Documente Academic
Documente Profesional
Documente Cultură
Drug Interactions
Încărcat de
Tiven StiveDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Drug Interactions
Încărcat de
Tiven StiveDrepturi de autor:
Formate disponibile
1
DRUG INTERACTIONS
azalia arif fkui
2
Drug interactions occurs when :
The effects of one drug altered by the effetcs of
another drug
Drug that precipitate precipitant
Drug whose action affected object drug
Can result an increase or a decrease the effect
of the object drug
3
example :
amiodarone inhibits a cytochrome P
450
(CYP2C9) metabolisme of S(-) warfarin
and anticoagulant effect
carbamazepine anticoagulant effect of S(-)
warfarin by increasing its hepatic metabolism
cytochrome P
450
occasionally in an interaction the effects of both
drug are altered i.e the complex interaction of
phenytoin with phenobarbital
4
Although drug interaction usually result in an
adverse drug reaction; in some cases an
interaction is beneficial i.e :
The pharmacodynamic synergy between
diuretics and angiotensin-converting enzyme
(ACE) inhibitor in the treatment of hypertension
5
Incidence of significant drug interactions :
the more drugs a patient is taking the
greater the chance of an interaction
several factors that make patients
vulnerable to interactions :
- advance age
- multiple medications
- acute severe illness
- poor renal and hepatic functions
- more than one prescribing doctor
6
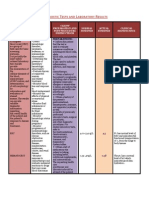
Drugs that are likely to precipitate drug
interactions
drugs that are highly protein bound likely
to displace object drugs from protein-binding
sites
drugs that alter (stimulate or inhibit) the
metabolism of other drug (see table)
drugs that affect renal function and alter the
renal clearance of object drugs i.e diuretics,
probenecid
7
drugs that are likely to be the object of drug
interactions :
those that have a steep dose-response curve
i.e drugs for which a small change in dose
results in a relatively large large change in
therapeutic effect causing reduced efficacy
of the object drug
drug that have a low toxic/therapeutic ratio
i.e ??
8
Pharmaceutical interactions
are physicochemical interactions :
a drug with IV infusion
two drugs in the same solution loss of
activity the drug involved
are too numerous to remember in detail
can be simply to be avoided by adhering the
following principles :
9
1. Give IV drugs by bolus injection or via an IV burrette
2. Do not add drugs to infusion solution other to
dextrose or saline, some drugs are unstable and
some are light sensitive (see table)
3. Avoid mixing drugs in the same infusion solution,
unless is known to be safe
4. Look for specific warning in manufactures literature
5. Mix the drug thoroughly in the infusion solution and
check regularly for visible changes (turbidity,
precipitation or color change)
10
6. Prepare solution only when needed
7. Label all infussion bottles clearly with the
name and dose of drug added, the time of
starting and ending the infusion
8. Use two separate infusion sitesif two drugs
must be infused simultaneously, unless you
are sure there is no interaction
9. Consult the local hospital pharmacist if in
doubt
11
Pharmacokinetic interactions
occur when the absorption, distribution,
metabolism and elimination of the object
drug is altered by the precipitant drug
Absorption interactions
the absorption of a drug can be reduced by
another drug in several ways :
12
The git absorption of drugs may be affected
by concurrent use of other agents that :
have a large surface area of absorption
bind or chelate
alter gastric pH
alter git motility
affect transport protein such as P-glycoprot.
reduction of absorption will be clinically
important if it results in subtherapeutic serum
levels
13
reduced git motility caused by morphine-
like drugs and drugs with anticholinergic
effects, such as tricyclic antidepresant
chelation of Ca, Al, Mg and iron salt by
tetracyclines
binding of warfarin and digitoxin by
cholestyramin
14
The mechanism by which drug interactions
alter drug distribution include :
competition of plasma binding protein
displacement from tissue binding site
alteration in local tissue barriers i.e
P- glycoprotein inhibition in the BBB
15
The metabolism of drugs can be stimulated or
inhibited by concurrent therapy
Induction (stimulation) of cytochrom P450
isoenzyme can be caused by drug such as :
barbiturate, carbamazepine, phenytoin,
rifampin and others (Katz. p1082)
Enzyme induction can also increase the
activity of phase II metabolism such as
glucuronidation
16
Enzyme induction usually occurs 7 10
days and requires equal/longer time to
disappear after the inducer stopped
