Documente Academic
Documente Profesional
Documente Cultură
Fluid and Electrolyte Maps
Încărcat de
ChrFaDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
Fluid and Electrolyte Maps
Încărcat de
ChrFaDrepturi de autor:
Formate disponibile
Fluid and Electrolyte Balance
What?
60% of the adult body is fluid
Varies with age, gender, body size/fat
ICF (intracellular fluid)
2/3 of body
Skeletal muscle mass
ECF (Extracellular fluid)
1/3 of body
Intravascular (3-6L)
Plasma
blood volume
Interstitial (11-12L)
Lymph
Fluid surrounding cells
Transcellular (1 l)
Cerebral spinal, pericardial, intraocular,
pleural, digestive secretions, sweat
Third spacing loss of ECF into spaces that do not
contribute to equilibrium
Decreased urine output with adequate fluid
intake
Electrolytes
Major Cations: sodium, potassium, calcium,
magnesium, hydrogen ions
Major anions: chloride, bicarbonate, phosphate,
sulfate, protienate ions
Labs
Osmolality concentration of fluid that effects
movement of H2O between compartments;
measures solute concentration in blood/urine
Serum and urine measured
Urine Specific Gravity varies inversely with
urine volume
BUN varies w/ volume of urine output (etiologies
for / values)
Regulation of Fluid
Movement of fluid through capillary walls:
Hydrostatic pressure: exerted on walls of
blood vessels
Osmotic pressure: exerted by protein in
plasma
Types of Movement
Osmosis: Fluid moves from Low solute
concentration to high solute concentration
Diffusion: Solutes move from high
concentration to low concentration
Filtration: Movement of water, solutes occurs
from high hydrostatic pressure to an area of
low hydrostatic pressure
Active transport: Pump that moves fluid
from area of lower concentration to high
concentration
Move against concentration gradient
Sodium-potassium
pump:
maintains
Systemic
Routes: Gains
and losses
higher
eC NA
and lower IC K
Healthy: 2.500
cc I&O
daily
Requires
ATP
for
energy
Kidney: urine output: 1 ml urine/kg/hour
(1-2L/day)
Skin: sensible loss, perspiration; solutes Na, Cl, K
1,000 ml/hr due to activity/environment
Effect of fever, major burns
Insensible loss, evaporation (500 mL/day)
Lungs: insensible loss (300 mL/day), with
RR/Dry climate
GI Tract: 8L of fluids/day; 100-200 mL of fluid loss
Critical effects of diarrhea, fistulas
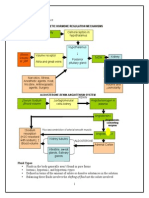
Fluid and Electrolyte Balance: Homeostatic
Mechanisms
Kidney
Regulation of:
ECF volume
Electrolyte levels
pH of ECF
Excretion of wastes/toxic substances
Heart, Blood Vessels
Pumping ensures adequate kidney
perfusion
Lung Functions
Fluid removal
Acid-Base balance
Pituitary Functions
Controls release of ADH
Adrenal Functions
Effects of aldosterone
Effects of cortisol
Parathyroid Functions
Parathyroid hormone (PTH)
Calcium and phosphate balance
Vascular
Baroreceptors: affect sympathetic
nervous system
Renin-angiotensin-aldosterone
system
Antidiuretic hormone and thirst
Osmoreceptors
Natriuretic peptides
Fluid Volume Deficits (FVD) - Hypovolemia
What?
FVD Loss of extracellular fluid exceeds
intake ratio of water
Electrolytes lost in same proportion
as they exist in normal body fluids
Dehydration Loss of water alone with
increased serum sodium level
Pathophysiology
Abnormal fluid loss:
Vomiting
Diarrhea
GI suctioning
Sweating
Inadequate intake:
Nausea
Third spacing
Disease states:
Diabetes insipidus
Major burns
Hemorrhage
Diagnostics
BUN
Serum Creatinine
Serum electrolytes
Urine specific gravity
Manifestations
Major fluid & electrolyte imbalances
Rapid weight loss
Decreased skin turgor
Oliguria, concentrated urine
Postural hypotension, rapid weak pulse,
increased temperature
Cool clammy skin (vasoconstriction),
thirst, nausea, muscle weakness, cramps
Geriatrics
Increased sensitivity to:
Fluid volume changes & Electrolyte
changes
Responsive to changes in function with:
Kidney
Cardiac
GI Function
Management
Medical
Provide fluid (oral, plasma vol.
expanders)
Assess renal function (urine output,
tests)
Nursing
I&O, Daily weight, vitals
Monitor: skin & tongue turgor,
mucosa, urine, mental status
Fluid Volume Excess (FVE) - Hypervolemia
What?
