Documente Academic
Documente Profesional
Documente Cultură
Pharmaceutical Isolator Technology
Încărcat de
Florin PătrulescuDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Pharmaceutical Isolator Technology
Încărcat de
Florin PătrulescuDrepturi de autor:
Formate disponibile
Pharmaceutical Isolator
Technology
Thinking inside the box
Filling in the Fifties
Isolators
Are environments which are sealed, or
supplied with microbially retentive filtered
air, and are reproducibly decontaminated.
When closed, use only decontaminated
interfaces or transfer devices which
preclude contamination.
Are recognized to be superior for product
and/or operator protection when designed
and operated appropriately.
The Isolation Continuum
B
i
o
s
a
f
e
t
y
C
a
b
i
n
e
t
L
a
m
i
n
a
r
F
l
o
w
H
o
o
d
C
l
a
s
s
i
f
i
e
d
R
o
o
m
Isolators
Containment
Aseptic
I
n
c
r
e
a
s
i
n
g
R
e
l
i
a
b
i
l
i
t
y
o
f
O
p
e
r
a
t
i
o
n
Positive Pressure
Negative Pressure
Increased sterility assurance Increased worker protection
Conventional Cleanroom Mfg
Heavy requirements for
operator training and
monitoring
Sterile gowning
certification required
Relies on continuous
high airflow for
protection
Entire rooms designed
to be essentially aseptic
Isolator-based Mfg
No requirement for
sterile gowning
Background
classified to ISO8
No direct contact
between people and
product
Drastic reduction in
sterile airflow
requirements
Added flexibility for
multi-product usage
Functions For An Isolator
Operator Interface
Isolator Design Fundamentals
Isolator Instrumentation
Pressure monitoring and control
Modes
Run
Leak-test
Decontaminate
Aerate
Particle monitoring
Temp/Humidity
Airflow
Closed isolators acceptable with turbulent
airflow
May employ localized unidirectional airflow
Open isolators use unidirectional strictly
True unidirectional air, as velocities and
space do not generate any laminarity
May be operated in positive or negative
pressure, dependent upon containment or
aseptic
Closed vs. Open Isolators
Closed
Tightly sealed units
Often turbulent airflow
Ceiling air supply and
exhaust
Simpler to design and
operate
Easier to validate
Lowest risk aseptic
process
Open
Utilize mouseholes
for material ingress
and egress
Use unidirectional air
Rely on adequate
airflow to preclude
contamination
Faster throughput
Larger capacities
Rapid Transfer System
Isolator Designs
Flexible wall
PVC Bag with
support
Lighter
Cheaper
Less puncture
resistant
Longer aeration
times
Isolator Designs
Rigid Wall
More puncture
resistant
Short aeration time
Less Pressure
fluctuation
More customizable
Isolator Mock-up
Key step in
design
Assess
ergonomics
Place
instrumentation
No two
isolators are
the same
Leak Testing
Tested during
assembly
Tested daily in
operation
Set on low, but
measurable rate
Important for
VHP safety and
aseptic
operation
Syringe Filling Isolator Line
Sterility Test Isolator
Integrated Vial Filling Line
Rigid Wall Plastic Isolator
Compounding Isolator
Tank able to attach with
RTP
Allows for contained
compounding of
hazardous materials
Able to provide
pos./neg. pressure
Anaerobic
compounding possible
Isolated Robotics
New, next step in
aseptic technology
Sealed, VHP-
compatible robotics
Eliminates need for
most ergonomics
Removes human
intervention at greater
level
Decontamination
Concept now used to
define isolator
environmental control
Repeatable method to
destroy all likely
contaminating
organisms
Not sterilization
High end, automated
sanitization
Sterilization
Absence of viable microorganisms
Generally regarded as a Probability of Non-
Sterile Unit at one in a million (PNSU 10
-6
)
Inversely, Sterility Assurance Level (SAL 10
6
)
Dependent upon controlled conditions and
defendable data
Sterilization & Decontamination
Measured by Biological Indicator
Destruction
Use Spores as challenge organism
BI use coupons, discs, etc. holding a
population of spores
Most common sterilization to use overkill
approach
A science based upon probability, not
perfection
PNSU/SAL
-6
-4
-2
0
2
4
6
0 5 10 15 20 25 30
Time (min.)