Rifampin, may produce enzyme induction
after only a few doses
If the half-life of the affected drug is long, it
may take a week or more to reach the new
steady state concentration
17
Drugs that may inhibit cytochrome P450
metabolism of other include :
amiodarone, androgens, atazanavir,
chloramphenicol, cimetidine, ciprofloxacin and
others (Katz. p1082)
18
The renal excretion of active drug can also be
affected :
weak acid or weak bases may be influence
by other drugs that affect urinary pH due
to ionization of the drug
19
Pharmacodynamic interactions
precipitant drug alters the effect of the object
drug at its site of action direct or indirect
Direct pharmacodynamic interactions
occur when two drugs either act on the
same site (antagonism or synergism)
or act on two different sites with a similar
end result
20
Antagonism at the same site
many example, some of which are
therapeutically beneficial
i.e the reversal of the effectsof opiates
with naloxone and
the reversal action of warfarin by
vitamin K
21
Synergism at the same site
1. The effects of warfarin can be incresed or
decreased in direct synergistic interaction :
The pricise mech. of this interaction is not
clear could be :
a. changes in the affinity of warfarin for
vitamin K epoxide reductase (clofibrate,
D-thyroxine, & anabolic steroids)
22
b. alteration in the synthesis rate of clotting
factors ( anabolic steroids)
c. changes in the activity of clotting factors
(tetracyclines)
d. reduced availability of vitamin K secondary to
reduced plasma lipid conc. (d-thyroxine and
anabolic steroids)
23
2. The effects of depolarizing muscle relaxant
potentiated by some antibiotics ( colistin,
aminoglycosides and polymixin B) and by
quinine and quinidine due to the curare-
like effects on the motor end plate of skeletal
muscle
3. Verapamil and - adrenoceptor antagonist
higher frequency of cardiac arrythmia
This combination is also associated with an
increased risk of heart failure both have
negative inotropic effects on cardiac muscle
24
4. drugs that prolong QT interval
can cause ventricular arrhythmia, particularly
the form of polymorphous ventricular
tachycardia called torsade de pointes i.e
halofantrin and antiarrhythmia
25
Synergysm of similar effects at different sites
two CNS depressant will potentiate the effects
of each other, whether or not the two drugs act
on the same receptors : alcohol with CNS
depressant
beneficial : combination of cytotoxic drugs in
the treatment of malignancies
combination of antibiotic in the
treatment of infection
(tuberculosis)
26
Indirect pharmacodynamic interactions
Coagulation : warfarin and other anticoagulant
can be involved in indirect
interactions in 3 ways
1. Platelet aggregation these drugs reduced
the ability of platelet to aggregate ; salicylate,
dipyridamol, sunfinpyrazone, mefenemic acid,
phenylbutazone and other.
27
2. gastrointestinal ulceration
if a drug causes git ulceration it provides
bleeding in patient taking anticoagulant ( e.g
aspirin, phenylbutazone, indomethacin and
other AINS drug)
3. fibrinolysis enhance the effect or warfarin
28
Fluid and electrolyte balance
changes in electrolyte balance alter the
effect of some drug
- the effects of cardiac glycosides are
enhanced by potassium depletion digitalis
toxicity
- hypokalemia risk of arrhythmia in patient
taking antiarrhythmia that prolong QT
interval e.g quinidine, procaineamid,
encainid and flecainide)
29
- thiazide effect hypoglycemic sulfonylurea
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- ENN PHARMACOLOGY BUNDLE PrintDocument142 paginiENN PHARMACOLOGY BUNDLE Printronique reid83% (6)
- Lovenox (Enoxaparin)Document1 paginăLovenox (Enoxaparin)E100% (5)
- Hypertension CrisisDocument24 paginiHypertension CrisisTiven StiveÎncă nu există evaluări
- Mycoplasma SPPDocument12 paginiMycoplasma SPPTiven StiveÎncă nu există evaluări
- Atypical Mycobacteria: DG Dasar Epidemiologi, Mycobacteria Dibagi: 1. M. Tuberculosis Komplek - M. TuberculosisDocument19 paginiAtypical Mycobacteria: DG Dasar Epidemiologi, Mycobacteria Dibagi: 1. M. Tuberculosis Komplek - M. TuberculosisTiven StiveÎncă nu există evaluări
- Gastroenteritis PDFDocument5 paginiGastroenteritis PDFLikhna PertiwiÎncă nu există evaluări
- A1004 Drug DoseDocument32 paginiA1004 Drug DoseTiven StiveÎncă nu există evaluări
- Electrolyte ImbalanceDocument44 paginiElectrolyte ImbalanceTiven StiveÎncă nu există evaluări
- Acute AppendisitisDocument27 paginiAcute AppendisitisTiven StiveÎncă nu există evaluări
- Kuliah Pengantar Epi, Pato, Klinik, Diagnosis MalariaDocument19 paginiKuliah Pengantar Epi, Pato, Klinik, Diagnosis MalariaTiven StiveÎncă nu există evaluări
