Documente Academic
Documente Profesional
Documente Cultură
GOLD Spirometry 2010 CorxFeb11
Încărcat de
samuel_rumende38950 evaluări0% au considerat acest document util (0 voturi)
33 vizualizări59 paginiSpirometry is a method of assessing lung function by measuring the total volume of air the patient can expel from the lungs after a maximal inhalation. Underuse leads to inaccurate COPD diagnosis Widespread uptake has been limited by: - Concerns over technical performance of operators - Difficulty with interpretation of results - Lack of approved local training courses.
Descriere originală:
Titlu original
GOLD Spirometry 2010 CorxFeb11(22)
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PPT, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentSpirometry is a method of assessing lung function by measuring the total volume of air the patient can expel from the lungs after a maximal inhalation. Underuse leads to inaccurate COPD diagnosis Widespread uptake has been limited by: - Concerns over technical performance of operators - Difficulty with interpretation of results - Lack of approved local training courses.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPT, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
33 vizualizări59 paginiGOLD Spirometry 2010 CorxFeb11
Încărcat de
samuel_rumende3895Spirometry is a method of assessing lung function by measuring the total volume of air the patient can expel from the lungs after a maximal inhalation. Underuse leads to inaccurate COPD diagnosis Widespread uptake has been limited by: - Concerns over technical performance of operators - Difficulty with interpretation of results - Lack of approved local training courses.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPT, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 59
Spirometry in Primary Care
Global Initiative for Chronic Obstructive
Lung Disease (GOLD) 2010
Spirometry - Introduction
Spirometry is the gold standard for COPD
diagnosis
Underuse leads to inaccurate COPD diagnosis
Widespread uptake has been limited by:
Concerns over technical performance of
operators
Difficulty with interpretation of results
Lack of approved local training courses
Lack of evidence showing clear benefit when
spirometry is incorporated into management
What is Spirometry?
Spirometry is a method of
assessing lung function by
measuring the total volume of
air the patient can expel from
the lungs after a maximal
inhalation.
Why Perform Spirometry?
Measure airflow obstruction to help make a
definitive diagnosis of COPD
Confirm presence of airway obstruction
Assess severity of airflow obstruction in COPD
Detect airflow obstruction in smokers who may
have few or no symptoms
Monitor disease progression in COPD
Assess one aspect of response to therapy
Assess prognosis (FEV
1
) in COPD
Perform pre-operative assessment
Spirometry Additional Uses
Make a diagnosis and assess severity in a
range of other respiratory conditions
Distinguish between obstruction and
restriction as causes of breathlessness
Screen workforces in occupational
environments
Assess fitness to dive
Perform pre-employment screening in certain
professions
Types of Spirometers
Bellows spirometers:
Measure volume; mainly in lung
function units
Electronic desk top spirometers:
Measure flow and volume with real
time display
Small hand-held spirometers:
Inexpensive and quick to use but no
print out
Volume Measuring Spirometer
Flow Measuring Spirometer
Desktop Electronic Spirometers
Small Hand-held Spirometers
Standard Spirometric Indicies
FEV
1
- Forced expiratory volume in one second:
The volume of air expired in the first second of
the blow
FVC - Forced vital capacity:
The total volume of air that can be forcibly
exhaled in one breath
FEV
1
/FVC ratio:
