaise, bone pain
Local tenderness / temperature
Sinus- discharge
Puckering /Granulation at mouth of sinus
Bony thickening- localised /length of
diaphysis
Bony surface irregular
Wasting of muscles
Pathological fractures
Pathogenesis
Inadequate treatment of acute OM /
Foreign implant /
Open fracture
Inflammatory process continues with time
together with persistent infection by Staphylococcus aureus
Persistent infection in the bone leads to increase
in intramedullary pressure due to inflammatory exudates (pus)
stripping the periosteum
Vascular thrombosis
Bone necrosis (Sequestrum formation)
New bone formation occur (Involucrum)
Multiple openings appear in this involucrum, through which exudates & debris
from the sequestrum pass via the sinuses
(Sinus formation)
Pathological Features
Hallmark is bone necrosis
Exudation of PMNL, large no. of lymphocytes,
histiocytes and plasma cells( occasionally )
Formation of new bone (involucrum) from surviving
periosteum & endosteum
Involucrum- enveloping sheet of live bone with
perforations (cloacae) for pus to drain to the exterior
causing chronic sinus
Proliferation of endosteal new bone causing
obliteration of medullary canal
Prostaglandin E production is increased many folds in
infected bone causing bone resorption &
sequestration formation
Resorption is mediated by several cytokines IL-1, IL-
6, IL-11 & TNF
Why Chronicity ?
Negative charge on surface of devitalized bone
promotes organism adherence and subsequent
glycocalyx formation thereby preventing access to
phagocytes & microbials.
Bacteria enter the interior of the cell eluding host
defense. Dead & dying osteoblast release viable S.
Aureus causing persistence of infection & its flare up.
Pathology:
Features:
Dead piece of bone
Pale
Inner smooth ,outer rough
Surrounded by infected granulation tissue
trying to eat it
Types-
ring(external fixator)
tubular/match-stick(sickle)
coke and rice grain(TB)
Feathery(syphilis)
Colored(fungal)
Annular(amputation stumps)
Labs
Leukocyte count- in acute OM, often normal in chronic
cases (elevated in only 35%)
ESR in both
CRP - in acute/chronic, faster than ESR, more sensitive.
Favorable outcome if CRP decreases within 3 days of
antibiotic treatment.
Nutritional status
S. albumin level
Total iron binding capacity
Blood culture- yield approx. 60%
PCR
Culture & sensitivity- discharge/sinus
Deep bone biopsy- yield approx. 90%
Stage Characteristic Features
I Medullary Endosteal disease
II Superficial Cortical surface infected because of coverage
defect
III Localised Cortical sequestrum that can be excised without
compromising stability
IV Diffuse I, II and III plus mechanical instability before or
after debridement.
Anatomical Type
Cierney and Mader staging system of
Chronic Osteomyelitis
The Cierny-Mader Classification
1: Medullary Osteomyelitis -
Infection confined to medullary
cavity.
2: Superficial Osteomyelitis -
Contiguous type of infection.
Confined to surface of bone.
3: Localized Osteomyelitis -
Full-thickness cortical
sequestration which can easily be
removed surgically.
4: Diffuse Osteomyelitis -Loss of
bone stability, even after surgical
debridement.
93
Class Hosts immune
system
Features
A host Normal Immunocompetent with good local vascularity
B host Compromised Local or systemic factors that compromise
immunity or healing
C host Prohibitive Minimal disability, prohibitive morbidity
anticipated, poor prognosis for cure, treatment
worse than disease
Physiological class
Imaging
1) X-ray examination
2) Radioisotope scintigraphy
- Sensitive but not specific
- Technetium labelled hydroxymethylene diphosphonate (99mTc-
HDP) may show increased activity in both perfusion phase and
bone phase
3) CT scan & MRI
- Show the extent of bone destruction, reactive oedema, hidden
abscess and sequestra
Imaging
X-ray
Usually show bone resorption (patchy loss of density
/ osteolytic lesion)
Thickening & sclerosis around the bone
Occasionaly it may present as a Brodies abscess
surrounded by vascular tissue and area of sclerosis
Sequestrum
Involucrum
Cloacae
Irregular bone thickening
Pathological fracture
AP & lateral view of the left wrist show a lobulated osteolytic lesion with
well-defined borders and surrounding sclerosis at the distal radius.
Minimal expansion, mild periosteal reaction and soft tissue swelling are
present.
Sclerosing osteomyelitis of the
lower tibia. Note the bone
expansion and marked
sclerosis.
Sequestrum at lower tibia
.
sequestrum with normal structural
involucrum of a proximal humerus.
