Documente Academic
Documente Profesional
Documente Cultură
Erytrasma
Încărcat de
Andrean LinataDescriere originală:
Titlu original
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Erytrasma
Încărcat de
Andrean LinataDrepturi de autor:
Formate disponibile
ERYTHRASMA
DERMATOVENEROLOGY DEPARTMENT
MEDICAL FACULTY UKRIDA UNIVERSITY
KUDUS, 1-9-2014
Supervisor:
INTRODUCTION
Definition:
Erythrasma is a common superficial bacterial
infection of the skin characterized by well-difened but
irregular reddish brown patches, occuring in the
intertriginous areas, or by fissuring and white maceration in
the toe clefts.
EPIDEMIOLOGY
1. The incidence of erythrasma is reported to be around 4%
2. The widespread form is found more frequently in the
subtropical and tropical areas
3. The incidence of erythrasma increases with age
and higher in black people
4. Men and women are equally affected; the crural
form is more common in men and the interdigital form
is more common in women (83% of 24 patients).
ETIOLOGY
The incriminated organism is Corynebacterium minutissimum,
which usually is present as a normal human skin inhabitant.
Prediposing Factors: Humid cutaneous microclimate,
warm and/or humid climate or season; occlusive
clothing/shoes; obesity; diabetes mellitus; hiperhydrosis;
poor hygiene; and immunocompromised states.
PATHOGENESIS
Corynebacterium
minutissimum
dispersed over the
skin surface
In heat and
humidity
conditions: these
organisms
proliferate
Invade the upper
third of the
stratum corneum
Invade
intracellular
spaces
Penetrating
superficial
cornified cells and
keratinized cells
Hyperkeratotic
and likely
keratolytic
processes
Stratum corneum
is thickened
Lichenification
and
hyperpigmentation
ERYTHRASMA
CLINICAL MANIFESTATION
Figure 1. A. Sharply marginated, red patch in the axilla.
B. This macerated interdigital web-space.
A B
Commonly asymptomatic
Duration: weeks to months to years
Frequently misdiagnosed as tinea cruris
or pedis
DIAGNOSIS
1. Anamnesis :
Site of predilection
Toe webspaces
Inguinal folds (inner thigs)
Axilla
Groin
Intergluteal
Inframammary
Skin Lesion
Patches, sharply
marginated, macerated,
eroded, fissured, red or
brownish red.
Pruriticexcoriation,
lichenification
DIAGNOSIS
2. Physical examination:
DIAGNOSIS
3. Laboratory examinations:
a. Wood Lamp: Characteristic coral-red fluorescence (attributed to
coproporphyrin III). May not be present if patient has bathed recently.
Figure 2. A. Coral-red fluoresence of interdigital lesion
B. Coral-red fluoresence of inguinal (crural) lesion
DIAGNOSIS
b. Direct Microscopy: Negative for
fungal forms on KOH preparation of
skin scraping.
Figure 4. KOH preparation of skin
scraping show fine filaments of
Corynebacterium minutissimum.
c. Bacterial Culture:
Heavy growth of Corynebacterium.
Rules out Staphylococcus aureus,
group A or group B Streptococcus,
and Candida infection.
Pseudomonas aeruginosa webspace
infection (feet) is also present.
DIFFERENTIAL DIAGNOSIS
1. Pityriasis versicolor
Figure 5.
A. Pityriasis versicolor: These
lesion are darker (hyperemia
secondary inflammatory
response and increased
melanin).
B. Spaghetti and meatballs
appearence of Malassezia in
KOH preparation.
A
B
DIFFERENTIAL DIAGNOSIS
Figure 6.
2. Tinea Cruris: Blotchy
erythema with areas of
atrophy and scale on the right
medial upper thigh boerdering
the inguinal area.
3. Tinea Pedis (interdigital
type): Hyperkeratotic and
macerated (hydration of the
stratum corneum).
2.
3.
Tinea Pedis
(interdigital
type)
Tinea Cruris
Pityriasis
Versicolor
Site of
Predilection
Most: between
fourth and fifth
toes
Groins and
thighs, may
extend to
buttocks
Upper trunk,
upper arms, neck,
abdomen, axillae,
groins, thighs,
genitalia
Wood Lamp
Yellow-green Yellow-green
Blue-green
(yellowish white
or copper-orange)
Direct
microscopy
+ (septated
hyphae and
spora)
+ (septated
hyphae and
spora)
Spagetthi and
meatballs
apperance
Culture
Dermatophytes
can be isolated
Dermatophytes
can be isolated
Malassezia furfur
TREATMENT
1. Prevention/Prophylaxis: Wash with benzoyl
peroxide. Medicated powders. Topical antiseptic alcohol gels:
isopropyl, ethanol.