The fraction of air exhaled in the first second
relative to the total volume exhaled
Additional Spirometric Indicies
VC - Vital capacity:
A volume of a full breath exhaled in the patients
own time and not forced. Often slightly greater
than the FVC, particularly in COPD
FEV
6
Forced expired volume in six seconds:
Often approximates the FVC. Easier to perform
in older and COPD patients but role in COPD
diagnosis remains under investigation
MEFR Mid-expiratory flow rates:
Derived from the mid portion of the flow volume
curve but is not useful for COPD diagnosis
Total
lung
capacity
Tidal volume
Inspiratory reserve
volume
Expiratory reserve
volume
Residual volume
Inspiratory
capacity
Vital
capacity
Lung Volume Terminology
Spirogram Patterns
Normal
Obstructive
Restrictive
Mixed Obstructive and Restrictive
Spirometry
Predicted Normal
Values
Predicted Normal Values
Age
Height
Sex
Ethnic Origin
Affected by:
Criteria for Normal
Post-bronchodilator Spirometry
FEV
1
: % predicted > 80%
FVC: % predicted > 80%
FEV
1
/FVC: > 0.7 - 0.8, depending
on age
Normal Trace Showing FEV
1
and FVC
1 2 3 4 5 6
1
2
3
4
V
o
l
u
m
e
,
l
i
t
e
r
s
Time, sec
FVC
5
1
FEV
1
= 4L
FVC = 5L
FEV
1
/FVC = 0.8
SPIROMETRY
OBSTRUCTIVE
DISEASE
Spirometry: Obstructive Disease
V
o
l
u
m
e
,
l
i
t
e
r
s
Time, seconds
5
4
3
2
1
1 2 3 4 5 6
FEV
1
= 1.8L
FVC = 3.2L
FEV
1
/FVC = 0.56
Normal
Obstructive
Spirometric Diagnosis of COPD
COPD is confirmed by post
bronchodilator FEV
1
/FVC < 0.7
Post-bronchodilator FEV
1
/FVC
measured 15 minutes after 400g
salbutamol or equivalent
Bronchodilator Reversibility Testing
Provides the best achievable FEV
1
(and FVC)
Helps to differentiate COPD from
asthma
Must be interpreted with clinical
history - neither asthma nor COPD
are diagnosed on spirometry alone
Bronchodilator Reversibility Testing
Can be done on first visit if no diagnosis has
been made
Best done as a planned procedure: pre-
and post-bronchodilator tests require a
minimum of 15 minutes
Post-bronchodilator only saves time but does
not help confirm if asthma is present
Short-acting bronchodilators need to be
withheld for at least 4 hours prior to test
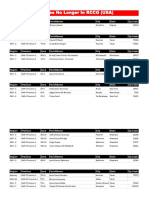
Bronchodilator Reversibility Testing
Bronchodilator*
Dose FEV
1
before
and after
Salbutamol
200 400 g via large
volume spacer
15 minutes
Terbutaline
500 g via Turbohaler 15 minutes
Ipratropium
160 g** via spacer
45 minutes
* Some guidelines suggest nebulised bronchodilators can be given but the doses
are not standardised. There is no consensus on the drug, dose or mode of
administering a bronchodilator in the laboratory. Ref: ATS/ERS Task Force :
Interpretive strategies for Lung Function Tests ERJ 2005;26:948
** Usually 8 puffs of 20 g
Figure 5.1-6.
Bronchodilator
Reversibility
Testing in COPD
GOLD
Report (2009)
Figure 5.1-6. Bronchodilator
Reversibility Testing in COPD
Preparation
Tests should be performed when patients are
clinically stable and free from respiratory infection
Patients should not have taken:
inhaled short-acting bronchodilators in the
previous six hours
long-acting bronchodilator in the previous 12
hours
sustained-release theophylline in the previous
24 hours
Figure 5.1-6. Bronchodilator
Reversibility Testing in COPD
Spirometry
FEV
1
should be measured (minimum twice, within
5% or 150mls) before a bronchodilator is given
The bronchodilator should be given by metered dose
inhaler through a spacer device or by nebulizer to be
certain it has been inhaled
The bronchodilator dose should be selected to be
high on the dose/response curve
(..continued)
Figure 5.1-6. Bronchodilator
Reversibility Testing in COPD
Spirometry (continued)
Possible dosage protocols:
400 g
2
-agonist, or
80-160 g anticholinergic, or
the two combined
FEV
1