SINOGRAPHY
CT Scan
To identify areas of necrotic bone/ sequestra
Help in establishing a surgical plan
MRI
High sensitivity & specificity for diagnosis
Localises abnormal bone marrow early
Can detect myositis, cellulitis, sinus tract formation &
soft tissue abscess
Rim sign-in chronic OM is high signal intensity
surrounding the focus of active disease
Radionuclide scan
Used when diagnosis is ambiguous
Gauges extent of bone & soft tissue inflammation
-99mTc
- 67 Gallium citrate
- 111 Indium labelled leukocytes-ideally for acute OM.
MRI-is much more sensitive than nuclear studies .
During the 1
st
post-op year MRI can not accurately distinguish
infection from fibrovascular scarCOMBINED NUCLEAR
MEDICINE STUDIES WERE FOUND TO BE MORE USEFUL
DURING THIS PERIOD
18
FDG PET Scan
Meta-analysis showed Fluorodeoxyglucose positron
emission tomography has the highest accuracy for
confirming or excluding the diagnosis of Chr OM
The Accuracy of Diagnostic Imaging for the Assessment of
ChronicOsteomyelitis: A Systematic Review and Meta-Analysis
The Journal of Bone and Joint Surgery (American). 2005;87:2464-
2471.
Radiologic Classification of Chronic
Hematogenous
Osteomyelitis in Children
Henry Wynn Jones, FRCS (T&O), James W. Harrison, FRCS (T&O),
Jeremy Bates, FCS (ECSA), Gwyn A. Evans, FRCS, and Nicolas Lubega, FCS
(ECSA)
J Pediatr Orthop Volume 29, Number 7, October/November 2009
Chronic Hematogenous Osteomyelitis in Children
Classification
Type ABrodies abscess,
Type BSequestrum involucrum,
B1-Localised cortical sequestrum
B2-Sequestrum with normal /structural involucrum*
B3-Sequestrum with sclerotic involucrum
B4-Sequestrum without structural involucrum
Type Csclerotic.
If proximal physis is damaged the suffix P is added If distal
physis is affected the suffix D is added
Peltola and vahvanens criteria
-Pus on aspiration
-Positive bacterial culture from bone or blood
-Presence of classic signs and symptoms of acute osteomyelitis
-Radiographic changes typical of osteomyelitis
*--Two of the listed findings must be present for establishment of the
diagnosis.
Peltola H, Vahvanen V (1984) A comparative study of osteomyelitis and purulent arthritis with special reference
to aetiology and recovery. Infection 12:7579
Treatment
Patient evaluation
(History taking, PE, Investigation)
Disease assessment
(Anatomic & Physiologic classification)
Identification of organism
(Biopsy + Culture)
Antibiotic administration
Surgical treatment
(Debridement, Deep space management)
Follow up
TREATMENT
MEDICAL
Specific antimicrobial coverage
In compromised hostcorrect or reduce the host
defect
SURGICAL
Adequate drainage
Debridement
Obliteration of dead space
Adequate soft tissue cover for wound protection
Restoration of an effective blood supply
Antibiotics
- Chronic infection is seldom eradicated by antibiotics
alone
- Bactericidal drugs are important to:
a) Stop the spread of infection to healthy bone
b) Control acute flares
- The choice of antibiotic used must be:
a) Capable of penetrating sclerotic bone
b) Non toxic with long term use
ANTIBIOTICS
IV antibiotics
Nafcillin/oxacillin/nafcillin with rifampcin *
Vancomycin/ampicillin/cefazolin/ceftriaxone
Clindamycin/sulbactum/piperacillin/tazobactam
ORAL antibiotics
Clindamycin/rifampcin/cotrimexazole
Fluroquinolones in gram ve organisms
Linezolid-oral & IV antibioticsMRSA
2) Surgical Treatment
- After 10 days of antibiotic administration,
debridement is
done to remove:
a) All the infected tissue
b) Dead / devitalised bone (Sequestrectomy)
c) Sinus tract
- Debridement approach used is direct & atraumatic
Bone Debridement:
The goal of debridement is to leave healthy, viable tissue.
Dbridement of bone is done until punctate bleeding is noted, giving
rise to the term the paprika sign.
Copious irrigation with 10 to 14 L of normal saline.
Pulsatile lavage using fluid pressures 50-70 pounds per square inch
and 800 pulses per min.
The extent of resection is important in B hosts as B hosts treated
with marginal resection (i.e., with a clearance margin of <5 mm) found
to have a higher rate of recurrence than normal hosts.
A
Repeated debridements may be required.
A.Simpson AH, Deakin M, Latham JM. Chronic osteomyelitis. The effect of
the extent of surgical resection on infection-free survival. J Bone Joint Surg
Br. 2001;83:403-7.