Isotonic expansion of ECF
Abnormal retention of water and sodium
consistent with normal proportions
Serum sodium levels remain normal
Pathophysiology
Due to fluid overload or diminished
homeostatic mechanisms
Risk factors: heart failure, renal failure,
liver cirrhosis
Contributing factors: excessive dietary
sodium or sodium containing IV solutions
Manifestations
Edema
Distended neck veins
Abnormal lung sounds (crackles),
tachycardia, increased blood pressure,
pulse pressure, CVP
Increased weight, increased urine output
Shortness of breath and wheezing
Management
Medical
Directed at cause
Restrictions of fluid and sodium
Administration of diuretics
Nursing
I&O, Daily weights; assess lung
sounds, edema, etc
Monitor response to meds
Promote adherence to fluid
rerstrictions
Teaching r/t sodium and fluid
limits
Monitor:
Avoid sources of excessive
sodium, including meds
Semi-fowlers position for
orthopnea
Skin care, positioning/trauma
Electrolyte Imbalances - Sodium
Hyponatremia
What?
Serum sodium less than 135 mEq/L
Causes: adrenal insufficiency, water
intoxication, SIADH or losses by vomiting,
diarrhea, sweating, diuretics
Manifestations
Poor skin turgor, dry mucosa, headache
Decreased salivation, decreased BP
nausea, abdominal cramping
Neurologic changes
Management
Medical
Water restriction
Sodium replacement
Nursing
Assessment and Prevention
Dietary sodium and fluid intake
Identify and monitor at-risk patients
Effects of meds (diuretics, lithium)
Hypernatremia
What?
Serum sodium greater than 145 mEq/L
Causes: Excess water loss, excess
sodium administration, diabetes
insipidus, heat stroke, hypertonic IV
solutions Manifestations
Thirst (may be impaired in elderly and
ill)
Elevated temperature, dry/swollen
tongue
Sticky mucosa
Neurologic symptoms
Restlessness,
weakness
Management
Medical
Hypotonic electrolyte solution or
D5W
Nursing
Assessment and prevention
Assess for OTC sources of sodium
Offer and encourage fluids
Provide sufficient fluids with tube
feedings
Electrolyte Imbalances - Potassium
Hypokalemia
What?
Serum potassoi, less than 3.5 mEq/L
Causes: GI losses, medications,
alterations of acid-base balance,
hyperaldosteronism, poor diet intake
Manifestations
Fatigue, anorexia, nausea, vomiting
Dysrhythmias, muscle weakness/cramps,
paresthesias
Glucose intolerance, decreased muscle
strength
DTRs
Management
Medical
Increased dietary potassium
Potassium replacement
IV for severe deficit
Nursing
Assessment
Severe deficit is life threatening
Monitor ECG and ABG
Dietary potassium
IV potassium administration
Hyperkalemia
What?
Serum potassium greater than 5.0 mEq/L
Causes: Usually treatment related, impaired
renal function, hypoaldosteronism, tissue
trauma, acidosis
Manifestations
Cardiac changes and dysrhythmias
Muscle weakness with potential respiratory
impairment
Paresthesias, anxiety, GI manifestations
Management
Medical
Monitor ECG
Limitation of dietary potassium
Cation-exchange resin (Kayexalate)
IV sodium bicarbonate
IV calcium gluconate
Regular insulin and hypertonic dextrose
IV
B-2 agonists
DIalysis
Nursing
Assess potassium levels
Mix Ivs containing K+ well
Monitor Med effects
Dietary potassium restrictions/ diet
teaching
Hemolysis of blood or drawing above IV
may cause false lab results
Salt substitutes, meds containing
Electrolyte Imbalances - Calcium
Hypocalcemia
What?
Serum calcium less than 8.6 mg/dL
(consider albumin)
Causes: Hypoparathyroidism,
malabsorption, pancreatitis, alkalosis,
massive transfusion of citrated blood,
Manifestations
renal failure,
medications
Tetany, circumoral numbness,
paresthesias
Hyperactive DTRs, Trouseaus sign,
Chovsteks sign
Seizures, respiratory symptoms (dyspnea
& laryngospasm)
Management
Abnormal clotting, anxiety
Medical
IV of calcium gluconate
Calcium and vitamin D supplements
Diet
Nursing
Assessment
Severe cases are life threatening
Weight-bearing exercises to decrease
bone calcium loss
Teaching related to diet and
medications
IV Calcium administration
Hypercalcemia
What?
