Documente Academic
Documente Profesional
Documente Cultură
Endocrine Glands
Încărcat de
Екатерина КостюкDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Endocrine Glands
Încărcat de
Екатерина КостюкDrepturi de autor:
Formate disponibile
Chapter 11
Endocrine Glands:
Secretion and Action of Hormones
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Endocrine Glands and Hormones
Secrete biologically
active molecules into
the blood.
Lack ducts.
Carry hormones to
target cells that
contain specific
receptor proteins for
that hormone.
Target cells can
respond in a specific
fashion.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Endocrine Glands and Hormones
(continued)
Neurohormone:
Specialized neurons that secrete chemicals into
the blood rather than synaptic cleft.
Chemical secreted is called neurohormone.
Hormones:
Affect metabolism of target organs.
Help regulate total body metabolism, growth, and
reproduction.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Chemical Classification of
Hormones
Amines:
Hormones derived from tyrosine and tryptophan.
NE, Epi, T
4
.
Polypeptides and proteins:
Polypeptides:
Chains of < 100 amino acids in length.
ADH.
Protein hormones:
Polypeptide chains with > 100 amino acids.
Growth hormone.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Chemical Classification of
Hormones (continued)
Lipids derived from cholesterol.
Are lipophilic hormones.
Testosterone.
Estradiol.
Cortisol.
Progesterone.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Chemical Classification of
Hormones (continued)
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Chemical Classification of
Hormones (continued)
Glycoproteins:
Long polypeptides (>100) bound to 1 or more
carbohydrate (CHO) groups.
FSH and LH.
Hormones can also be divided into:
Polar:
H
2
0 soluble.
Nonpolar (lipophilic):
H
2
0 insoluble.
Can gain entry into target cells.
Steroid hormones and T
4
.
Pineal gland secretes melatonin:
Has properties of both H
2
0 soluble and lipophilic hormones.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Prohormones and Prehormones
Prohormone:
Precursor is a longer chained polypeptide that is
cut and spliced together to make the hormone.
Proinsulin.
Preprohormone:
Prohormone derived from larger precursor
molecule.
Preproinsulin.
Prehormone:
Molecules secreted by endocrine glands that are
inactive until changed into hormones by target
cells.
T
4
converted to T
3
.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Common Aspects of Neural and
Endocrine Regulation
APs are chemical events produced by diffusion of
ions through neuron plasma membrane.
Action of some hormones are accompanied by ion
diffusion and electrical changes in the target cell.
Nerve axon boutons release NTs.
Some chemicals are secreted as hormones, and also are
NTs.
In order for either a NT or hormone to function in
physiological regulation:
Target cell must have specific receptor proteins.
Combination of the regulatory molecule with its receptor
proteins must cause a specific sequence of changes.
There must be a mechanism to quickly turn off the action of
a regulator.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Synergistic:
Two hormones work together to produce a
result.
Additive:
Each hormone separately produces response,
together at same concentrations stimulate even
greater effect.
NE and Epi.
Complementary:
Each hormone stimulates different step in the
process.
FSH and testosterone.
Hormonal Interactions
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Hormonal Interactions (continued)
Permissive effects:
Hormone enhances the responsiveness of a
target organ to second hormone.
Increases the activity of a second hormone.
Prior exposure of uterus to estrogen induces
formation of receptors for progesterone.
Antagonistic effects:
Action of one hormone antagonizes the effects
of another.
Insulin and glucagon.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Effects of [Hormone] on Tissue
Response
[Hormone] in blood reflects the rate of
secretion.
Half-life:
Time required for the blood [hormone] to be
reduced to reference level.
Minutes to days.
Normal tissue responses are produced only
when [hormone] are present within
physiological range.
Varying [hormone] within normal, physiological
range can affect the responsiveness of target
cells.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Effects of [Hormone] on Tissue
Response (continued)
Priming effect (upregulation):
Increase number of receptors formed on target
cells in response to particular hormone.
Greater response by the target cell.
Desensitization (downregulation):
Prolonged exposure to high [polypeptide
hormone].