Sequestrectomy and curettage. A, Affected bone is exposed, and sequestrum is
removed. B, All infected matter is removed. C, Wound is either packed open or closed
loosely over drains.
In either case it is critical to preserve the
involucrum
preferable to wait at least 3-6 mo before performing a
sequestrectomy
Early sequestrectomy
- Eradicate infection
- Better environment for
periosteum to respond
Delayed sequestrectomy
Wait till sufficient involucrum
has formed before doing a
sequestrectomy to mimimize
the risk of cx, fracture,
deformity & segmental loss
When to do sequestrectomy?
Prerequisites for
Sequestrectomy
Radiological
Well formed
involucrum
surrounding the
discretely visible
sequestrum
adequately at least
2/3
rd
diameter of bone
(3 intact walls on two
views ensure 3/4
th
intact walls)
Clinical
Symptomatic patient
with pus discharge or
chronic unreleaved
disabling pain due to
osteomyelitis per se
and type A/B host.
SEQUESTRUM
Post sequestrectomy
NO STABLISATION IS NECESSARY WHEN 70% OF
THE ORIGINAL CORTEX REMAINS INTACT
If >70% cortical volume has been retainedprotect
by cast
Greater bone loss-Ext fix
Focal bone loss-open cancellous BG/conventional
BG
Seg. bone lossBG/Bone transport/other devices
Saucerization
Extension of surgical
debridement
Debrided wounds left open
widely through excision of
overhanging soft tissue and bone
Wounds drain freely
Abscesses do not form
Limited to areas where it causes
acceptable loss of function e.g.
Tibia and femur
May require stabilization
- After debridement is done, a large dead space is left in
the bone
- Among the methods of managing dead space:
a) Open cancellous grafting (Papineau technique)
b) Primary closure with local tissue (+/- cancellous
grafts)
c) Primary closure with transferred tissues (+/-
cancellous grafts)
d) Primary closure over antibiotic impregnated beads
Four basic methods of immediate, biological management of dead space using living
tissue or cancellous bone grafts.
Management of Dead Space:
Antibiotic Beads
May be used to sterilize and temporarily maintain
a dead space.
Beads are made with PMMA+ab
Cement -40 gm.
Genta- 1-2 gm. or vanco 1-2 gm.
Other antibiotics that can be used are
Tobramycin, Penicillin, cephalosporins, amikacin,
vancomycin.
Usually removed within two to four weeks and are
replaced with a cancellous bone graft.
a. Patzakis MJ, Mazur K, Wilkins J, et al. Septopal beads and autogenous bone grafting for bone defects in patients with
chronic osteomyelitis. Clinical Orthopaedics and Related Research 1993, 295: 1128.
Management
Cierny-Mader stage 1,3,4 require 4 - 6 wks of antibiotics
(revascularisation of bone after debridement takes about 4
wks)
Stage 2short course antibiotics for 2 wks following
debridement of cortex/soft tissue
Stage 3 /4 antibiotics for 4 to 6 wks from last major
decompression/debridement
Culture Blood bone
Initial antibiotic
selection
Change or confirm d/o culture results
Poor
response
Operative treatment
unroofing ,abscess
drainage, IM reaming
4 wks
antibiotics
Failure
Retreat
as
above
Arrest
Good
response
Continue 2 wks
parenteral & 4 wks
Oral antibiotics
Treatment algorithm
of Cierny-Mader
Stage-1, or
hematogenous,
long-bone
osteomyelitis.
Hardware removal
Bone stable
Hardware removal
IM reaming
Antibiotics
Continue 2 wks parenteral
& 4 wks Oral
Failure
Retreat as
above
Arrest
Bone
unstable
Suppressive antibiotic
treatment until
stabilisation
Treatment algorithm of
Cierny-Mader Stage-1 long-
bone osteomyelitis
associated with infection
at the site of hardware
Superficial
debridement
Biopsy &
culture
Initial antibiotic
selection
Change or confirm based on culture
results
Continue antibiotics for 2
wks
Local or
microvascular coverage
Treatment
algorithm of
Cierny-Mader
Stage-2 long-
bone
osteomyelitis
Biopsy &
Culture
Initial antibiotic
selection
Change or confirm d/o
culture results
6wks antibiotics
after major
operative
debridement
Failure
Retreat
as above
Arrest
Debridement
Hardware
removal
Dead space
management, beads,
bone grafts, & muscle
flaps
Stabilisation
external fixation
Ilizarov
technique
Soft tissue coverage
Treatment
algorithm of
Cierny-Mader
Stages-3 and 4
long-bone
osteomyelitis.