Serum calcium greater than 10.2 mg/dL
Causes: Malignancy, and
hyperparathyroidism, bone loss related
to immobility
Manifestations
Muscle weakness, incoordination,
anorexia
Constipation, nausea, vomiting
Abdominal and bone pain
Polyuria, thirst
ECG changes, dysrhythmias
Management
Medical
Treat cause
Fluids
Furosemide, phosphates, calcitonin,
biphosphonates
Nursing
Assessment
Crisis has a high mortality
Ambulate patient
3-4 l fluids per day
Provide fluids with sodium unless CI
Fiber for constipation
Ensure safety
Electrolyte Imbalances - Magnesium
Hypomagnesemia
What?
Serum magnesium less than 1.3 mg/dL
(consider albumin)
Causes: Alcoholism, GI losses, enteral or
parenteral feeding deficit in magnesium,
medications, rapid administration of
citrated blood, contributing causes in:
DKA, sepsis,Manifestations
burns, hypothermia
Neuromuscular irritability, muscle
weakness, tremors
Athetoid movements, ECG changes and
dysrhythmias
Alterations inManagement
mood and LOC
Medical
Diet
Oral magnesium
Magnesium sulfate IV
Nursing
Assessment
Teaching: diet, meds, alcohol
IV magnesium sulfate administration
Often accompanies hypocalcemia
(monitor and treat)
Dysphagia common (assess pt
abilities)
Hypermagnesemia
What?
Serum Magnesium greater than 2.3
mg/dL
Causes: Renal failure, DKA, excess Mg
administration
Manifestations
Flushing, low BP, nausea, vomiting,
hypoactive reflexes
Drowsiness, muscle weakness, resp
depression
ECG changes, hemodialysis
Management
Medical
IV calcium gluconate, loop diuretics
IV NS or LR
Hemodialysis
Nursing
Assessment
Do not administer meds with
magnesium
Patient teaching regarding OTC
meds with Mg
Electrolyte Imbalances - Phosphorus
Hypophosphatemia
What?
Serum phosphorus less than 2.5 mg/dL
Causes: Alcoholism, refeeding of
patients after starvation, pain, heat
stroke, resp alkalosis, hyperventilation,
DKA, hepatic encephalopathy, major
burns, hyperparathyroidism, low
magnesium, low potassium, diarrhea, low
vitamin D, use
of diuretics or antacids
Manifestations
Neurologic symptoms, Confusion
Muscle weakness, tissue hypoxia,
muscle/bone pain
Increased susceptibility to infection
Hyperphosphatemia
Management
Management
Medical
Oral or IV replacement
Nursing
Assessment
Encourage foods high in phosphorus
Gradually introduce calories for
malnourished pts receiving
parenteral nutrition
What?
Serum phosphorus greater than 4.5
mg/dL
Causes: Renal failure, excess
phosphorus, excess vitamin D, acidosis,
hypoparathyroidism, chemotherapy
Manifestations
Few symptoms, soft tissue calcifications
Symptoms occur due to associated
hypocalcemia
Medical
Treat underlying disorder
Vitamin D preparations
Ca binding antacids
Phosphate-binding gels or antacids
Loop diuretics, NS IV, dialysis
Nursing
Assessment
Avoid high phosphorus foods
Diet teaching (phosphate
containing substances)
Signs of hypocalcemia
Electrolyte Imbalances - Chloride
Hypochloremia
What?
Serum chloride less than 97 mEq/L
Causes: Addisons disease, reduced
chloride intake, GI loss, DKA, Excessive
sweating, fever, burns, medications,
metabolic alkalosis
Loss of chloride occurs with loss of other
electrolytes (potassium, sodium)
Manifestations
Agitation, irritability, weakness
Hyperexcitability of muscles
Dysrhthmias, seizures, coma
Hyperchloremia
Management
Management
Medical
Replace chloride IV NS or 0.45% NS
Nursing
Assessment
Avoid free water
Encourage high-chloride foods
Patient teaching related to highchloride foods
What?