S
p
o
r
e
P
o
p
u
l
a
t
i
o
n
(
L
o
g
)
Validate
Total Kill
GMP Cycle
Decontamination
GASSING
RETURN
Enclosure
Phase 1 Pre-Conditioning
Phase 2 - Gassing
- Gas dwell
Phase 3 Aeration
VHP - Cycle Stages
VHP Cycle Parameters
Humidity inside the Isolator at the beginning of
gassing
Injection rate of hydrogen peroxide
Switching point from gassing phase to dwell phase
Exposure time
Gas concentration
Temperature of the surface to be decontaminated
Temperature inside the isolator
Gas distribution
Ambient temperature
Reliable Cycle Development
Uniformity of temperature on surface
to be decontaminated.
Especially at beginning of gassing phase
Adequate distribution of VHP
throughout space to be
decontaminated.
Rapid discharge of VHP from system in
aeration
Reproducibility of cycle developed
Isolator Decontamination
Many agents have been employed:
Peroxyacetic acid
Chlorine Dioxide
Steam/Peroxide
Ozone
Formaldehyde
Vapourized Hydrogen Peroxide
VHP most common today
Operating Technique
Not Sterile Processing
Relies upon good, consistent aseptic
technique
Motion as/more important as in cleanroom,
due to small size of space
Cleaning and material compatibility key for
particulate control
Historic Problems
Extreme difficulties in demonstrating
Sterilization and Sterile Processing
Overcomplicated and leaky designs
Perfection set as goal
Zero leak spec
Sterile
Materials and decon agent compatibility
Just equipment in a box
Summary
Now generally accepted
technology
Relies upon solid
design and operation
practices
Widely held as the
superior aseptic
technology
Highly adaptable with
associated devices and
methods
S-ar putea să vă placă și
- Manual of Avionics PDFDocument300 paginiManual of Avionics PDFJhony BhatÎncă nu există evaluări
- IVT Cleaning Validation IV 0Document87 paginiIVT Cleaning Validation IV 0Noemi100% (7)
- 12 Sterile ProductionDocument140 pagini12 Sterile ProductionsamirneseemÎncă nu există evaluări
- Cleanroom Technology: Fundamentals of Design, Testing and OperationDe la EverandCleanroom Technology: Fundamentals of Design, Testing and OperationÎncă nu există evaluări
- Cleanroom Technology, Contamination Control and CleaningDocument190 paginiCleanroom Technology, Contamination Control and CleaningMihailo Vrzic100% (2)
- Cleanroom A Complete Guide - 2021 EditionDe la EverandCleanroom A Complete Guide - 2021 EditionEvaluare: 5 din 5 stele5/5 (2)
- Containment in PharmaDocument271 paginiContainment in PharmaArRashidRashid100% (2)
- NE25. Sterilizing Liquid Filtration TR26Document32 paginiNE25. Sterilizing Liquid Filtration TR26ghostllhÎncă nu există evaluări
- F0 What It Means - How To Calculate It - How To Use Itv3 PDFDocument34 paginiF0 What It Means - How To Calculate It - How To Use Itv3 PDFJosé Manuel Pais-Chanfrau100% (1)
- Critical Utility QualificationDocument14 paginiCritical Utility QualificationYayan IrawanÎncă nu există evaluări
- 6 - Clean Room Validation RequirmentsDocument3 pagini6 - Clean Room Validation Requirmentsvijaysirsat2007100% (1)
- PDA TR Nº40 Sterilizing Filtration of Gases PDFDocument45 paginiPDA TR Nº40 Sterilizing Filtration of Gases PDFehsan050628Încă nu există evaluări
- Clean Room - Clean Room & HVAC SystemsDocument74 paginiClean Room - Clean Room & HVAC Systemspchakravarty_2100% (8)
- Aseptic Processing Risk Assessment The Simplified Akers Agalloco MethodDocument55 paginiAseptic Processing Risk Assessment The Simplified Akers Agalloco MethodDoan Chi ThienÎncă nu există evaluări
- 747Document12 pagini747GurdevBaines100% (3)
- Bài Tập Bổ Trợ Nâng Cao Tiếng Anh 7-8-9 Chương Trình Mới (1) -Trang-292-433Document142 paginiBài Tập Bổ Trợ Nâng Cao Tiếng Anh 7-8-9 Chương Trình Mới (1) -Trang-292-433Nguyễn Lâm ThươngÎncă nu există evaluări