Osteomyelitis in long bones, L . Lazzarini,J.T.Mader,JBJS.Am.2004;86:2305-318
Chronic multifocal osteomyelitis
In the 1970s it was noted that a number of children
presented with a low-grade form of bone disease that
behaved clinically like an acute osteomyelitis.
Typically it affected the long bones and went on to a
sclerotic reaction.
The first episode would settle and some months or even a
few years later there would be recurrence at another site.
No organisms are grown and the course of the disease
becomes chronic and relapsing.
The clinical importance is to avoid repeated biopsy
once the relapsing nature of the condition has been
recognized.
Plain radiographs are essential to recognize the bone
infection.
Skeletal scintigraphy is a good method of screening for
other lesions
whilst MRI is the best means of judging extent and
activity
Chronic recurrent multifocal osteomyelitis (CRMO)
. Diagnostic criteria for CRMO have been
proposed to include all of the following:
(a) the presence of two or more radiographically
confirmed bone lesions,
(b) a prolonged course of at least 6 months with
characteristic exacerbation and remission,
(c) radiographic and nuclear scintigraphic evidence of
osteomyelitis,
(d) a lack of response to antimicrobial therapy of at
least 1 months duration, and
(e) the lack of an identifiable etiology .
A definitive role for steroids or long term antibiotics has
not been established. Supportive management with
anti-inflammatory medication is recommended, as the
typical course of CRMO is self-limited.
Sclerosing osteomyelitis of Garr
A rare type of osteomyelitis
Occuring in children and young adults
Presents with insidious onset of pain, pyrexia and
swelling.
Symptoms recur at intervals for several years and
subside gradually . .
Radiological appearance is of intense sclerosis
resulting in thickned bone.
There is predilection for involvement of mandible and
shaft of long bones.
There is no discharging sinus
No necrosis
No purulent exudate
Little granulation tissue
Garr sclerosing osteomyelitis, or chronic nonsuppurative sclerosing osteomyelitis,
is a form of chronic osteomyelitis. Mild inflammation and infection lead to
subperiosteal bone deposition. It is frequently asymptomatic. The characteristic
radiographic appearance is an area of periosteal proliferation surrounded by
successive layers of condensed cortical bone (arrows), described as an onion skin
appearance.
Tuberculosis
Tuberculous bone infection occurs secondarily as a
result of hematogenous spread from a primary source
such as lung or genitourinary tract.
Bone infection is most typically slow growing and
indolent. Tuberculous caries is seen where the margin
of the bone is scalloped and eaten away. Large cold
abscesses occur. This means that the patient is
surprisingly well given the size of the collection
Little or no surrounding reactive bone with presence of
osteopenia
Affects epiphysis, metaphysis and diaphysis.
Eccentric area of osteolysis is seen in metaphysic
Transepiphyseal spread of lytic lesion
No sequestrum formation is seen.
Occasionally, destruction in the mid diaphysis of a
short tubular bone of the hand or foot(tuberculous
dactylitis) may produce a fusiform enlargement of the
entire diaphysis is called as spina vetosa.
Lytic lesion with soft tissue
swelling
No sclerosis or periosteal
new bone formation
Fungal osteomyelitis
A variety of fungi may affect bones and joints
slowly developing and difficult to eradicate;
Low grade with abcess and draining sinuses
they may mimic tumours.
little or no reactive sclerosis or periosteal response
Seen more often in immunosuppressed patients.
Fungi should be considered when the bacteriological
findings do not fit the clinical presentation.
Radiography
well-marginated, punched-out osteolytic lesions.
Unilocular, but occasionally multiloculated.
permeative type of bone destruction.
joint involvement (septic arthritis)
Soft-tissue swelling and osteoporosis
CRYPTOCOCCOSIS
Destructive lesion , minimal sclerosis and no periosteal reaction
coccidiodomycosis
Syphilis
Skeletal presentations are varied and mimic many
other diseases
Congenital syphilis may cause a symmetric periostitis
with lamination.
Congenital syphilis - chronic osteochondritis,
periostitis, or osteitis.
Granulomas occurring in the metaphyses of long
bones produce lytic areas known as Wimberger's sign
The growth plate may be abnormal with lytic bands in
the adjacent bone
saber-shin deformity of tibia
1) Acute exacerbations
2) Pathological Fracture
- This occurs in the bone weakened by chronic
osteomyelitis
3) Deformity
In children the focus of osteomyelitis destroys
part of the epiphysis growth plate.
4) Shortening/ lengthening
- Destruction of growth plate arrest growth.
- Stimulation of growth plate due to hyperemia.