should be measured again:
15 minutes after a short-acting bronchodilator
45 minutes after the combination
Figure 5.1-6. Bronchodilator
Reversibility Testing in COPD
Results
An increase in FEV
1
that is both greater
than 200 ml and 12% above the pre-
bronchodilator FEV
1
(baseline value) is
considered significant
It is usually helpful to report the absolute
change (in ml) as well as the % change
from baseline to set the improvement in a
clinical context
SPIROMETRY
RESTRICTIVE
DISEASE
Criteria: Restrictive Disease
FEV
1:
normal or mildly reduced
FVC: < 80% predicted
FEV
1
/FVC: > 0.7
V
o
l
u
m
e
,
l
i
t
e
r
s
Time, seconds
FEV
1
= 1.9L
FVC = 2.0L
FEV
1
/FVC = 0.95
1 2 3 4 5 6
5
4
3
2
1
Spirometry: Restrictive Disease
Normal
Restrictive
Mixed Obstructive/Restrictive
FEV
1
: < 80% predicted
FVC: < 80% predicted
FEV
1
/FVC: < 0.7
Mixed Obstructive and Restrictive
V
o
l
u
m
e
,
l
i
t
e
r
s
Time, seconds
Restrictive and mixed obstructive-restrictive are difficult to diagnose by
spirometry alone; full respiratory function tests are usually required
(e.g., body plethysmography, etc)
FEV
1
= 0.5L
FVC = 1.5L
FEV
1
/FVC = 0.30
Normal
Obstructive - Restrictive
SPIROMETRY
Flow Volume
Flow Volume Curve
Standard on most desk-top spirometers
Adds more information than volume
time curve
Less understood but not too difficult to
interpret
Better at demonstrating mild airflow
obstruction
Flow Volume Curve
Expiratory
flow rate
L/sec
Volume (L)
FVC
Maximum
expiratory flow
(PEF)
Inspiratory
flow rate
L/sec
RV
TLC
Flow Volume Curve Patterns
Obstructive and Restrictive
Obstructive Severe obstructive Restrictive
Volume (L)
E
x
p
i
r
a
t
o
r
y
f
l
o
w
r
a
t
e
E
x
p
i
r
a
t
o
r
y
f
l
o
w
r
a
t
e
E
x
p
i
r
a
t
o
r
y
f
l
o
w
r
a
t
e
Volume (L) Volume (L)
Steeple pattern,
reduced peak flow,
rapid fall off
Normal shape,
normal peak flow,
reduced volume
Reduced peak flow,
scooped out mid-
curve
Obstructive Restrictive Mixed
Time Time
Time
V
o
l
u
m
e
V
o
l
u
m
e
V
o
l
u
m
e
Spirometry: Abnormal Patterns
Slow rise, reduced
volume expired;
prolonged time to
full expiration
Fast rise to plateau
at reduced
maximum volume
Slow rise to reduced
maximum volume;
measure static lung
volumes and full PFTs
to confirm
PRACTICAL SESSION
Performing Spirometry
Spirometry Training
Training is essential for operators to learn correct
performance and interpretation of results
Training for competent performance of spirometry
requires a minimum of 3 hours
Acquiring good spirometry performance and
interpretation skills requires practice, evaluation,
and review
Spirometry performance (who, when and where)
should be adapted to local needs and resources
Training for spirometry should be evaluated
Obtaining Predicted Values
Independent of the type of spirometer
Choose values that best represent the
tested population
Check for appropriateness if built into
the spirometer
Optimally, subjects should rest 10 minutes
before performing spirometry
Withholding Medications
Before performing spirometry, withhold:
Short acting
2
-agonists for 6 hours
Long acting
2
-agonists for 12 hours
Ipratropium for 6 hours
Tiotropium for 24 hours
Optimally, subjects should avoid caffeine and
cigarette smoking for 30 minutes before
performing spirometry
Performing Spirometry - Preparation
1. Explain the purpose of the test and
demonstrate the procedure
2. Record the patients age, height and
gender and enter on the spirometer
3. Note when bronchodilator was last used
4. Have the patient sitting comfortably
5. Loosen any tight clothing
6. Empty the bladder beforehand if needed
Performing Spirometry
Breath in until the lungs are full
Hold the breath and seal the lips
tightly around a clean mouthpiece
Blast the air out as forcibly and fast as
possible. Provide lots of
encouragement!