2. Topical Therapy: Preferable.
Benzoyl peroxide (2,5 %) gel daily, after showering, for 7 days
Topical erythromycin or clindamycin solution twice daily for 7
days
Sodium fusidate ointment, mupirocin ointment or cream
Benzoic acid cream (6%) and salicylic acid cream (3%)
Topical antifungal agents: clotrimazole, miconazole, econazole,
or ketoconazole (2%)
TREATMENT
3. Systemic Antibiotic Therapy:
Erythromycin:
Children: 30-50 mg/kgBW/day 7-10 days
Adult: 4 x 250 mg/day 2-3 weeks
Clarithromycin: 1 gram single dose
Tetracylin: 250 mg for 7 days
COMPLICATION & PROGNOSIS
Complication
Fatal septicemia
Infective
endocarditis
Postsurgical wound
infection
Prognosis
Excellent
The condition tends
to recur if the
predisposing factors
are not eliminated
S-ar putea să vă placă și
- Management of Tuberculosis: A guide for clinicians (eBook edition)De la EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Încă nu există evaluări
- HypermagnesemiaDocument5 paginiHypermagnesemiaNader Smadi100% (1)
- Riaz Gul AHN Unit 1Document106 paginiRiaz Gul AHN Unit 1Riaz Gul RindÎncă nu există evaluări
- WK13 CDN - Meningitis, Poliomyelitis, Leprosy, Tetanus, Red TideDocument43 paginiWK13 CDN - Meningitis, Poliomyelitis, Leprosy, Tetanus, Red TidePotato PceeÎncă nu există evaluări
- MeaslesDocument32 paginiMeaslesYum C100% (2)
- Blood TransfusionDocument5 paginiBlood TransfusionMoustafa Hazzaa100% (1)
- Final PPT SiDocument38 paginiFinal PPT SiSaad IqbalÎncă nu există evaluări
- Demo Teaching Physical Health AssessmentDocument5 paginiDemo Teaching Physical Health AssessmentJulie May SuganobÎncă nu există evaluări
- This Study Resource Was: Chamberlain College of NursingDocument5 paginiThis Study Resource Was: Chamberlain College of NursingHugsÎncă nu există evaluări
- Levofloxacin 500mg Film-Coated Tablets - Summary of Product Characteristics (SMPC)Document10 paginiLevofloxacin 500mg Film-Coated Tablets - Summary of Product Characteristics (SMPC)OdunlamiÎncă nu există evaluări
- Exam NurseDocument87 paginiExam Nurseyayasan daar alquran100% (1)
- CIP-NCM-121-Disaster Nursing-TuesdaysDocument3 paginiCIP-NCM-121-Disaster Nursing-TuesdaysKhen QuiringÎncă nu există evaluări
- Nursing Process Diagnosis Plan Implementation EvaluationDocument59 paginiNursing Process Diagnosis Plan Implementation EvaluationYemaya84Încă nu există evaluări
- Pre Authorization FormDocument1 paginăPre Authorization FormMurugan RamalingamÎncă nu există evaluări
- HypermagnesemiaDocument2 paginiHypermagnesemiaapi-3712326100% (1)
- Week 5 CareplanDocument2 paginiWeek 5 CareplanRaenell Curry100% (1)
- Management of A Patient With Acute Abdominal Pain - College of Surgeons of Sri Lanka 2007 PDFDocument30 paginiManagement of A Patient With Acute Abdominal Pain - College of Surgeons of Sri Lanka 2007 PDFRevalitha PutriÎncă nu există evaluări
- 8. Care of Child With GI Dysfunction (1) ءءءءDocument44 pagini8. Care of Child With GI Dysfunction (1) ءءءءNuhaÎncă nu există evaluări
- Orem'S Self-Care Deficit Nursing TheoryDocument39 paginiOrem'S Self-Care Deficit Nursing TheoryAlex AlegreÎncă nu există evaluări
- Muscle Strength TestingDocument3 paginiMuscle Strength TestingGiselle Chloe Baluya ico100% (1)
- Handout 1 Nursing ProcessDocument8 paginiHandout 1 Nursing ProcessGAMBOAÎncă nu există evaluări
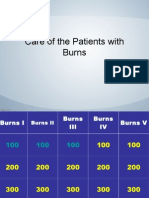
- Jeopardy Game - BurnsDocument42 paginiJeopardy Game - BurnsPC NÎncă nu există evaluări
- Final Teaching PlanDocument2 paginiFinal Teaching Planapi-352581650Încă nu există evaluări