Subsequent exposure to the same [hormone] produces
less response.
Decrease in number of receptors on target cells.
Insulin in adipose cells.
Pulsatile secretion may prevent downregulation.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Mechanisms of Hormone Action
Hormones of same chemical class have
similar mechanisms of action.
Similarities include:
Location of cellular receptor proteins depends
on the chemical nature of the hormone.
Events that occur in the target cells.
To respond to a hormone:
Target cell must have specific receptors for
that hormone (specificity).
Hormones exhibit:
Affinity (bind to receptors with high bond strength).
Saturation (low capacity of receptors).
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Hormones That Bind to Nuclear
Receptor Proteins
Lipophilic steroid and
thyroid hormones are
attached to plasma
carrier proteins.
Hormones dissociate
from carrier proteins to
pass through lipid
component of the target
plasma membrane.
Receptors for the
lipophilic hormones are
known as nuclear
hormone receptors.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Nuclear Hormone Receptors
Steroid receptors are located in cytoplasm and in the
nucleus.
Function within cell to activate genetic transcription.
Messenger RNA directs synthesis of specific enzyme proteins
that change metabolism.
Each nuclear hormone receptor has 2 regions:
A ligand (hormone)-binding domain.
DNA-binding domain.
Receptor must be activated by binding to hormone
before binding to specific region of DNA called HRE
(hormone responsive element).
Located adjacent to gene that will be transcribed.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Mechanisms of Steroid Hormone
Action
Cytoplasmic receptor
binds to steroid
hormone.
Translocates to nucleus.
DNA-binding domain
binds to specific HRE of
the DNA.
Dimerization occurs.
Process of 2 receptor
units coming together at
the 2 half-sites.
Stimulates transcription
of particular genes.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Mechanism of Thyroid Hormone
Action
T
4
passes into cytoplasm and
is converted to T
3
.
Receptor proteins located in
nucleus.
T
3
binds to ligand-binding
domain.
Other half-site is vitamin A
derivative (9-cis-retinoic)
acid.
DNA-binding domain can
then bind to the half-site of
the HRE.
Two partners can bind to
the DNA to activate HRE.
Stimulate transcription of
genes.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Hormones That Use 2
nd
Messengers
Hormones cannot pass through plasma
membrane use 2
nd
messengers.
Catecholamine, polypeptide, and glycoprotein
hormones bind to receptor proteins on the
target plasma membrane.
Actions are mediated by 2
nd
messengers
(signal-transduction mechanisms).
Extracellular hormones are transduced
into intracellular 2
nd
messengers.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Polypeptide or glycoprotein hormone
binds to receptor protein causing
dissociation of a subunit of G-protein.
G-protein subunit binds to and activates
adenylate cyclase.
ATP cAMP + PP
i
cAMP attaches to inhibitory subunit of
protein kinase.
Inhibitory subunit dissociates and
activates protein kinase.
Adenylate Cyclase-cAMP
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Adenylate Cyclase-cAMP (continued)
Phosphorylates
enzymes within the
cell to produce
hormones effects.
Modulates activity of
enzymes present in
the cell.
Alters metabolism of
the cell.
cAMP inactivated by
phosphodiesterase.
Hydrolyzes cAMP
to inactive
fragments.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Binding of Epi to a-adrenergic receptor
in plasma membrane activates a G-
protein intermediate, phospholipase C.
Phospholipase C splits phospholipid into
IP
3
and DAG.
Both derivatives serve as 2
nd
messengers.
IP
3
diffuses through cytoplasm to ER.
Binding of IP
3
to receptor protein in ER
causes Ca
2+
channels to open.
Phospholipase-C-Ca
2+
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Phospholipase-C-Ca
2+
(continued)
Ca
2+
diffuses into
the cytoplasm.
Ca
2+
binds to
calmodulin.
Calmodulin
activates specific
protein kinase
enzymes.
Alters the
metabolism of the
cell, producing
the hormones
effects.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Epi Can Act Through Two 2
nd
Messenger Systems
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Tyrosine Kinase
Insulin receptor consists of 2 units that dimerize
when they bind with insulin.