5) Amyloidosis
Complications
S-ar putea să vă placă și
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- OsteomyelitisDocument35 paginiOsteomyelitischinnnababu100% (1)
- Osteomyelitis: Mariamawit B Dbu, College of MedicineDocument34 paginiOsteomyelitis: Mariamawit B Dbu, College of MedicinedenekeÎncă nu există evaluări
- SPRAINS and StrainsDocument26 paginiSPRAINS and StrainsRaquid MariaÎncă nu există evaluări
- Acute and Chronic Osteomyelitis-1Document63 paginiAcute and Chronic Osteomyelitis-1Cati Moraru100% (1)
- Amputation: DefinitionDocument9 paginiAmputation: DefinitionCharaÎncă nu există evaluări
- Fracture of Tibia and FibulaDocument31 paginiFracture of Tibia and Fibulaunknown unknown100% (1)
- Lecture Contents: Definitions Composition of Hernia Managment of HerniaDocument26 paginiLecture Contents: Definitions Composition of Hernia Managment of Herniaissam_1994Încă nu există evaluări
- Intestinal ObstructionDocument58 paginiIntestinal ObstructionTUSHAR PARMARÎncă nu există evaluări
- OsteomyelitisDocument3 paginiOsteomyelitisIanne Merh100% (1)
- Classification of FracturesDocument26 paginiClassification of FracturesHoney May Rollan VicenteÎncă nu există evaluări
- Complications of FracturesDocument68 paginiComplications of FracturesChenna Kesava100% (1)
- Supracondylar Humerus FractureDocument20 paginiSupracondylar Humerus FractureMusyawarah MelalaÎncă nu există evaluări
- Buerger's DiseaseDocument8 paginiBuerger's DiseaseGayle Bautista100% (1)
- Peptic Ulcers: DR Yotham Phiri Mmed (Surg)Document46 paginiPeptic Ulcers: DR Yotham Phiri Mmed (Surg)Emmanuel MukukaÎncă nu există evaluări
- Case Report (Ola)Document44 paginiCase Report (Ola)amel015Încă nu există evaluări
- Treatment and Management of Rheumatoid ArthritisDocument32 paginiTreatment and Management of Rheumatoid ArthritisamirthaÎncă nu există evaluări
- Rheumatoid ArthritisDocument19 paginiRheumatoid ArthritisKim GonzalesÎncă nu există evaluări
- Truncus ArteriosusDocument4 paginiTruncus ArteriosuskemalahmadÎncă nu există evaluări
- Legg-Calvé-Perthes Disease - An Overview With Recent LiteratureDocument10 paginiLegg-Calvé-Perthes Disease - An Overview With Recent LiteratureFranz BlacuttÎncă nu există evaluări
- Proximal Femur FracturesDocument34 paginiProximal Femur FracturesPrashant Madan MohanÎncă nu există evaluări
- Perthes Disease: by Dr. Abdul Karim Postgraduate Resident Orthopedic Surgery Pgmi/Lgh. Lahore PakistanDocument68 paginiPerthes Disease: by Dr. Abdul Karim Postgraduate Resident Orthopedic Surgery Pgmi/Lgh. Lahore Pakistandrakkashmiri50% (2)
- Tuberculosis of SpineDocument11 paginiTuberculosis of SpineSepti RahadianÎncă nu există evaluări
- Hemorrhoid MedscapeDocument10 paginiHemorrhoid MedscapeRastho Mahotama100% (1)
- Pyothorax / Purulent Pleuritis / Empyema Thoracis: Prepared By: Sharmin SusiwalaDocument22 paginiPyothorax / Purulent Pleuritis / Empyema Thoracis: Prepared By: Sharmin SusiwalaAnkan Dey100% (1)
- MeningoceleDocument33 paginiMeningoceleAnkira Findoro100% (1)
- CellulitisDocument15 paginiCellulitisSujatha J JayabalÎncă nu există evaluări
- Amputation: by Ashenafi Zemed MSC PTDocument25 paginiAmputation: by Ashenafi Zemed MSC PTHęñøķ BęŕhãñęÎncă nu există evaluări
- Fractures: Mary Grace B. Gutierrez Resti Mariano Ma. Cindy O. BautistaDocument50 paginiFractures: Mary Grace B. Gutierrez Resti Mariano Ma. Cindy O. BautistaJustin Ahorro-DionisioÎncă nu există evaluări
- Inguinal Hernias: CaseDocument6 paginiInguinal Hernias: Casechomz14Încă nu există evaluări
- Indirani College of Nursing: AmputationDocument7 paginiIndirani College of Nursing: AmputationdhanasundariÎncă nu există evaluări
- Balance Skeletal Traction1Document31 paginiBalance Skeletal Traction1Maria Victoria ColomaÎncă nu există evaluări