- Incontinence Case StudyDocument26 paginiIncontinence Case StudyRose AnnÎncă nu există evaluări
- Naloxone in AdultsDocument8 paginiNaloxone in AdultsRoboschi StefaniaÎncă nu există evaluări
- Chart AuditDocument3 paginiChart AuditAnonymous WJtqIhhvPÎncă nu există evaluări
- AntepartalDocument43 paginiAntepartalxing414Încă nu există evaluări
- Urinary CatheterizationDocument2 paginiUrinary CatheterizationFains YdbwidÎncă nu există evaluări
- Ethical and Legal Issues in Perioperative NursingDocument3 paginiEthical and Legal Issues in Perioperative NursingJohn Pearl Fernandez100% (2)
- Postoperative Nursing CareDocument2 paginiPostoperative Nursing CareYeana AlonÎncă nu există evaluări
- Oral Glucose Tolerance TestDocument4 paginiOral Glucose Tolerance TestCyna Jane Yao AlcularÎncă nu există evaluări
- Module 1 To 4Document208 paginiModule 1 To 4smbawasainiÎncă nu există evaluări
- NCM 120 Skills LabDocument59 paginiNCM 120 Skills LabRoan DAlleÎncă nu există evaluări
- Drug Study TemplateDocument1 paginăDrug Study TemplateJulia Shane BarriosÎncă nu există evaluări
- Nursing Bullets: Fundamentals of Nursing ReviewerDocument44 paginiNursing Bullets: Fundamentals of Nursing ReviewerErl DiamanteÎncă nu există evaluări
- Research Synopsis FormatDocument13 paginiResearch Synopsis Formatmaya vermaÎncă nu există evaluări
- Demonstrating Theory in Practice Examples of The McGill Model of NursingDocument10 paginiDemonstrating Theory in Practice Examples of The McGill Model of NursingFerdy LainsamputtyÎncă nu există evaluări
- Intravenous Parenteral Therapy LectureDocument31 paginiIntravenous Parenteral Therapy Lecturerommelrn100% (1)
- Operational Guidelines For HWCDocument83 paginiOperational Guidelines For HWCharleenÎncă nu există evaluări
- N410 SyllabusDocument20 paginiN410 SyllabusTwobucktinÎncă nu există evaluări
- Guideline Antibiotic RationalDocument35 paginiGuideline Antibiotic RationalIstianah EsÎncă nu există evaluări
- Personal Data of Patient: Intensive Nursing Practicum - Pediatric Ward (BMC) CASE STUDY 5: Pediatric OncologyDocument12 paginiPersonal Data of Patient: Intensive Nursing Practicum - Pediatric Ward (BMC) CASE STUDY 5: Pediatric OncologyromelynÎncă nu există evaluări
- Sas#1 - Ite 303-SiaDocument7 paginiSas#1 - Ite 303-SiaFranzh Lawrence BataanÎncă nu există evaluări
- Antituberculous Therapy in Special SituationsDocument8 paginiAntituberculous Therapy in Special SituationsMobeen Raza100% (1)
- Shock Concept MapDocument2 paginiShock Concept MapElizabeth GarretsonÎncă nu există evaluări
- Maternal and Child Health Nursing: KeepsDocument32 paginiMaternal and Child Health Nursing: Keepsshenric16Încă nu există evaluări
- Hourly Round ProjectDocument8 paginiHourly Round ProjectaustinisaacÎncă nu există evaluări
- Module 1 Study QuestionsDocument13 paginiModule 1 Study QuestionsLuna AstanehÎncă nu există evaluări
- Rating Scale: 0 Omitted 1 Poorly Done 2 Fairly Done 3 Well Done Indicates Critical Step Omission or Poor Performance Equates To FailureDocument3 paginiRating Scale: 0 Omitted 1 Poorly Done 2 Fairly Done 3 Well Done Indicates Critical Step Omission or Poor Performance Equates To FailureTemahlungwane100% (1)
- SKILL 8-16 Drawing Blood From A Central Venous Catheter: Key TermsDocument7 paginiSKILL 8-16 Drawing Blood From A Central Venous Catheter: Key TermsElizalde HusbandÎncă nu există evaluări
- Heat Stroke PatophysiologyDocument48 paginiHeat Stroke PatophysiologyMbenk NjoeÎncă nu există evaluări
