Documente Academic
Documente Profesional
Documente Cultură
Initial Assessment of Respi. Emergency (PKGDI Medan)
Încărcat de
Novriefta NugrahaDrepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Initial Assessment of Respi. Emergency (PKGDI Medan)
Încărcat de
Novriefta NugrahaDrepturi de autor:
Formate disponibile
Initial Assessment
Respiratory Emergency In
Children And Its Management
Tatty Ermin Setiati
Diponegoro University
Dr. Kariadi Hospital Semarang
Introduction (1)
Respiratory disease Most frequent medical
emergency, need early intervention to decrease
mortality
Initial assessment is a very important to
differentiate upper or lower respiratory
emergency
Pediatric Assessment Triangle (PAT) an easy
and fast initial assessment to measure the severity
of the disease, and begin inflammatory treatment
Introduction (2)
Specific treatment for airway obstruction after
PAT and ABCDE assessment should be given
Positioning, suctioning, non-invasive and invasive
airway management, and pharmacologic
treatment (Nebulizer, Antibiotics)
Oxygen therapy according to the need
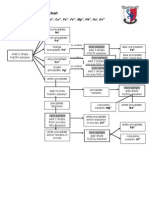
Initial Assessment
PAT Differentiate Respiratory Distress,
Respiratory Failure, and Respiratory Arrest
APPEARANCE
WORK OF
BREATHING
CIRCULATION
Conciousness
Core-Skin Temp. Different
Capillary refill
Warm or cool skin
Resp. Rate
Retraction
Initial Assessment
Pediatric Assessment Triangle :
Circulation to Skin
Appearance (Tickles = TICLS)
Tonus
Interactive ness
Consol ability
Look/Gaze
Speech/Cry
Work of Breathings
Abnormal airway sounds
Abnormal positioning
Retractions
Nasal flaring
Characteristic of Circulation to Skin
Pallor
Mottling
Cyanosis
Capillary Refill Time >
Circulation to Skin
Normal capillary refill is < 2 seconds in a warm environment
Circulation to Skin
PAT : Potential Respiratory Failure
Normal
Increased
Normal
Circulation to Skin
PAT : Respiratory Failure
Abnormal
Increased
or
decreased
Normal or abnormal
Rate
Effort / mechanics
Air entry
Skin color and temperature
Rapid Cardiopulmonary Assessment
Physical Examination Breathing
Respiratory Rate
In non-critical : RR determine by sitting the child
in his caregivers lap and exposing his chest
RR may be affected by level of activity, fever,
anxiety, and metabolic state
RR > 60x / minute abnormal in any age
RR < 20x / minute in a sick child < 6 years and <
15x / minute in a sick child 7-14 years RF
Air Movement and
Abnormal Lung Sound
Stethoscope at the mid axillary line clinical
estimation of tidal volume (a volume of air
exchanged with each breath)
Abnormal breath sound (stridor, wheezing,
expiratory grunting, inspiratory crackles, absent
breath sounds despite WOB)
Causes of Poor Air
Movement in Children
Obstruction of airways : Asthma, Bronchiolitis,
Croups
Restriction of chest wall movement : Chest wall
injury, severe scoliosis
Chest wall muscle fatigue : WOB, Muscular
dystrophy
Decreased central respiratory drive : Head injury
Chest injury : Rib fractures, pneumothorax
Oxygen Saturation (SaO2)
Pulse oxymetry excellent tool for assessing a
childs breathing
SaO2 > 94% oxygenation probably good
SaO2 < 90% in a child on 100% oxygen NR mask
need assisted ventilation
Interpret SaO2 together with WOB
Circulation Heart Rate
Tachycardia Early sign of hypoxia or low
perfusion, but may also caused by : fever, anxiety,
pain, excitement
A trend of increasing or decreasing HR
worsening hypoxia or shock or improvement after
treatment
Bradycardia critical hypoxia and or ischemia
Circulation Pulse quality
Normally the brachial pulse is palpable inside or
medial to the biceps (weak / strong) if strong
probably not hypotensive
If peripheral pulse not palpated, check the central
pulse (femoral / carotid)
Absent of a central pulse CPR
Skin Temperature
Capillary Refill Time
The child skin warm near the wrists and ankles -
good perfusion
Decreasing perfusion the line of separation
from cool to warm advances up the limb
Capillary refill time (N 2-3 seconds), affected by
environmental factors cool room temp
Circulation to the skin (skin temp., capillary refill
time, pulse quality) assessment circulatory
status
Rapid Cardiopulmonary Assessment
Physical Examination : Breathing
Respiratory Arrest
Absence of effective breathing