Insulin binds to ligandbinding site on plasma
membrane, activating enzymatic site in the cytoplasm.
Autophosphorylation occurs, increasing tyrosine
kinase activity.
Activates signaling molecules.
Stimulate glycogen, fat and protein synthesis.
Stimulate insertion of GLUT-4 carrier proteins.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Tyrosine Kinase (continued)
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Pituitary Gland
Pituitary gland is
located in the
diencephalon.
Structurally and
functionally
divided into:
Anterior lobe.
Posterior lobe.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Anterior pituitary:
Master gland (adenohypophysis).
Derived from a pouch of epithelial tissue that
migrates upward from the mouth.
Consists of 2 parts:
Pars distalis: anterior pituitary.
Pars tuberalis: thin extension in contact with the
infundibulum.
Posterior pituitary(neurohypophysis):
Formed by downgrowth of the brain during fetal
development.
Is in contact with the infundibulum.
Nerve fibers extend through the infundibulum.
Pituitary Gland (continued)
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Pituitary Hormones
Anterior Pituitary:
Trophic effects:
High blood
[hormone] causes
target organ to
hypertrophy.
Low blood
[hormone] causes
target organ to
atrophy.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Pituitary Hormones (continued)
Posterior pituitary:
Stores and releases 2 hormones that are
produced in the hypothalamus:
Antidiuretic hormone (ADH/vasopressin):
Promotes the retention of H
2
0 by the kidneys.
Less H
2
0 is excreted in the urine.
Oxytocin:
Stimulates contractions of the uterus during parturition.
Stimulates contractions of the mammary gland alveoli.
Milk-ejection reflex.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Hypothalamic Control of
Posterior Pituitary
Hypothalamus neuron
cell bodies produce:
ADH: supraoptic
nuclei.
Oxytocin:
paraventricular nuclei.
Transported along
the hypothalamo-
hypophyseal tract.
Stored in posterior
pituitary.
Release controlled by
neuroendocrine
reflexes.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Hypothalamic Control of the
Anterior Pituitary
Hormonal control rather
than neural.
Hypothalamus neurons
synthesize releasing and
inhibiting hormones.
Hormones are transported
to axon endings of
median eminence.
Hormones secreted into
the hypothalamo-
hypophyseal portal
system regulate the
secretions of the anterior
pituitary
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Anterior pituitary and hypothalamic secretions
are controlled by the target organs they
regulate.
Secretions are controlled by negative feedback
inhibition by target gland hormones.
Negative feedback at 2 levels:
The target gland hormone can act on the
hypothalamus and inhibit secretion of releasing
hormones.
The target gland hormone can act on the anterior
pituitary and inhibit response to the releasing
hormone.
Feedback Control of the Anterior
Pituitary
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Feedback Control of the Anterior
Pituitary (continued)
Short feedback loop:
Retrograde transport of
blood from anterior
pituitary to the
hypothalamus.
Hormone released by
anterior pituitary
inhibits secretion of
releasing hormone.
Positive feedback
effect:
During the menstrual
cycle, estrogen
stimulates LH surge.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Higher Brain Function and
Pituitary Secretion
Axis:
Relationship between anterior pituitary and
a particular target gland.
Pituitary-gonad axis.
Hypothalamus receives input from
higher brain centers.
Psychological stress affects:
Circadian rhythms.
Menstrual cycle.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Adrenal Glands
Paired organs that cap the kidneys.
Each gland consists of an outer cortex and
inner medulla.
Adrenal medulla:
Derived from embryonic neural crest
ectoderm (same tissue that produces the
sympathetic ganglia).
Synthesizes and secretes:
Catecholamines (mainly Epi but some NE).
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Adrenal Glands (continued)
Adrenal cortex:
Does not receive
neural innervation.
Must be stimulated
hormonally (ACTH).
Consists of 3 zones:
Zona glomerulosa.
Zona fasciculata.
Zona reticularis.
Secretes
corticosteroids.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Functions of the Adrenal Cortex
Zona glomerulosa:
Mineralcorticoids (aldosterone):
Stimulate kidneys to reabsorb Na
+
and secrete
K
+
.