- Skin Cancer!Document8 paginiSkin Cancer!HudiansyahÎncă nu există evaluări
- Pruritus PRURITIS Pruritis (Itching) Is One of The Most CommonDocument2 paginiPruritus PRURITIS Pruritis (Itching) Is One of The Most CommonFreeNursingNotesÎncă nu există evaluări
- IV Cannulation ChecklistDocument2 paginiIV Cannulation ChecklistDo0odi AlharbiÎncă nu există evaluări
- Dhanusthamba/Dhanurvata/Tetanus: Dr. Mahesh C KundagolDocument19 paginiDhanusthamba/Dhanurvata/Tetanus: Dr. Mahesh C KundagolkundagolÎncă nu există evaluări
- Disaster Nursing SAS Session 15Document6 paginiDisaster Nursing SAS Session 15Niceniadas CaraballeÎncă nu există evaluări
- Provide Advanced Nursing Care (HLT NUR4 01222) : For Regular Nursing (Level Iv - TVET) Students AAMBC, January 2022Document56 paginiProvide Advanced Nursing Care (HLT NUR4 01222) : For Regular Nursing (Level Iv - TVET) Students AAMBC, January 2022Abel100% (1)
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsDe la EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsÎncă nu există evaluări
- Consolidated General Application Form Immigration Regulation DivisionDocument1 paginăConsolidated General Application Form Immigration Regulation DivisionAndrean LinataÎncă nu există evaluări
- Department of Dermatology Ospital NG Maynila Medical Center Pamantasan NG Lungsod NG MaynilaDocument21 paginiDepartment of Dermatology Ospital NG Maynila Medical Center Pamantasan NG Lungsod NG MaynilaAndrean LinataÎncă nu există evaluări
- PesanestetikaDocument2 paginiPesanestetikaAndrean LinataÎncă nu există evaluări
- Research 31233Document5 paginiResearch 31233Andrean LinataÎncă nu există evaluări
- Mary Grace Anne A. CalvaridoDocument15 paginiMary Grace Anne A. CalvaridoAndrean LinataÎncă nu există evaluări
- Photodiagnosis and Photodynamic Therapy: SciencedirectDocument5 paginiPhotodiagnosis and Photodynamic Therapy: SciencedirectAndrean LinataÎncă nu există evaluări
- FINAL Research Androgenetic AlopeciaDocument42 paginiFINAL Research Androgenetic AlopeciaAndrean LinataÎncă nu există evaluări
- Giacaman2019 Article UseOfTopicalNitricZincComplexSDocument6 paginiGiacaman2019 Article UseOfTopicalNitricZincComplexSAndrean LinataÎncă nu există evaluări
- Suh 2019Document23 paginiSuh 2019Andrean LinataÎncă nu există evaluări
- Reporting in Phototherapy-CompiledDocument78 paginiReporting in Phototherapy-CompiledAndrean LinataÎncă nu există evaluări
- Nailgrowth and Differentiation: Transer: Andrean LinataDocument5 paginiNailgrowth and Differentiation: Transer: Andrean LinataAndrean LinataÎncă nu există evaluări
- 10 1111@dth 13034Document6 pagini10 1111@dth 13034Andrean LinataÎncă nu există evaluări
- Atropine SulfateDocument4 paginiAtropine SulfateAndrean LinataÎncă nu există evaluări
- Eritrasma BelajarDocument6 paginiEritrasma BelajarAndrean LinataÎncă nu există evaluări
- Case Report Tyroid CA SkinDocument6 paginiCase Report Tyroid CA SkinAndrean LinataÎncă nu există evaluări
- Common Nevus: Clinical Diagnosis: Andrean Linata Ospital NG Maynila Medical CenterDocument26 paginiCommon Nevus: Clinical Diagnosis: Andrean Linata Ospital NG Maynila Medical CenterAndrean LinataÎncă nu există evaluări
- Total: TotalDocument1 paginăTotal: TotalAndrean LinataÎncă nu există evaluări
- Atropine SulfateDocument4 paginiAtropine SulfateAndrean LinataÎncă nu există evaluări