Continue blowing until the lungs feel
empty
Watch the patient during the blow to
assure the lips are sealed around the
mouthpiece
Check to determine if an adequate
trace has been achieved
Repeat the procedure at least twice
more until ideally 3 readings within 100
ml or 5% of each other are obtained
Performing Spirometry
Three times FVC within 5% or 0.15 litre (150 ml)
Reproducibility - Quality of Results
V
o
l
u
m
e
,
l
i
t
e
r
s
Time, seconds
Spirometry - Possible Side Effects
Feeling light-headed
Headache
Getting red in the face
Fainting: reduced venous return or
vasovagal attack (reflex)
Transient urinary incontinence
Spirometry should be avoided after
recent heart attack or stroke
Spirometry - Quality Control
Most common cause of inconsistent
readings is poor patient technique
Sub-optimal inspiration
Sub-maximal expiratory effort
Delay in forced expiration
Shortened expiratory time
Air leak around the mouthpiece
Subjects must be observed and encouraged
throughout the procedure
Spirometry Common Problems
Inadequate or incomplete blow
Lack of blast effort during exhalation
Slow start to maximal effort
Lips not sealed around mouthpiece
Coughing during the blow
Extra breath during the blow
Glottic closure or obstruction of mouthpiece
by tongue or teeth
Poor posture leaning forwards
Equipment Maintenance
Most spirometers need regular calibration to
check accuracy
Calibration is normally performed with a 3 litre
syringe
Some electronic spirometers do not require
daily/weekly calibration
Good equipment cleanliness and anti-infection
control are important; check instruction manual
Spirometers should be regularly serviced; check
manufacturers recommendations
Troubleshooting
Examples - Unacceptable Traces
Unacceptable Trace - Poor Effort
V
o
l
u
m
e
,
l
i
t
e
r
s
Time, seconds
May be accompanied by a slow start
Inadequate sustaining of effort
Variable expiratory effort
Normal
V
o
l
u
m
e
,
l
i
t
e
r
s
Time, seconds
Unacceptable Trace Stop Early
Normal
V
o
l
u
m
e
,
l
i
t
e
r
s
Time, seconds
Unacceptable Trace Slow Start
Normal
V
o
l
u
m
e
,
l
i
t
e
r
s
Time, seconds
Unacceptable Trace - Coughing
Normal
V
o
l
u
m
e
,
l
i
t
e
r
s
Time, seconds
Unacceptable Trace Extra Breath
Normal
Some Spirometry Resources
Global Initiative for Chronic Obstructive Lung
Disease (GOLD) - www.goldcopd.org
Spirometry in Practice - www.brit-thoracic.org.uk
ATS-ERS Taskforce: Standardization of
Spirometry. ERJ 2005;29:319-338
www.thoracic.org/sections/publications/statements
National Asthma Council: Spirometry Handbook
www.nationalasthma.org.au
S-ar putea să vă placă și
- Surat Keterangan Bekerja Untuk Visa SchengenDocument1 paginăSurat Keterangan Bekerja Untuk Visa Schengensamuel_rumende3895Încă nu există evaluări
- Surat Keterangan Bekerja Untuk Visa SchengenDocument1 paginăSurat Keterangan Bekerja Untuk Visa Schengensamuel_rumende3895Încă nu există evaluări
- Brother Solutions CenterDocument1 paginăBrother Solutions Centersamuel_rumende3895Încă nu există evaluări
- Brother Solutions CenterDocument1 paginăBrother Solutions Centersamuel_rumende3895Încă nu există evaluări
- Asthma (Chest 2012)Document39 paginiAsthma (Chest 2012)samuel_rumende3895Încă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (120)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Churches That Have Left RCCG 0722 PDFDocument2 paginiChurches That Have Left RCCG 0722 PDFKadiri JohnÎncă nu există evaluări
- 40+ Cool Good Vibes MessagesDocument10 pagini40+ Cool Good Vibes MessagesRomeo Dela CruzÎncă nu există evaluări