Zona fasciculata:
Glucocorticoids (cortisol):
Inhibit glucose utilization and stimulate
gluconeogenesis.
Zona reticularis (DHEA):
Sex steroids:
Supplement sex steroids.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Functions of the Adrenal Cortex
(continued)
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Functions of the Adrenal
Medulla
Innervated by preganglionic
sympathetic axons.
Increase respiratory rate.
Increase HR and cardiac output.
Vasoconstrict blood vessels, thus
increasing venous return.
Stimulate glycogenolysis.
Stimulate lipolysis.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Stress and the Adrenal Gland
Non-specific response
to stress produces the
general adaptation
syndrome (GAS).
Alarm phase:
Adrenal glands
activated.
Stage of resistance:
Stage of readjustment.
Stage of exhaustion:
Sickness and/or death
if readjustment is not
complete.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Thyroid Hormones
Thyroid gland is located
just below the larynx.
Thyroid is the largest of
the pure endocrine
glands.
Follicular cells secrete
thyroxine.
Parafollicular cells
secrete calcitonin.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Production of Thyroid Hormones
Iodide (I
-
) actively transported into the
follicle and secreted into the colloid.
Oxidized to iodine (I
o
).
Iodine attached to tyrosine within
thyroglobulin chain.
Attachment of 1 iodine produces
monoiodotyrosine (MIT).
Attachment of 2 iodines produces diiodotyrosine
(DIT).
MIT and DIT or 2 DIT molecules coupled
together.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Production of Thyroid Hormones
(continued)
T
3
and T
4
produced.
TSH stimulates pinocytosis into the follicular
cell.
Enzymes hydrolyze T
3
and T
4
from
thyroglobulin.
Attached to TBG and released into blood.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Production of Thyroid Hormones
(continued)
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Actions of T
3
Stimulates protein synthesis.
Promotes maturation of nervous system.
Stimulates rate of cellular respiration by:
Production of uncoupling proteins.
Increase active transport by Na
+
/K
+
pumps.
Lower cellular [ATP].
Increases metabolic heat.
Increases metabolic rate.
Stimulates increased consumption of glucose, fatty
acids and other molecules.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Diseases of the Thyroid
Iodine-deficiency
(endemic) goiter:
Abnormal growth of
the thyroid gland.
In the absence of
sufficient iodine,
cannot produce
adequate amounts of
T
4
and T
3
.
Lack of negative
feedback inhibition.
Stimulates TSH,
which causes
abnormal
growth.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Diseases of the Thyroid (continued)
[Iodine-deficiency (endemic) goitercontinued]
Adult myxedema:
Accumulation of mucoproteins and fluid in subcutaneous tissue.
Symptoms:
Decreased metabolic rate.
Weight gain.
Decreased ability to adapt to cold.
Lethargy.
Graves disease:
Autoimmune disorder:
Exerts TSH-like effects on thyroid.
Not affected by negative feedback.
Cretinism:
Hypothyroid from end of 1
st
trimester to 6 months postnatally.
Severe mental retardation.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Parathyroid Glands
Embedded in the lateral
lobes of the thyroid gland.
Parathyroid hormone (PTH):
Only hormone secreted by
the parathyroid glands.
Single most important
hormone in the control of
blood [Ca
2+
].
Stimulated by decreased
blood [Ca
2+
].
Promotes rise in blood [Ca
2+
]
by acting on bones, kidney
and intestines.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Pancreatic Islets (Islets of
Langerhans)
Alpha cells secrete glucagon.
Stimulus is decrease in
blood [glucose].
Stimulates glycogenolysis
and lipolysis.
Stimulates conversion of
fatty acids to ketones.
Beta cells secrete insulin.
Stimulus is increase in blood
[glucose].
Promotes entry of glucose
into cells.
Converts glucose to
glycogen and fat.
Aids entry of amino acids
into cells.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Pineal Gland
Secretes melatonin:
Production stimulated by the suprachiasmatic nucleus (SCN)
in hypothalamus.