- TRACTION LavlyDocument9 paginiTRACTION Lavlylabsky_evol100% (1)
- HirschprungDocument13 paginiHirschprungfitra hayatiÎncă nu există evaluări
- DDH - PFDocument34 paginiDDH - PFAnnisa Oktoviani MursidaÎncă nu există evaluări
- Osteomyelitis: Dr. Amit Gupta Reader Department of Oral PathologyDocument77 paginiOsteomyelitis: Dr. Amit Gupta Reader Department of Oral PathologyAMIT GUPTAÎncă nu există evaluări
- Osteomyelitis PresentationDocument15 paginiOsteomyelitis PresentationFrancis_Legasp_3667Încă nu există evaluări
- Osteoarthritis: T Person's of Developing Osteoarthritis. It IncludesDocument5 paginiOsteoarthritis: T Person's of Developing Osteoarthritis. It IncludesLove Shery SabrosoÎncă nu există evaluări
- Management Head Injury in ICUDocument5 paginiManagement Head Injury in ICUIrma KusumaÎncă nu există evaluări
- Hip FracturesDocument7 paginiHip FracturesDinly JoyÎncă nu există evaluări
- Pes PlanusDocument6 paginiPes PlanusdeffyÎncă nu există evaluări
- Leg UlcersDocument22 paginiLeg UlcersMarera DomnicÎncă nu există evaluări
- Inguinal Hernias and Abdominal Wall Defects: Murad Nuserat & Abd AL-Rahman AlhelwDocument51 paginiInguinal Hernias and Abdominal Wall Defects: Murad Nuserat & Abd AL-Rahman AlhelwRashed ShatnawiÎncă nu există evaluări
- Fracture in Leg Tibia and FibulaDocument27 paginiFracture in Leg Tibia and Fibulachilsya shajiÎncă nu există evaluări
- Club Foot-Dr J SahooDocument9 paginiClub Foot-Dr J SahooSheel Gupta100% (1)
- Compartment Syndrome AndreDocument40 paginiCompartment Syndrome AndreOlivia Christy KaihatuÎncă nu există evaluări
- 08 Bone TumorsDocument94 pagini08 Bone TumorsSara FoudaÎncă nu există evaluări
- 1 PeritonitisDocument26 pagini1 PeritonitisGizachew AsimareÎncă nu există evaluări
- Aetiology and Management 0f Septic ArthritisDocument62 paginiAetiology and Management 0f Septic ArthritisSamÎncă nu există evaluări
- Osteoporosis: Hani Abu DiehDocument24 paginiOsteoporosis: Hani Abu DiehAngelic khan100% (1)
- Umbilical Hernia - Wikipedia PDFDocument31 paginiUmbilical Hernia - Wikipedia PDFNeelamÎncă nu există evaluări
- Crush Injuries: Prepared By: Lynette J. CaldoDocument17 paginiCrush Injuries: Prepared By: Lynette J. CaldoLynette JavaÎncă nu există evaluări
- Knee MechanicsDocument107 paginiKnee MechanicsAhmed El goharyÎncă nu există evaluări
- Stages of Fracture HealingDocument5 paginiStages of Fracture HealingNnaa LlppÎncă nu există evaluări
- OSTEOMYELITISDocument4 paginiOSTEOMYELITISapi-3822433Încă nu există evaluări
- Osteogenesis ImperfectaDocument25 paginiOsteogenesis ImperfectaNavya Sruthi MandapatiÎncă nu există evaluări
- HerniaDocument11 paginiHerniaHapsari Wibawani 'winda'100% (1)
- WoundDocument5 paginiWoundMd Ahsanuzzaman PinkuÎncă nu există evaluări
- Musculoskeletal Disorders: Prepared By: John Gil B. Ricafort, RNDocument55 paginiMusculoskeletal Disorders: Prepared By: John Gil B. Ricafort, RNPaola AgustinÎncă nu există evaluări
- RRL Anne)Document27 paginiRRL Anne)api-3728522Încă nu există evaluări
- Classification and Patient Selection in Abdominoplasty: Alan Matarasso, MD, FacsDocument8 paginiClassification and Patient Selection in Abdominoplasty: Alan Matarasso, MD, FacsPopa FlorinÎncă nu există evaluări
- Schizo QuizDocument4 paginiSchizo QuizmalindaÎncă nu există evaluări
- Accuveinav400 For Vein Visualisation PDF 1763868852421Document24 paginiAccuveinav400 For Vein Visualisation PDF 1763868852421Mohannad HamdÎncă nu există evaluări
- New Microsoft Office Word DocumentDocument14 paginiNew Microsoft Office Word DocumentMohamed RashadÎncă nu există evaluări
- What Is BronchitisDocument1 paginăWhat Is BronchitisMelvin Lopez SilvestreÎncă nu există evaluări