- Erythrasma Normal Y O U N G Adults Dorothy A. ERY: Department Bacteriology, ST John's Hospital, London, W.C.2Document8 paginiErythrasma Normal Y O U N G Adults Dorothy A. ERY: Department Bacteriology, ST John's Hospital, London, W.C.2Andrean LinataÎncă nu există evaluări
- Pityriasis VersicolorDocument4 paginiPityriasis VersicolorLidya NazirÎncă nu există evaluări
- DermatologyDocument4 paginiDermatologyRemelou Garchitorena AlfelorÎncă nu există evaluări
- Mycology NotesDocument9 paginiMycology NotesIya Corpus100% (1)
- Tinea KorporisDocument3 paginiTinea Korporishaprisia winaÎncă nu există evaluări
- Chapter22 LectureDocument45 paginiChapter22 Lecturecee_prasetyo100% (1)
- Tinea Pedis An Update 1Document6 paginiTinea Pedis An Update 1putrinurulapriliaÎncă nu există evaluări
- Miyajima 2013Document7 paginiMiyajima 2013Siti Bellia Arafah XndÎncă nu există evaluări
- Microbial Diseases of The Skin and Eyes (Microbiology Chapter 21)Document82 paginiMicrobial Diseases of The Skin and Eyes (Microbiology Chapter 21)Katrina Isabel100% (1)
- Palmoplantar PustulosisDocument6 paginiPalmoplantar PustulosisputraimanullahÎncă nu există evaluări
- Self Assessment CasesDocument512 paginiSelf Assessment CasesmixandgoÎncă nu există evaluări
- Tinea Pedis Et ManusDocument14 paginiTinea Pedis Et ManusagisagitaÎncă nu există evaluări
- Diagnosis and Management of Common Tinea InfectionsDocument23 paginiDiagnosis and Management of Common Tinea InfectionsGiovanni AnggastaÎncă nu există evaluări
- Assessing The IntegumentaryDocument73 paginiAssessing The IntegumentaryHelena Meurial HilkiahÎncă nu există evaluări
- Communicable DiseasesDocument176 paginiCommunicable DiseasesKimsha ConcepcionÎncă nu există evaluări
- Tinea VersicolorDocument4 paginiTinea Versicolorparand2003Încă nu există evaluări
- Annular LesionsDocument8 paginiAnnular LesionshpmcentreÎncă nu există evaluări
- Standar Kompetensi Dokter Umum 1Document11 paginiStandar Kompetensi Dokter Umum 1Desriani SariÎncă nu există evaluări
- Ekakustha and CarmakushtaDocument32 paginiEkakustha and CarmakushtaVenkatesan VidhyaÎncă nu există evaluări
- Fungal PresentationDocument93 paginiFungal PresentationBenediktus BayuÎncă nu există evaluări
- KohDocument5 paginiKohNanny HerwantoÎncă nu există evaluări
- Faktor Resiko Terjadinya Dermatofitosis2Document25 paginiFaktor Resiko Terjadinya Dermatofitosis2Anggi OvialitaÎncă nu există evaluări
- Nail TheoryDocument36 paginiNail TheoryPeter Frank0% (1)
- Superficial Mycoses: Paramasari D PHD Darukutni DRDocument50 paginiSuperficial Mycoses: Paramasari D PHD Darukutni DRSheilla ElfiraÎncă nu există evaluări
- Management of Tinea Corporis, Tinea CrurisDocument10 paginiManagement of Tinea Corporis, Tinea CrurisRansidelenta Vistaprila ElmardaÎncă nu există evaluări
- Common Skin RashesDocument8 paginiCommon Skin RashesVictoria GomezÎncă nu există evaluări
- Derm PathologyDocument21 paginiDerm PathologyMaria GeorgeÎncă nu există evaluări
- Sertaconazole A Review of Its Use in The Management of Superficial Mycoses in Dermatology and GynaecologyDocument21 paginiSertaconazole A Review of Its Use in The Management of Superficial Mycoses in Dermatology and GynaecologyEdwin MontañezÎncă nu există evaluări
- FF Psoriasis SampleDocument11 paginiFF Psoriasis Samplemol3yÎncă nu există evaluări
- CDPCEUT00038Document156 paginiCDPCEUT00038Siddhant YadavÎncă nu există evaluări
- ICD 10 - Chapter 1 Certain Infectious and Parasitic DiseasesDocument16 paginiICD 10 - Chapter 1 Certain Infectious and Parasitic DiseasesHuseikha VelayazulfahdÎncă nu există evaluări