If ventilation and oxygenation are not adequately
support Cardio respiratory Arrest a low
probability of survival
General Non-invasive
Treatment Positioning
Patient position of comfort Severe upper
airway obstruction may get into sniffing position
Severe lower airway obstruction Tripod posture
Infants and Toddlers caregivers arms or lap
The sniffing position
The abnormal tripod position
Retractions
Oxygen
Treatment with High flow O2 safe
Give oxygen to any child with clinical signs of
cardiopulmonary distress, or with a history
suggesting possible abnormalities in gas exchange
When treating children, it is better to overuse
oxygen than to underused it
Management of Respiratory Failure
Initially treat with general noninvasive measures
Upper or lower airway obstruction specific
treatment
Altered level of consciousness and signs of or
WOB (flaring, grunting, gasping, apnea, cyanosis)
and or SaO2 < 90% on 100% NR O2 mask
Assisted Ventilation or PPV with BVM
ventilation or ET intubation
Placement of OG or NG tube (relieve gastric
distension and improve ventilation)
BVM Ventilation
The best technique for providing oxygenation and
ventilation during resuscitation and transport
60-95% O2 can be given effectively and safely by
choosing a well-fitted mask, connecting with O2
reservoir to an oxygen source at 15L/ minute
How To Use
Resuscitation Mask
Possible Complications
BVM Ventilation
Hypoxia
Barotraumas
Gastric Distension
Emesis and Aspiration
Endotracheal Intubation (ETT)
Potential Advantages : Definitive Airway Control,
Decrease Risk of Aspiration, Ease of assisted
ventilation
Potential Complications : Transient hypoxia,
hypercarbia (due to prolonged intubation
attempts), elevation if intracranial pressure,
mechanical trauma of the airway, misplacement
of the tube (intrabronchial / esophageal
intubation)
DOPE
Intubated patient fail to respond (improve color,
SaO2, HR, and appearance)
Dislodgment Extubate, BVM, Reintubate
Obstruction Suction, Extubate, BVM,
Reintubate
Pneumothorax Needle thoracocentesis
Equipment Check equipment patient-to-tank
Specific Treatment
For Respiratory Distress
Determine upper or lower airway obstruction
Snoring or stridor upper airway obstruction
Wheezing lower airway obstruction
Upper airway obstruction due the tounge and
mandible falling back/ partially blocking the
pharynx head tilt / chin-lift or jaw trust
Maintenance of adequate airway: Placement of an
oropharyngeal airway, nasopharyngeal or ETT
Croup
A viral disease with inflammation, edema,
narrowing of the larynx, trachea, and bronchioles
Affects infants and toddlers
Cold symptoms several days followed by the
development of a barking cough, stridor, various
level of respiratory distress
Fever and symptoms are worse at night
Croup Treatment
Cool mist (humidified oxygen or nebulized
saline)
Cool water vapor reduced the inflammation and
obstruction
Pharmacologic treatment: Nebulized epinephrine
(stridor, WOB, poor air movement, SaO2 <
94%, altered appearance (need observation in
ED for 4 6 hours)
Croup Assisted Ventilation
Rare case
Invasive airway management : ETT in a case that
does not respond to BVM ventilation
Choosing ETT one or two sizes smaller than
normal for age or length (inflammation of the
trachea at the subglottic level)
Bacterial Upper Airway Infections
Usually > 12 months
Appears ill, Toxic, Pain on swallowing, Stridor
may be present, no barking cough
Examples: Epiglotitis ( H. Influenzae), Tracheitis,
Diphtheria, Peritonsillar Abcess, Retropharyngeal
Abcess
Treatment : General noninvasive dgn high flow
oxygen and position of comfort. In RF give BVM
consider ETT
Lower Airway Obstruction
(Bronchiolitis)
Bronchiolitis viral lower respiratory infection,
usually in children < 3 years caused by RSV
Destruction lining of the bronchioles, profuse
secretions, bronchoconstriction
Assessment shows variable degrees of WOB,
tachypnea, diffuse wheezing, insp. Crackles,
tachycardia
Predictors of RF in
Suspected Bronchiolitis
RR > 60x / minute with WOB
RR < 20x / minute with WOB
HR > 200x / minute or < 100x / minute
Poor appearance
SaO2 < 90% on supplemental O2
Asthma
Asthma is a disease of small airway inflammation
leads to bronchoconstriction, mucosal edema, and
profuse secretions
Severe airway obstruction and V/Q mismatch