Serum Chloride greater than 107 mEq/L
Causes: Excess sodium chloride
infusions with water loss, head injury,
hypernatremia, dehydration, severe
diarrhea, respiratory alkalosis,
metabolic Manifestations
acidosis
Tachypnea, lethargy, weakness
Rapid/deep respirations
Hypertensions, cognitive changes
Normal serum anion gap
Medical
Restore electrolyte and fluid
balance, LR, sodium bicarbonate,
diuretics
Nursing
Assessment
Patient teaching related to diet and
hydration
S-ar putea să vă placă și
- Fluid and Electrolytes for Nursing StudentsDe la EverandFluid and Electrolytes for Nursing StudentsEvaluare: 5 din 5 stele5/5 (12)
- Handout Medical-Surgical Nursing Fluid and ElectrolyteDocument13 paginiHandout Medical-Surgical Nursing Fluid and ElectrolytePaul Christian P. Santos, RN100% (10)
- Fluid & ElectrolyteDocument26 paginiFluid & Electrolytesanjana bhatia100% (1)
- Chapter 14 Fluid and Electrolytes ChartsDocument7 paginiChapter 14 Fluid and Electrolytes ChartsBNA_RN100% (3)
- Fluids and Electrolytes HandoutsDocument15 paginiFluids and Electrolytes HandoutsSiv Carlaisle100% (3)
- RenalDocument54 paginiRenalUSC Upstate Nursing Coaches100% (1)
- Nursing Fluids and ElectrolytesDocument14 paginiNursing Fluids and Electrolytesaga1028100% (18)
- Fluid and ElectrolytesDocument13 paginiFluid and ElectrolytesHenry Philip93% (15)
- Head To Toe GuideDocument12 paginiHead To Toe GuideHer Cats100% (3)
- Nursing Diagnosis & Careplan SamplesDocument5 paginiNursing Diagnosis & Careplan SamplesE94% (18)
- Endocrine NursingDocument2 paginiEndocrine NursingUnclePorkchop94% (34)
- Fluid & Electrolytes Cheat Sheet v3Document1 paginăFluid & Electrolytes Cheat Sheet v3faten100% (1)
- MEDSURG - Cellular AberrationDocument10 paginiMEDSURG - Cellular AberrationLeslie CruzÎncă nu există evaluări
- Upper Respiratory Drugs #17Document5 paginiUpper Respiratory Drugs #17Gina Giammalvo100% (3)
- Fluid & ElectrolytesDocument6 paginiFluid & ElectrolyteskauragiousÎncă nu există evaluări
- Complete Assessment Script Print FormDocument6 paginiComplete Assessment Script Print Formkeirvyl0% (1)
- Nursing Cheat SheetDocument1 paginăNursing Cheat Sheetabardwell100% (85)
- Fluid and ElectrolytesDocument179 paginiFluid and ElectrolytesTrixie Al Marie75% (4)
- Head To Toe AssessmentDocument6 paginiHead To Toe AssessmentBernard Shao100% (3)
- Fluid and ElectrolytesDocument14 paginiFluid and Electrolytesstring44100% (2)
- Perioperative NursingDocument18 paginiPerioperative Nursinglagunda100% (2)
- Acute Renal Failure-Student-Rapid ReasoningDocument4 paginiAcute Renal Failure-Student-Rapid Reasoningapi-268403950Încă nu există evaluări
- Electrolytes StudyDocument14 paginiElectrolytes StudyAlly Shawnae Ordanozo88% (8)
- Chart of Neuro DisordersDocument1 paginăChart of Neuro DisordersNursingSchoolNotes100% (2)
- Head To Toe Physical AssessmentDocument16 paginiHead To Toe Physical Assessmentabagatsing100% (5)
- Health AssessmentttDocument64 paginiHealth AssessmentttAudreySalvador100% (4)
- Critical Thinking and The Nursing ProcessDocument48 paginiCritical Thinking and The Nursing ProcessNurseReyes100% (1)
- Health AssessmentDocument17 paginiHealth Assessmentsflower85100% (8)
- Fluid and Electrolytes (PDF File) : A. Body FluidsDocument5 paginiFluid and Electrolytes (PDF File) : A. Body FluidsLegendX100% (3)
- Pediatric Nursing Reviewer CardiovascularDocument4 paginiPediatric Nursing Reviewer CardiovascularJemy Lorane TemporalÎncă nu există evaluări
- Fundamentals of NursingDocument45 paginiFundamentals of NursingCarrei Anne H. Duque100% (1)