- Meuhedet Adif RegulationsDocument72 paginiMeuhedet Adif RegulationsEnglishAccessibilityÎncă nu există evaluări
- Anemia PPT 3 Nov 2014Document60 paginiAnemia PPT 3 Nov 2014Susi DesmaryaniÎncă nu există evaluări
- Autocoid PharmacologyDocument29 paginiAutocoid PharmacologyLyadelou Fortu100% (1)
- Cold ApplicationDocument2 paginiCold ApplicationNazire Luis Colita YandugÎncă nu există evaluări
- The Arthritis Step by Step Strategy PDF EBook DownloadDocument7 paginiThe Arthritis Step by Step Strategy PDF EBook Downloadowenmathias880% (2)
- Family Nursing Care Plan SeizuresDocument3 paginiFamily Nursing Care Plan SeizuresClaire AlcantaraÎncă nu există evaluări
- Drugs That Affect The Digestive SystemDocument17 paginiDrugs That Affect The Digestive SystemMusa MuhamadÎncă nu există evaluări
- Not Yet Done!Document9 paginiNot Yet Done!Erickamae GregorioÎncă nu există evaluări
- Pontalis, J. B. (2014) - No, Twice NoDocument19 paginiPontalis, J. B. (2014) - No, Twice NocabaretdadaÎncă nu există evaluări
- AbDocument5 paginiAbapi-466413302Încă nu există evaluări
- Pelvic Inflammatory DiseaseDocument34 paginiPelvic Inflammatory DiseaseOhunakin AfolabiÎncă nu există evaluări
- Handbook: For Clinical Management of DengueDocument124 paginiHandbook: For Clinical Management of DengueraattaiÎncă nu există evaluări
- MHFW OrderDocument4 paginiMHFW OrderNavjivan IndiaÎncă nu există evaluări
- SWS Bibliography1Document3 paginiSWS Bibliography1Valaki MimiÎncă nu există evaluări
- Presented By: Bhagyashree KaleDocument58 paginiPresented By: Bhagyashree KaleSupriya JajnurkarÎncă nu există evaluări
- Drug Free Australia's Dr. Stuart Reece & Culpable Abuse of PatientsDocument6 paginiDrug Free Australia's Dr. Stuart Reece & Culpable Abuse of PatientsPaul GallagherÎncă nu există evaluări
- ASCCP Management Guidelines - August 2014 PDFDocument24 paginiASCCP Management Guidelines - August 2014 PDFAnita BlazevskaÎncă nu există evaluări
- Herbal GuideDocument42 paginiHerbal GuideladygreenÎncă nu există evaluări
- Case Study 2Document6 paginiCase Study 2Gertie Mae CuicoÎncă nu există evaluări
- Vriddhi KshayaDocument37 paginiVriddhi KshayaVenkatesan VidhyaÎncă nu există evaluări
- Author's Overall Organizational PatternDocument6 paginiAuthor's Overall Organizational PatternTashieka GrahamÎncă nu există evaluări
- Antiaritmice Clasa I A MedicamentDocument3 paginiAntiaritmice Clasa I A MedicamentAndreea ElenaÎncă nu există evaluări
- SNR Englisch-3Document6 paginiSNR Englisch-3Geoff WhiteÎncă nu există evaluări
- Manual C28 Plus enDocument28 paginiManual C28 Plus enSveto SlÎncă nu există evaluări
- The Bodies of Others: The New Authoritarians, COVID-19 and The War Against the HumanDe la EverandThe Bodies of Others: The New Authoritarians, COVID-19 and The War Against the HumanEvaluare: 4.5 din 5 stele4.5/5 (12)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisDe la EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisEvaluare: 4 din 5 stele4/5 (9)
- Do You Believe in Magic?: The Sense and Nonsense of Alternative MedicineDe la EverandDo You Believe in Magic?: The Sense and Nonsense of Alternative MedicineÎncă nu există evaluări
- Deaths of Despair and the Future of CapitalismDe la EverandDeaths of Despair and the Future of CapitalismEvaluare: 4.5 din 5 stele4.5/5 (30)
- Uncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicDe la EverandUncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicÎncă nu există evaluări
- Mama Might Be Better Off Dead: The Failure of Health Care in Urban AmericaDe la EverandMama Might Be Better Off Dead: The Failure of Health Care in Urban AmericaÎncă nu există evaluări
- Epic Measures: One Doctor. Seven Billion Patients.De la EverandEpic Measures: One Doctor. Seven Billion Patients.Evaluare: 4 din 5 stele4/5 (13)