Clinically Different degrees of tachypnea,
tachycardia, WOB, wheezing on exhalation,
SaO2 normal or low
Asthma with RF
Altered appearance
Exhaustion
Inability to recline
Interrupted speech
Severe retraction
Decreased Air Movement
Management
Lower Respiratory Obstruction
General noninvasive treatment with high flow O2
therapy
Nebulized Bronchodilators
In asthma : Assisted Ventilation PPV required
very high insp. Pressure may caused
pneumothorax / pneumomediastinum
BVM ventilation or ETT If RF and failed to
respond to high flow O2 and maximal
bronchodilator therapy
Summary (1)
The PAT is a good tool for determining the
effectiveness of gas exchange
The PAT also identify the critical child in RF who
requires immediate assisted ventilation
Obtaining RR, listening for air movement, and
SaO2 in concert with PAT
An initial assessment allow an evaluation of
severity and urgency for treatment, establish
specific treatment for upper / lower airway
obstruction
Summary (2)
Specific treatment for croup cool mist and
nebulized epinephrine
If RF occurred begin with assisted ventilation
with BVM at an age-appropriate rate
Add spesific treatment for airway obstructed if
indicated
Performed ETT, and be alert for DOPE in the
intubated child who suddenly worsens / fails to
respond
S-ar putea să vă placă și
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Diabetes Dengan Xanthoma KulitDocument2 paginiDiabetes Dengan Xanthoma KulitNovriefta NugrahaÎncă nu există evaluări
- Embryology&TeratologyDocument43 paginiEmbryology&TeratologyNovriefta NugrahaÎncă nu există evaluări
- Islamic MedicineDocument16 paginiIslamic MedicineNovriefta NugrahaÎncă nu există evaluări
- Journal of XanthomaDocument5 paginiJournal of XanthomaNovriefta NugrahaÎncă nu există evaluări
- Tugas Journal ReadingDocument34 paginiTugas Journal ReadingNovriefta NugrahaÎncă nu există evaluări
- Pediatrics 2004 Garcia Peña 24 8Document7 paginiPediatrics 2004 Garcia Peña 24 8Novriefta NugrahaÎncă nu există evaluări
- Dengue Guideline DengueDocument33 paginiDengue Guideline DenguedrkkdbÎncă nu există evaluări
- Newcastle OttawaDocument3 paginiNewcastle OttawaNovriefta NugrahaÎncă nu există evaluări
- 05 Nose AnatomyDocument28 pagini05 Nose AnatomyNovriefta NugrahaÎncă nu există evaluări
- Results of Case-Control Studies Support Association Between Contact Lens Use andDocument17 paginiResults of Case-Control Studies Support Association Between Contact Lens Use andNovriefta NugrahaÎncă nu există evaluări
- Respiratory EmergenciesDocument30 paginiRespiratory EmergenciesNovriefta NugrahaÎncă nu există evaluări
- Journal of Ultrasonography in Acute AppendisitisDocument7 paginiJournal of Ultrasonography in Acute AppendisitisNovriefta NugrahaÎncă nu există evaluări
- COPD, Asthma, and DM Risk FactorDocument13 paginiCOPD, Asthma, and DM Risk FactorNovriefta NugrahaÎncă nu există evaluări
- Ankle Brachial Pressure IndexDocument12 paginiAnkle Brachial Pressure IndexNovriefta NugrahaÎncă nu există evaluări
- ARITMIA, Gangguan Irama JantungDocument37 paginiARITMIA, Gangguan Irama JantungNovriefta NugrahaÎncă nu există evaluări
- Handbook of Pathology and Pathophysiology of Cardiovascular Disease 2002 PDFDocument321 paginiHandbook of Pathology and Pathophysiology of Cardiovascular Disease 2002 PDFChavo Delocho100% (1)
- WHO - Surgical Care at The District Hospital (WHO 2003)Document514 paginiWHO - Surgical Care at The District Hospital (WHO 2003)gekriaÎncă nu există evaluări
- Terminology of The Tonsils: 2011 Blackwell Verlag GMBH - Anat. Histol. Embryol. 40 (2011) 204-209Document7 paginiTerminology of The Tonsils: 2011 Blackwell Verlag GMBH - Anat. Histol. Embryol. 40 (2011) 204-209Novriefta NugrahaÎncă nu există evaluări
- 05 Nose AnatomyDocument28 pagini05 Nose AnatomyNovriefta NugrahaÎncă nu există evaluări
- Atypical Bacteria in Adenoids and Tonsils of Children Requiring AdenotonsillectomyDocument7 paginiAtypical Bacteria in Adenoids and Tonsils of Children Requiring AdenotonsillectomyNovriefta NugrahaÎncă nu există evaluări
- Allergic Rhinitis 2Document4 paginiAllergic Rhinitis 2Novriefta NugrahaÎncă nu există evaluări
- 05 Nose AnatomyDocument28 pagini05 Nose AnatomyNovriefta NugrahaÎncă nu există evaluări