- Airflow Pattern StudiesDocument18 paginiAirflow Pattern Studiessainath_84100% (1)
- Media Fill ChecklistDocument11 paginiMedia Fill ChecklistSilke Igemann100% (1)
- Technical and Qualification Issues: Alain KupfermanDocument65 paginiTechnical and Qualification Issues: Alain Kupfermanjonh366100% (1)
- Risk Management For Aseptic ProcessingDocument9 paginiRisk Management For Aseptic Processinggbra80100% (1)
- 15702, Maintenance and Facilities OutsourDocument6 pagini15702, Maintenance and Facilities OutsournabilbyÎncă nu există evaluări
- Sterile Product Manufacturing PDFDocument28 paginiSterile Product Manufacturing PDFAnis ouch67% (3)
- Best Practices For Critical Sterile Filter Operation: A Case StudyDocument5 paginiBest Practices For Critical Sterile Filter Operation: A Case StudySailendra Meher50% (2)
- Barrier Technology: Rabs & Isolators For Aseptic ProcessingDocument16 paginiBarrier Technology: Rabs & Isolators For Aseptic ProcessingalnichmÎncă nu există evaluări
- Cleanroom Design, Construction, and QualificationDocument10 paginiCleanroom Design, Construction, and QualificationApoloTrevinoÎncă nu există evaluări
- Clean Room Presentation ISPEDocument62 paginiClean Room Presentation ISPEBNPARIKH75% (4)
- Risk Management in Sterile EnvironmentsDocument30 paginiRisk Management in Sterile EnvironmentsTim Sandle100% (4)
- Design of Containemt IsolatorsDocument72 paginiDesign of Containemt IsolatorsSweekar Borkar50% (2)
- Good Manufacturing Practices (GMP) Modules for Pharmaceutical ProductsDe la EverandGood Manufacturing Practices (GMP) Modules for Pharmaceutical ProductsÎncă nu există evaluări
- ILFD Lyophilization Process Validation 04-14-10 One Slide PeDocument102 paginiILFD Lyophilization Process Validation 04-14-10 One Slide Peboddarambabu100% (1)
- Appendix 1 URS For Isolator and Safety CabinetsDocument31 paginiAppendix 1 URS For Isolator and Safety Cabinetsgarys100% (3)
- Media Fills and Environment Atl Monitoring 26 July 2011 Presentation OneDocument18 paginiMedia Fills and Environment Atl Monitoring 26 July 2011 Presentation OneRiccardo TorelliÎncă nu există evaluări
- Lyophilization of Pharmaceutical and Biological Products, Rey (2004)Document21 paginiLyophilization of Pharmaceutical and Biological Products, Rey (2004)Shenshen CaiÎncă nu există evaluări
- Principles and Practices of Contamination Control and CleanroomsDe la EverandPrinciples and Practices of Contamination Control and CleanroomsÎncă nu există evaluări
- 2013-840 Guidance 11-25-14 Supac Adendum For EquipmentDocument48 pagini2013-840 Guidance 11-25-14 Supac Adendum For EquipmentEdy TeranÎncă nu există evaluări
- Integrated Process Equipment Into High Containment System: Presented byDocument44 paginiIntegrated Process Equipment Into High Containment System: Presented byMauliana Tiani Marsaid100% (1)
- Risk Management For Aseptic Processing PDFDocument9 paginiRisk Management For Aseptic Processing PDFArmando SaldañaÎncă nu există evaluări
- Pressure Cascade in CleanroomDocument39 paginiPressure Cascade in CleanroomPhạm Quang HuyÎncă nu există evaluări
- RABS and Isolators Barrier TechnologyDocument44 paginiRABS and Isolators Barrier TechnologySilke IgemannÎncă nu există evaluări
- Romaco Aseptic Powder Filling-EnDocument24 paginiRomaco Aseptic Powder Filling-EnWinoto HadiprodjoÎncă nu există evaluări
- Cross Contamination Control Facility DesignDocument22 paginiCross Contamination Control Facility DesignAlok Kumar SharmaÎncă nu există evaluări
- GEA Niro Fuid Bed TechnologyDocument16 paginiGEA Niro Fuid Bed Technologychien_yu_leeÎncă nu există evaluări
- CIP Cycle Development Sep04Document7 paginiCIP Cycle Development Sep04John HigginsÎncă nu există evaluări