- Nueva Ecija University of Science and TechnologyDocument3 paginiNueva Ecija University of Science and TechnologyRay Anne GonzalesÎncă nu există evaluări
- Assessment Head To Toe ScriptDocument7 paginiAssessment Head To Toe Scriptannekemp96% (27)
- Exam #4 - Urinary and Renal-1Document14 paginiExam #4 - Urinary and Renal-1aerislina100% (6)
- Fundamentals of Nursing 25 Practice QuestionsDocument10 paginiFundamentals of Nursing 25 Practice QuestionsLara BÎncă nu există evaluări
- Different Types of IV FluidsDocument10 paginiDifferent Types of IV FluidsMarinill SolimanÎncă nu există evaluări
- Head To Toe AssessmentDocument9 paginiHead To Toe AssessmentTori Roland0% (1)
- NCLEX Fluids & ElectrolytesDocument6 paginiNCLEX Fluids & ElectrolytesNathalee Walker100% (1)
- Review of Systems For Current Health Problems (Health Assessment)Document5 paginiReview of Systems For Current Health Problems (Health Assessment)younggirldavid100% (1)
- Iggy Med Surg Test Bank Chapter 007Document10 paginiIggy Med Surg Test Bank Chapter 007Tracy Bartell100% (5)
- Concept Map Due 04Document9 paginiConcept Map Due 04api-545711468Încă nu există evaluări
- Endocrine Disorders (Study Notes)Document11 paginiEndocrine Disorders (Study Notes)Danelle Harrison, RN90% (10)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideDe la EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideÎncă nu există evaluări
- Fluids and Electrolytes Demystified, Second EditionDe la EverandFluids and Electrolytes Demystified, Second EditionÎncă nu există evaluări
- NLN PAX Practice: PAX-RN Practice Test QuestionsDe la EverandNLN PAX Practice: PAX-RN Practice Test QuestionsÎncă nu există evaluări
- Nursing Mnemonics: The Ultimate Tips and Notes For NursesDe la EverandNursing Mnemonics: The Ultimate Tips and Notes For NursesEvaluare: 5 din 5 stele5/5 (1)
- 2018 NCLEX-PN Test Prep. Questions and Answers with Explanations: Study Guide to Pass the License Exam Effortlessly - Exam Review for Practical NursesDe la Everand2018 NCLEX-PN Test Prep. Questions and Answers with Explanations: Study Guide to Pass the License Exam Effortlessly - Exam Review for Practical NursesEvaluare: 4.5 din 5 stele4.5/5 (2)
- Fluid and Electrolyte-2013Document91 paginiFluid and Electrolyte-2013shwetaÎncă nu există evaluări
- Fluid and Electrolyte BalanceDocument83 paginiFluid and Electrolyte BalanceRubinaÎncă nu există evaluări
- Fluids and Electrolytes SP 09Document119 paginiFluids and Electrolytes SP 09Amy100% (8)
- Fluid Electrolyte BalanceDocument59 paginiFluid Electrolyte BalanceLuqman RamzanÎncă nu există evaluări
- Fluids and ElectrolytesDocument62 paginiFluids and ElectrolytesLacy Ds FruitÎncă nu există evaluări
- Nur2731 3rd Semester Final ReviewDocument196 paginiNur2731 3rd Semester Final Reviewjanet rooseveltÎncă nu există evaluări
- Cairan Tubuh & ElektrolitDocument24 paginiCairan Tubuh & Elektrolitselviana hanifÎncă nu există evaluări
- SLIDE03 FluidElectrolyteImbalanceDocument57 paginiSLIDE03 FluidElectrolyteImbalanceGrace Amato-Moore100% (1)
- Acid BaseDocument74 paginiAcid BaseMiracle For NursesÎncă nu există evaluări
- 1.A Ndera CaseDocument13 pagini1.A Ndera CaseNsengimana Eric MaxigyÎncă nu există evaluări
- Infectii CutanateDocument24 paginiInfectii CutanateMaria Minodora PascuÎncă nu există evaluări
- Health and Safety Solutions Accident Investigation FormDocument2 paginiHealth and Safety Solutions Accident Investigation Formhussein aliÎncă nu există evaluări