- There Are No Accidents: The Deadly Rise of Injury and Disaster—Who Profits and Who Pays the PriceDe la EverandThere Are No Accidents: The Deadly Rise of Injury and Disaster—Who Profits and Who Pays the PriceEvaluare: 4.5 din 5 stele4.5/5 (11)
- The Wisdom of Plagues: Lessons from 25 Years of Covering PandemicsDe la EverandThe Wisdom of Plagues: Lessons from 25 Years of Covering PandemicsEvaluare: 4.5 din 5 stele4.5/5 (6)
- The Varicose Veins Mastery Bible: Your Blueprint for Complete Varicose Veins ManagementDe la EverandThe Varicose Veins Mastery Bible: Your Blueprint for Complete Varicose Veins ManagementÎncă nu există evaluări
- The Nocebo Effect: When Words Make You SickDe la EverandThe Nocebo Effect: When Words Make You SickÎncă nu există evaluări
- Clean: Overcoming Addiction and Ending America’s Greatest TragedyDe la EverandClean: Overcoming Addiction and Ending America’s Greatest TragedyEvaluare: 4 din 5 stele4/5 (18)
- There Are No Accidents: The Deadly Rise of Injury and Disaster—Who Profits and Who Pays the PriceDe la EverandThere Are No Accidents: The Deadly Rise of Injury and Disaster—Who Profits and Who Pays the PriceEvaluare: 4.5 din 5 stele4.5/5 (15)
- The Price of Health: The Modern Pharmaceutical Industry and the Betrayal of a History of CareDe la EverandThe Price of Health: The Modern Pharmaceutical Industry and the Betrayal of a History of CareEvaluare: 4.5 din 5 stele4.5/5 (3)
- The Invisible Rainbow: A History of Electricity and LifeDe la EverandThe Invisible Rainbow: A History of Electricity and LifeEvaluare: 4.5 din 5 stele4.5/5 (21)
- Heat Wave: A Social Autopsy of Disaster in ChicagoDe la EverandHeat Wave: A Social Autopsy of Disaster in ChicagoEvaluare: 4 din 5 stele4/5 (40)
- The Atlas of Disease: Mapping Deadly Epidemics and Contagion from the Plague to the CoronavirusDe la EverandThe Atlas of Disease: Mapping Deadly Epidemics and Contagion from the Plague to the CoronavirusEvaluare: 4.5 din 5 stele4.5/5 (10)
- The Hair Color Mix Book: More Than 150 Recipes for Salon-Perfect Color at HomeDe la EverandThe Hair Color Mix Book: More Than 150 Recipes for Salon-Perfect Color at HomeEvaluare: 3.5 din 5 stele3.5/5 (7)
- The Wuhan Cover-Up: And the Terrifying Bioweapons Arms RaceDe la EverandThe Wuhan Cover-Up: And the Terrifying Bioweapons Arms RaceÎncă nu există evaluări
- Coronary: A True Story of Medicine Gone AwryDe la EverandCoronary: A True Story of Medicine Gone AwryEvaluare: 5 din 5 stele5/5 (4)
- Fatal Conveniences: The Toxic Products and Harmful Habits That Are Making You Sick—and the Simple Changes That Will Save Your HealthDe la EverandFatal Conveniences: The Toxic Products and Harmful Habits That Are Making You Sick—and the Simple Changes That Will Save Your HealthEvaluare: 4 din 5 stele4/5 (7)
- Inflamed: Deep Medicine and the Anatomy of InjusticeDe la EverandInflamed: Deep Medicine and the Anatomy of InjusticeEvaluare: 5 din 5 stele5/5 (12)
- Beyond the Next Village: A Year of Magic and Medicine in NepalDe la EverandBeyond the Next Village: A Year of Magic and Medicine in NepalÎncă nu există evaluări
- COVID-19: The Victims, The Heroes, The Comlicit, and Our New NormalDe la EverandCOVID-19: The Victims, The Heroes, The Comlicit, and Our New NormalÎncă nu există evaluări
- Mercury, Mining, and Empire: The Human and Ecological Cost of Colonial Silver Mining in the AndesDe la EverandMercury, Mining, and Empire: The Human and Ecological Cost of Colonial Silver Mining in the AndesÎncă nu există evaluări
- Healthy Buildings: How Indoor Spaces Drive Performance and ProductivityDe la EverandHealthy Buildings: How Indoor Spaces Drive Performance and ProductivityEvaluare: 5 din 5 stele5/5 (2)