- Checklist For Rebar and Concrete WorkDocument4 paginiChecklist For Rebar and Concrete WorkDwinto RachmadÎncă nu există evaluări
- Validation of Process Gas SystemsDocument6 paginiValidation of Process Gas SystemsJuan Manuel Valdez Von FürthÎncă nu există evaluări
- Biosafety Cabinet Manual 23Document5 paginiBiosafety Cabinet Manual 23Kate EtienamÎncă nu există evaluări
- Production of Plasma Proteins for Therapeutic UseDe la EverandProduction of Plasma Proteins for Therapeutic UseEvaluare: 3 din 5 stele3/5 (5)
- Designing A Facility With Both GMP and Biosafety in MindDocument10 paginiDesigning A Facility With Both GMP and Biosafety in MindLemlogÎncă nu există evaluări
- Validation Part2Document48 paginiValidation Part2gvasÎncă nu există evaluări
- PUW and WFI Systems DesignDocument43 paginiPUW and WFI Systems DesignAhmad ZaidiÎncă nu există evaluări
- Aseptic ProcessingDocument63 paginiAseptic ProcessingAmir Ilyas100% (1)
- PHSS - Clarity - in - GMP - Guidance - Barrier - Isolator - Technology - Leak Integrity Classes - v1Document12 paginiPHSS - Clarity - in - GMP - Guidance - Barrier - Isolator - Technology - Leak Integrity Classes - v1AkuWilliamsÎncă nu există evaluări
- CIP Cycle Development ISPEDocument9 paginiCIP Cycle Development ISPEvijayns_250355172Încă nu există evaluări
- Legislation Statutory Inspection ChecklistDocument2 paginiLegislation Statutory Inspection ChecklistAry PutraÎncă nu există evaluări
- RABSDocument51 paginiRABSPrem Kumar100% (2)
- HEPA Filter Leak Test PDFDocument34 paginiHEPA Filter Leak Test PDFjoe bloggs100% (1)
- EUGMP Annex 1 Update 2008 Particle CountingDocument7 paginiEUGMP Annex 1 Update 2008 Particle CountingKye Hwan KimÎncă nu există evaluări
- 2risk MaPPandContainment PharmaForum2011 1Document35 pagini2risk MaPPandContainment PharmaForum2011 1Steven LambertÎncă nu există evaluări
- Validation of Terminal Sterilization PDFDocument14 paginiValidation of Terminal Sterilization PDFjpabloqf100% (1)
- E05 Weikmann Automated Visual InspectionDocument12 paginiE05 Weikmann Automated Visual InspectionFlorin PătrulescuÎncă nu există evaluări
- Contamination Control in Cleanrooms - TexwipeDocument43 paginiContamination Control in Cleanrooms - TexwipeKristian Uriel DelgadoÎncă nu există evaluări
- Pilot Plant Scale Up of Inject Able Sand Liquid OralsDocument38 paginiPilot Plant Scale Up of Inject Able Sand Liquid OralsPradeep BhimaneniÎncă nu există evaluări
- Downstream Industrial Biotechnology: Recovery and PurificationDe la EverandDownstream Industrial Biotechnology: Recovery and PurificationÎncă nu există evaluări
- Airflow Pattern StudiesDocument29 paginiAirflow Pattern StudiesBhagyesh Kulakrni100% (2)
- Ds Micro Xpe 26 56 enDocument2 paginiDs Micro Xpe 26 56 enFlorin PătrulescuÎncă nu există evaluări
- 8536 Dbi Sala Uni 8 Oh BCR enDocument12 pagini8536 Dbi Sala Uni 8 Oh BCR enFlorin PătrulescuÎncă nu există evaluări
- Biologicals: Johannes Reich, Pierre Lang, Holger Grallert, Hubert MotschmannDocument6 paginiBiologicals: Johannes Reich, Pierre Lang, Holger Grallert, Hubert MotschmannFlorin PătrulescuÎncă nu există evaluări
- VeriCube Manual enDocument76 paginiVeriCube Manual enFlorin PătrulescuÎncă nu există evaluări
- Variables in Bottle Cap Torque Testing 20140408Document11 paginiVariables in Bottle Cap Torque Testing 20140408Florin PătrulescuÎncă nu există evaluări
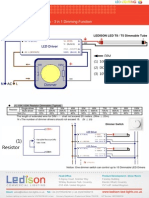
- T8/T5 Dimmable LED Tubes - 3 in 1 Dimming FunctionDocument2 paginiT8/T5 Dimmable LED Tubes - 3 in 1 Dimming FunctionFlorin PătrulescuÎncă nu există evaluări
- Pi Acryleze Ent Coat StabDocument2 paginiPi Acryleze Ent Coat StabFlorin PătrulescuÎncă nu există evaluări