SCN is primary center for circadian rhythms.
Light/dark changes required to synchronize.
Melatonin secretion increases with darkness and peaks in
middle of night.
May inhibit GnRH.
May function in the onset of puberty (controversial).
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Pineal Gland (continued)
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Thymus
Site of production of T cells (thymus-
dependent cells), which are lymphocytes.
Lymphocytes are involved in cell-mediated
immunity.
Secretes hormones that are believed to
stimulate T cells after leave thymus.
Thymus gland size is large in newborns and
children.
Regresses after puberty and becomes
infiltrated with strands of fibrous tissue.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Gonads and Placenta
Gonads (testes and ovaries):
Secrete sex hormones.
Testosterone.
Estradiol 17-b.
After menopause, produces estrone.
Progesterone.
Placenta:
Secretes large amounts of estriol,
progesterone, hCG, hCS.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Autocrine and Paracrine
Regulation
Autocrine:
Produced and act within the same tissue of an organ.
All autocrine regulators control gene expression in target cells.
Paracrine:
Produced within one tissue and regulate a different tissue of
the same organ.
Cytokines (lymphokines):
Regulate different cells (interleukins) .
Growth factors:
Promote growth and cell division in any organ.
Neutrophins:
Guide regenerating peripheral neurons.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Prostaglandins
Most diverse group of autocrine regulators.
Produced in almost every organ.
Wide variety of functions.
Different prostaglandins may exert antagonistic
effects in some tissues.
Immune system:
Promote inflammatory process.
Reproductive system:
Play role in ovulation.
Digestive system:
Inhibit gastric secretion.
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Prostaglandins (continued)
Copyright The McGraw-Hill Companies, Inc. Permission required for reproduction or display.
Prostaglandins (continued)
Respiratory system:
May bronchoconstrict or bronchodilate.
Circulatory system:
Vasoconstrictors or vasodilators.
Urinary system:
Vasodilation.
Inhibitors of prostaglandin synthesis:
Non-steroidal anti-inflammatory drugs (NSAIDS).
Aspirin, indomethacin, ibuprofen: inhibit COX1.
Celecoxib and rofecoxib: inhibit COX2.
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Topographicanatomy Lowerlimb TiskDocument68 paginiTopographicanatomy Lowerlimb TiskЕкатерина КостюкÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- IIEF-5 Questionnaire PDFDocument1 paginăIIEF-5 Questionnaire PDFOka Widya Putra100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- EASL Haemochromatosis GuidelinesDocument26 paginiEASL Haemochromatosis Guidelinesmonday125Încă nu există evaluări
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- Acspc 046379Document84 paginiAcspc 046379Екатерина КостюкÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
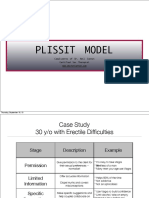
- Plissit PDFDocument5 paginiPlissit PDFЕкатерина КостюкÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- IIEF-5 Questionnaire PDFDocument1 paginăIIEF-5 Questionnaire PDFOka Widya Putra100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Malaria DiagnosisDocument82 paginiMalaria DiagnosisЕкатерина КостюкÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Doze ExamenDocument4 paginiDoze ExamenЕкатерина КостюкÎncă nu există evaluări
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Indicatii ExamenDocument4 paginiIndicatii ExamenЕкатерина КостюкÎncă nu există evaluări