- The Drug Therapy of Gastrointestinal, HepaticDocument37 paginiThe Drug Therapy of Gastrointestinal, HepaticTiven StiveÎncă nu există evaluări
- Kuliah Pengantar Epi, Pato, Klinik, Diagnosis MalariaDocument19 paginiKuliah Pengantar Epi, Pato, Klinik, Diagnosis MalariaTiven StiveÎncă nu există evaluări
- Malaria PropilaxixDocument2 paginiMalaria PropilaxixTiven StiveÎncă nu există evaluări
- Diagnosis of Tension-Type Headache, Migraine and Cluster HeadacheDocument1 paginăDiagnosis of Tension-Type Headache, Migraine and Cluster HeadacheTiven StiveÎncă nu există evaluări
- Corpus Callosum Agenesis and Rehabilitative, PediatricDocument7 paginiCorpus Callosum Agenesis and Rehabilitative, PediatricTiven StiveÎncă nu există evaluări
- TetanusDocument9 paginiTetanusTiven StiveÎncă nu există evaluări
- SCAE Aicardi SyndromeDocument2 paginiSCAE Aicardi SyndromeTiven StiveÎncă nu există evaluări
- Viral MeningitisDocument6 paginiViral Meningitisapi-3712326Încă nu există evaluări
- Carpal Tunnel SyndromeDocument2 paginiCarpal Tunnel SyndromeapinariyoÎncă nu există evaluări
- Neurogical DiseaseDocument7 paginiNeurogical DiseaseTiven StiveÎncă nu există evaluări
- Bayer Annual Report 2010Document273 paginiBayer Annual Report 2010James WuÎncă nu există evaluări
- Hematology: Presented by Alyazeed Hussein, BSCDocument96 paginiHematology: Presented by Alyazeed Hussein, BSCMONFOLAÎncă nu există evaluări
- TEP Jama 2022Document10 paginiTEP Jama 2022carla jazmin cortes rodriguezÎncă nu există evaluări
- Pro TaminaDocument2 paginiPro TaminaArcenciel26Încă nu există evaluări
- DVTDocument4 paginiDVTMàŗwā TāhāÎncă nu există evaluări
- Rivaroxaban PresentationDocument13 paginiRivaroxaban PresentationReem El-HusseinyÎncă nu există evaluări
- Secondary Stroke PreventionDocument54 paginiSecondary Stroke PreventionHùng Phạm Lý ChíÎncă nu există evaluări
- Postpartal ThrombophlebitisDocument8 paginiPostpartal ThrombophlebitisnursereviewÎncă nu există evaluări
- DVTDocument20 paginiDVTNachiket Vijay PotdarÎncă nu există evaluări
- Blood Transfusion & ComponentsDocument56 paginiBlood Transfusion & Componentsadithya polavarapuÎncă nu există evaluări
- Management of Acute Moderate and Severe Traumatic Brain Injury - UpToDateDocument80 paginiManagement of Acute Moderate and Severe Traumatic Brain Injury - UpToDateManuelEduardoSanchezSotoÎncă nu există evaluări
- Thrombophl Ebitis: Santos, Maria Ericka B. BSN Iii - 1Document39 paginiThrombophl Ebitis: Santos, Maria Ericka B. BSN Iii - 1Ericka SantosÎncă nu există evaluări
- Automatic Stop OrderDocument2 paginiAutomatic Stop OrderEva Myrna Sabalberino0% (1)
- Final DX ResultsDocument9 paginiFinal DX ResultszysheaiÎncă nu există evaluări
- S9 Clotting DisorderDocument87 paginiS9 Clotting Disorderelle70503Încă nu există evaluări
- MOH Therapeutic Protocol For COVID 19Document12 paginiMOH Therapeutic Protocol For COVID 19Faris Thomas FarisÎncă nu există evaluări
- Assessment and Management of The Unconscious PatientDocument6 paginiAssessment and Management of The Unconscious PatientRed DevilÎncă nu există evaluări
- 2023 MayDocument36 pagini2023 MayReshma Shaji PnsÎncă nu există evaluări
- ThrombocytopeniaDocument12 paginiThrombocytopeniatantyÎncă nu există evaluări
- National Inpatient Medication Chart User Guide - Including PediatricsDocument35 paginiNational Inpatient Medication Chart User Guide - Including PediatricsAnke Nemirovsky100% (1)
- Ischemic Stroke Management by The Nurse PR - 2019 - The Journal For Nurse PractDocument9 paginiIschemic Stroke Management by The Nurse PR - 2019 - The Journal For Nurse PractLina SafitriÎncă nu există evaluări
- Reabilitare Dupa AvcDocument91 paginiReabilitare Dupa AvcDiana StancaÎncă nu există evaluări
- Duration of Anticoagulation After Cerebral Venous Sinus Thrombosis 2012 Neurocritical CareDocument8 paginiDuration of Anticoagulation After Cerebral Venous Sinus Thrombosis 2012 Neurocritical Caremorris_tyoÎncă nu există evaluări
- Pertemuan 7 LiyanaDocument36 paginiPertemuan 7 LiyanaLiyana SafitriÎncă nu există evaluări
- 81 Byn VH PAHSDocument4 pagini81 Byn VH PAHSFaheem AwanÎncă nu există evaluări
- Igm Arc ChemDocument8 paginiIgm Arc Chembassam alharaziÎncă nu există evaluări
- Thrombotic Thrombocytopenic Purpura, Heparin-Induced Thrombocytopenia, and Disseminated Intravascular Coagulation 2020Document21 paginiThrombotic Thrombocytopenic Purpura, Heparin-Induced Thrombocytopenia, and Disseminated Intravascular Coagulation 2020Cris TobalÎncă nu există evaluări
- Hemiplegia Resource Book ModifiedDocument60 paginiHemiplegia Resource Book ModifiedAnonymous czrvb3hÎncă nu există evaluări