- 1 Seminar Taiwan-1Document63 pagini1 Seminar Taiwan-1Florin PătrulescuÎncă nu există evaluări
- Headspace Oxygen Measurement in Vials and AmpoulesDocument4 paginiHeadspace Oxygen Measurement in Vials and AmpoulesGhanta Ranjith KumarÎncă nu există evaluări
- E UK Flexible BrochureDocument8 paginiE UK Flexible BrochureFlorin PătrulescuÎncă nu există evaluări
- Adresa SisDocument1 paginăAdresa SisFlorin PătrulescuÎncă nu există evaluări
- Double Platform Large Orbital: ShakersDocument1 paginăDouble Platform Large Orbital: ShakersFlorin PătrulescuÎncă nu există evaluări
- Brochures Isoflex enDocument8 paginiBrochures Isoflex enFlorin PătrulescuÎncă nu există evaluări
- 226-Article Text-601-1-10-20210702Document12 pagini226-Article Text-601-1-10-20210702Leni NopriyantiÎncă nu există evaluări
- 1 Ha Cabbages - May 2018 PDFDocument1 pagină1 Ha Cabbages - May 2018 PDFMwai EstherÎncă nu există evaluări
- Drone Survival GuideDocument2 paginiDrone Survival GuidevthiseasÎncă nu există evaluări
- Refraction Experiment-PekaDocument8 paginiRefraction Experiment-PekaA. Suhaimi100% (3)
- WEEK 11 - LAB 2 LEVEL 0 - BS Lab Electrical Supply - Domestic House Wiring & Accessories Including Lighting - DONEDocument6 paginiWEEK 11 - LAB 2 LEVEL 0 - BS Lab Electrical Supply - Domestic House Wiring & Accessories Including Lighting - DONEMuhd Alif MikhailÎncă nu există evaluări
- Prose 2 - Lost Spring - Important QADocument5 paginiProse 2 - Lost Spring - Important QADangerous GamingÎncă nu există evaluări
- Filled System Temperature Recorders & Recorder Controllers: SpecificationDocument2 paginiFilled System Temperature Recorders & Recorder Controllers: SpecificationdencryÎncă nu există evaluări
- Amy CuddyDocument5 paginiAmy CuddygeetaÎncă nu există evaluări
- Jesper Kyd - Flight Over Venice (Assassin's Creed II)Document9 paginiJesper Kyd - Flight Over Venice (Assassin's Creed II)Aldert de VriesÎncă nu există evaluări
- 5 Levels of Leadership AnswersDocument4 pagini5 Levels of Leadership Answersk98hk8wnnbÎncă nu există evaluări
- SK AccBro CI Update - FABIA - Unpriced - SEPT 2023 AW v4Document34 paginiSK AccBro CI Update - FABIA - Unpriced - SEPT 2023 AW v4Vlad TiurinÎncă nu există evaluări
- Daftar Ebook Tentang LeanDocument2 paginiDaftar Ebook Tentang LeanChilmar Buchari100% (1)
- Autodesk 3ds Max SkillsDocument18 paginiAutodesk 3ds Max SkillsJuan UrdanetaÎncă nu există evaluări
- Conversation Class - Video GamesDocument4 paginiConversation Class - Video GamesMaíra MouraÎncă nu există evaluări
- A 2Document3 paginiA 2John Kevin NocheÎncă nu există evaluări
- Pro Tester ManualDocument49 paginiPro Tester ManualRobson AlencarÎncă nu există evaluări
- Lecture Note On Photovoltaic CellDocument1 paginăLecture Note On Photovoltaic CellHaseeb NawazÎncă nu există evaluări
- Ipcrf Core Values 2019 - FinalDocument23 paginiIpcrf Core Values 2019 - FinalFrendelyn p. Gador100% (4)
- Vocabulary Levels Tests Versions 1 2Document12 paginiVocabulary Levels Tests Versions 1 2Rangsiya PjewÎncă nu există evaluări
- Technical Bulletin: ConditionDocument11 paginiTechnical Bulletin: ConditionFrancoÎncă nu există evaluări
- Manual of Armacad v9 PDFDocument102 paginiManual of Armacad v9 PDFCristiana FelicianoÎncă nu există evaluări
- EV METER - EV1 and EV3Document2 paginiEV METER - EV1 and EV3Nguyen DucÎncă nu există evaluări
- BITS Pilani: Scale Up and Post Approval ChangesDocument56 paginiBITS Pilani: Scale Up and Post Approval ChangesshrikantmsdÎncă nu există evaluări
- Bistable Relays RXMVB 2, RXMVB 4: FeaturesDocument4 paginiBistable Relays RXMVB 2, RXMVB 4: FeaturesGabriel Maxo PapagalloÎncă nu există evaluări
- Winter Student Enrichment PacketDocument9 paginiWinter Student Enrichment PacketshelleyallynÎncă nu există evaluări