- Pink Panther - Diabetes Management - Chapter 6Document14 paginiPink Panther - Diabetes Management - Chapter 6jennmoyer100% (2)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- The American Psychiatric Publishing Textbook of Psychopharmacology 4th EdDocument1.858 paginiThe American Psychiatric Publishing Textbook of Psychopharmacology 4th EdIulia Mohai96% (25)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Ch05 Lecture-Cell Membranes and SignalingDocument95 paginiCh05 Lecture-Cell Membranes and SignalingbearreÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- S1 DPG Jeffrey A 2014 Bordtella Pertussis PathogenesisDocument15 paginiS1 DPG Jeffrey A 2014 Bordtella Pertussis PathogenesisAyerim Valeria Rojas DiazÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- USMLE Step 1 DrugsDocument36 paginiUSMLE Step 1 DrugscougardiverÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- Medicinal Chemistry/ CHEM 458/658 Chapter 8-Receptors and MessengersDocument41 paginiMedicinal Chemistry/ CHEM 458/658 Chapter 8-Receptors and MessengersMehak SarfrazÎncă nu există evaluări
- ReceptorsDocument9 paginiReceptorsrajenderÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Chapter 5 Vert Phys Students)Document76 paginiChapter 5 Vert Phys Students)Kertayvia Yepwekan HarrisÎncă nu există evaluări
- Receptors IntroductionDocument53 paginiReceptors IntroductionSunilÎncă nu există evaluări
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Cell Communication NotesDocument3 paginiCell Communication NoteselyssaÎncă nu există evaluări
- A Seminar Presentation On Mechanism of Drug ActionDocument40 paginiA Seminar Presentation On Mechanism of Drug Actionbellatrix aliaÎncă nu există evaluări
- Cell CommunicationDocument45 paginiCell CommunicationWilson HindartoÎncă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Hitchhiker's Guide To Clinical Pharmacology: Pharmacodynamics: How Drugs WorkDocument23 paginiThe Hitchhiker's Guide To Clinical Pharmacology: Pharmacodynamics: How Drugs WorkMylz MendozaÎncă nu există evaluări
- ENDOCRINOLOGY Notes 2 PDFDocument131 paginiENDOCRINOLOGY Notes 2 PDFkomal pattabiÎncă nu există evaluări
- Histamine and Antihistamines: Learning ObjectivesDocument6 paginiHistamine and Antihistamines: Learning Objectivesgeorgi.annaÎncă nu există evaluări
- General Pharmacodynamic PrinciplesDocument7 paginiGeneral Pharmacodynamic PrinciplesKrizza Camere100% (1)
- Gpcrs and CancervistaDocument45 paginiGpcrs and CancervistapriyaaÎncă nu există evaluări
- Course 12 - NeurotransmitersDocument40 paginiCourse 12 - NeurotransmitersPopa NicuÎncă nu există evaluări
- Signal Transduction in Prokaryotes and Eukaryotes-FinalDocument66 paginiSignal Transduction in Prokaryotes and Eukaryotes-FinalAsif gill0% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Drug TargetDocument35 paginiDrug Targetsri nurlatipahÎncă nu există evaluări
- Physiology Magdy Sabry EndocrineDocument162 paginiPhysiology Magdy Sabry Endocrineaminata kamara89% (9)
- Introduction To Endocrinology (Chapter 75) : Lacaden, LMGCDocument4 paginiIntroduction To Endocrinology (Chapter 75) : Lacaden, LMGCKC White Dela Rosa100% (1)
- Anatomy and Physiology Chapter 17Document21 paginiAnatomy and Physiology Chapter 17Dawlat SlamaÎncă nu există evaluări
- TMP D19 CDocument124 paginiTMP D19 CFrontiersÎncă nu există evaluări
- 1 Cholinergic & Noradrenergic Transmission IDocument37 pagini1 Cholinergic & Noradrenergic Transmission IGeraldine Ong100% (2)
- 02 Hormones PDFDocument8 pagini02 Hormones PDFKaram SaadÎncă nu există evaluări
- Biol 1205 - Chapter 5 - D2L - W2023Document44 paginiBiol 1205 - Chapter 5 - D2L - W2023Bray RobertsonÎncă nu există evaluări
- 7.013 Pset 4 PDFDocument12 pagini7.013 Pset 4 PDF15klaÎncă nu există evaluări
- BiochemistryDocument82 paginiBiochemistryAmritzz Paul83% (6)
- Target Mds Aiims Mock PDFDocument22 paginiTarget Mds Aiims Mock PDFReddyÎncă nu există evaluări
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Farmakologi FarmakodinamikDocument26 paginiFarmakologi FarmakodinamikMuhammad Nikko AomadaniÎncă nu există evaluări