- Rele A Gas BuchholtsDocument18 paginiRele A Gas BuchholtsMarco GiraldoÎncă nu există evaluări
- PHD Thesis - Table of ContentsDocument13 paginiPHD Thesis - Table of ContentsDr Amit Rangnekar100% (15)
- Multi Grade-ReportDocument19 paginiMulti Grade-Reportjoy pamorÎncă nu există evaluări
- Wonderland Audition PacketDocument5 paginiWonderland Audition PacketBritt Boyd100% (1)
- Pre T&C Checklist (3 Language) - Updated - 2022 DavidDocument1 paginăPre T&C Checklist (3 Language) - Updated - 2022 Davidmuhammad farisÎncă nu există evaluări
- Wwe SVR 2006 07 08 09 10 11 IdsDocument10 paginiWwe SVR 2006 07 08 09 10 11 IdsAXELL ENRIQUE CLAUDIO MENDIETAÎncă nu există evaluări
- Impact Grammar Book Foundation Unit 1Document3 paginiImpact Grammar Book Foundation Unit 1Domingo Juan de LeónÎncă nu există evaluări
- Alcatraz Analysis (With Explanations)Document16 paginiAlcatraz Analysis (With Explanations)Raul Dolo Quinones100% (1)
- Sayyid DynastyDocument19 paginiSayyid DynastyAdnanÎncă nu există evaluări
- Samsung LE26A457Document64 paginiSamsung LE26A457logik.huÎncă nu există evaluări
- DLP No. 10 - Literary and Academic WritingDocument2 paginiDLP No. 10 - Literary and Academic WritingPam Lordan83% (12)
- 360-Degree FeedbackDocument24 pagini360-Degree Feedbackanhquanpc100% (1)
- Conceptual Diagram of Ways To Increase SalesDocument1 paginăConceptual Diagram of Ways To Increase SalesO6U Pharmacy RecordingsÎncă nu există evaluări
- Charles P. Jones, Investments: Analysis and Management, Eleventh Edition, John Wiley & SonsDocument20 paginiCharles P. Jones, Investments: Analysis and Management, Eleventh Edition, John Wiley & SonsRizki AuliaÎncă nu există evaluări
- Thomas Noochan Pokemon Review Final DraftDocument6 paginiThomas Noochan Pokemon Review Final Draftapi-608717016Încă nu există evaluări
- Q & A Set 2 PDFDocument18 paginiQ & A Set 2 PDFBharathiraja MoorthyÎncă nu există evaluări
- Field Assignment On Feacal Sludge ManagementDocument10 paginiField Assignment On Feacal Sludge ManagementSarah NamyaloÎncă nu există evaluări
- LM213 First Exam Notes PDFDocument7 paginiLM213 First Exam Notes PDFNikki KatesÎncă nu există evaluări
- Science Project FOLIO About Density KSSM Form 1Document22 paginiScience Project FOLIO About Density KSSM Form 1SarveesshÎncă nu există evaluări
- 1986 Elektric M InfoDocument1 pagină1986 Elektric M InfoDanielDiasÎncă nu există evaluări
- Narrative ReportDocument6 paginiNarrative ReportAlyssa Marie AsuncionÎncă nu există evaluări
- Conductivity MeterDocument59 paginiConductivity MeterMuhammad AzeemÎncă nu există evaluări
- Apple Festival Program 2017Document3 paginiApple Festival Program 2017Elizabeth JanneyÎncă nu există evaluări
- Discrete Probability Distribution UpdatedDocument44 paginiDiscrete Probability Distribution UpdatedWaylonÎncă nu există evaluări
- Rebecca Young Vs CADocument3 paginiRebecca Young Vs CAJay RibsÎncă nu există evaluări
- Ruahsur Vangin Basket-Ball Court Lungrem ChimDocument4 paginiRuahsur Vangin Basket-Ball Court Lungrem ChimchanmariansÎncă nu există evaluări
- Ain Tsila Development Main EPC Contract A-CNT-CON-000-00282: Visual Inspection Test Procedure B-QAC-PRO-210-39162Document14 paginiAin Tsila Development Main EPC Contract A-CNT-CON-000-00282: Visual Inspection Test Procedure B-QAC-PRO-210-39162ZaidiÎncă nu există evaluări
- K3VG Spare Parts ListDocument1 paginăK3VG Spare Parts ListMohammed AlryaniÎncă nu există evaluări