- Vertigo PeriferDocument76 paginiVertigo PeriferAstriana IndrawatiÎncă nu există evaluări
- UPLOAD KE-1 HormDocument47 paginiUPLOAD KE-1 HormNovriefta NugrahaÎncă nu există evaluări
- Photo Quiz: Enlarged Tonsils and FatigueDocument3 paginiPhoto Quiz: Enlarged Tonsils and FatigueNovriefta NugrahaÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Plant Based Plan White PaperDocument24 paginiPlant Based Plan White PaperSara AdemovicÎncă nu există evaluări
- Bellows and Expansion JointsDocument5 paginiBellows and Expansion JointsSuresh MechÎncă nu există evaluări
- Artifact 7 - Superannuation Pension Calculator-GuidelinesDocument2 paginiArtifact 7 - Superannuation Pension Calculator-GuidelinesSai RamÎncă nu există evaluări
- Healing and Keeping Prayer (2013)Document2 paginiHealing and Keeping Prayer (2013)Kylie DanielsÎncă nu există evaluări
- 1101259L 580.752830 Pressure Washer ManualDocument64 pagini1101259L 580.752830 Pressure Washer Manualgork1roguesÎncă nu există evaluări
- Herbs and SpicesDocument77 paginiHerbs and SpicesNicole RicohermosoÎncă nu există evaluări
- Vocabulary June v22Document2 paginiVocabulary June v22Wiston TonwisÎncă nu există evaluări
- Cocktail Making Techniques 13.3.11Document3 paginiCocktail Making Techniques 13.3.11Ryan MenezesÎncă nu există evaluări
- Jokes and Their Relation To The Unconscious: Laurence HenkelmanDocument3 paginiJokes and Their Relation To The Unconscious: Laurence HenkelmanMilos VisnjicÎncă nu există evaluări
- Chinese Cinderella - MeDocument2 paginiChinese Cinderella - Meapi-298120057100% (1)
- Argumentative EssayDocument5 paginiArgumentative EssayJoshua MontoyaÎncă nu există evaluări
- Weaning Guidelines 2007Document4 paginiWeaning Guidelines 2007deliejoyceÎncă nu există evaluări
- Clinical Algorithms in General Surgery PDFDocument786 paginiClinical Algorithms in General Surgery PDFLaura Campaña100% (5)
- POFL Unit 1 Status QUO pp.1-37Document38 paginiPOFL Unit 1 Status QUO pp.1-37AruÎncă nu există evaluări
- Kmartinez Draft Research PaperDocument14 paginiKmartinez Draft Research Paperapi-273007806Încă nu există evaluări
- English 10-1 Personal Response EssayDocument2 paginiEnglish 10-1 Personal Response Essayapi-467840192Încă nu există evaluări
- ISKCON Desire Tree - Brahma Vimohana LeelaDocument34 paginiISKCON Desire Tree - Brahma Vimohana LeelaISKCON desire treeÎncă nu există evaluări
- Main Group Oganometallics: Shriver and Atkins, Chapter 15Document24 paginiMain Group Oganometallics: Shriver and Atkins, Chapter 15José Augusto VillarÎncă nu există evaluări
- Expository Cause and Effect OUTLINEDocument2 paginiExpository Cause and Effect OUTLINEAutoDefenceÎncă nu există evaluări
- 8-Critical Appraisal of An ArticleDocument20 pagini8-Critical Appraisal of An ArticleMohmmed Abu MahadyÎncă nu există evaluări
- Pipe Thickness CalculationDocument4 paginiPipe Thickness CalculationHarryÎncă nu există evaluări
- DICGC - For Depositors - A Guide To Deposit InsuranceDocument10 paginiDICGC - For Depositors - A Guide To Deposit InsuranceSachinÎncă nu există evaluări
- Major Head of AccountsDocument9 paginiMajor Head of AccountsArun EmmiÎncă nu există evaluări
- Vice President Quality Operations in Greater Chicago IL Resume Kevin FredrichDocument2 paginiVice President Quality Operations in Greater Chicago IL Resume Kevin FredrichKevin Fredrich1Încă nu există evaluări
- Enzymes in Grain ProcessingDocument1 paginăEnzymes in Grain ProcessingAttila-Levente FogarasiÎncă nu există evaluări
- Testing For Cations Flow ChartDocument2 paginiTesting For Cations Flow Chartapi-252561013Încă nu există evaluări
- EVK203/EVK213/EVK223/EVK233/EVK253: Digital Thermostats For Ventilated Refrigerating UnitsDocument2 paginiEVK203/EVK213/EVK223/EVK233/EVK253: Digital Thermostats For Ventilated Refrigerating UnitsMihai BordeianuÎncă nu există evaluări
- 9 SolutionsDocument31 pagini9 SolutionsLaurertan TavaresÎncă nu există evaluări
- Polycystic Ovary Syndrome (PCOS) - Symptoms, Causes, and TreatmentDocument19 paginiPolycystic Ovary Syndrome (PCOS) - Symptoms, Causes, and TreatmentAkshay HarekarÎncă nu există evaluări
- Modelling The Effects of Condensate Banking On High CGR ReservoirsDocument11 paginiModelling The Effects of Condensate Banking On High CGR ReservoirslikpataÎncă nu există evaluări