- Use E-MANIC' For Secondary Mania Workup: Dowden Health MediaDocument2 paginiUse E-MANIC' For Secondary Mania Workup: Dowden Health MediaJagdishVankarÎncă nu există evaluări
- FNCPDocument4 paginiFNCPJonalyn Tumanguil100% (2)
- Amenore Galactorea Hyperprolactinemia Adenoma HypophysisDocument24 paginiAmenore Galactorea Hyperprolactinemia Adenoma HypophysisShabrina Sari MedinaÎncă nu există evaluări
- Current Diagnosis and Treatment Cardiology 5Th Edition Michael H Crawford Full ChapterDocument67 paginiCurrent Diagnosis and Treatment Cardiology 5Th Edition Michael H Crawford Full Chapterkaty.manley552100% (4)
- Fever TakingDocument7 paginiFever TakingSantosh BhandariÎncă nu există evaluări
- DAY Date: Observation ReportDocument30 paginiDAY Date: Observation ReportPadma priyaÎncă nu există evaluări
- Acc-Aha - Full Text) Unstable Anghina and Non-St AmiDocument93 paginiAcc-Aha - Full Text) Unstable Anghina and Non-St Amiapi-3765169Încă nu există evaluări
- Alcoholic Hepatitis Diagnosis and ManagementDocument10 paginiAlcoholic Hepatitis Diagnosis and ManagementGW GeistÎncă nu există evaluări
- (Luo Xiwen) Treatise On Febrile Diseases Caused by Cold With 500 CasesDocument580 pagini(Luo Xiwen) Treatise On Febrile Diseases Caused by Cold With 500 CasesAlexandre HenriquesÎncă nu există evaluări
- Pathophysiology DKADocument2 paginiPathophysiology DKALovely CacapitÎncă nu există evaluări
- 404 Veterinary Referral Hospital - BrochureDocument11 pagini404 Veterinary Referral Hospital - BrochureJoanne FagnouÎncă nu există evaluări
- Arachnoid CystDocument4 paginiArachnoid CystSlaviša KovačevićÎncă nu există evaluări
- Dermatology - PedsDocument16 paginiDermatology - PedsbencleeseÎncă nu există evaluări
- Jurnal Retinopaty DiabetikumDocument11 paginiJurnal Retinopaty DiabetikumrestikaÎncă nu există evaluări
- Case Report EpilepsyDocument47 paginiCase Report EpilepsySonya HyekyoÎncă nu există evaluări
- Diagnosis and Treatment of Clostridioides (Clostridium) Difficile Infection in Adults in 2020Document2 paginiDiagnosis and Treatment of Clostridioides (Clostridium) Difficile Infection in Adults in 2020Alem OrihuelaÎncă nu există evaluări
- ECG Interpretation Program: User'S GuideDocument154 paginiECG Interpretation Program: User'S Guidemogahid jojoÎncă nu există evaluări
- Liver Trauma CaseDocument7 paginiLiver Trauma CaseMario KopljarÎncă nu există evaluări
- Amit Agrawal 2303705Document4 paginiAmit Agrawal 2303705Anushtha AgrawalÎncă nu există evaluări
- 16 Corneal DegenerationsDocument11 pagini16 Corneal DegenerationsIrma FloresÎncă nu există evaluări
- 54205-Article Text-94353-1-10-20100629Document7 pagini54205-Article Text-94353-1-10-20100629JamesÎncă nu există evaluări
- A Comparative Study OF NIHSS Between Ischemic Stroke Patients With and Without Risk FactorsDocument4 paginiA Comparative Study OF NIHSS Between Ischemic Stroke Patients With and Without Risk FactorsKlinik HanisÎncă nu există evaluări
- Amputation Guideline EN PDFDocument3 paginiAmputation Guideline EN PDFMuhammad RezaÎncă nu există evaluări
- Disaster Triage Forgotten Lessons in Pandemic Covid-19 Management - Dr. Yogi Prabowo, SpOT (K)Document23 paginiDisaster Triage Forgotten Lessons in Pandemic Covid-19 Management - Dr. Yogi Prabowo, SpOT (K)Clara EverlastÎncă nu există evaluări
- Open Book Exam - Renal Dz. 2019Document2 paginiOpen Book Exam - Renal Dz. 2019Ahmed AliÎncă nu există evaluări
- Nplex Micro ChartDocument12 paginiNplex Micro Chartapi-26938624100% (2)
- Bihag Quiz Medicine AreaDocument5 paginiBihag Quiz Medicine AreaDan HizonÎncă nu există evaluări