Documente Academic
Documente Profesional
Documente Cultură
PERICARDIOCENTESIS
Încărcat de
rasta0 evaluări0% au considerat acest document util (0 voturi)
759 vizualizări25 paginiPericardiocentesis is a procedure to remove fluid from the pericardial sac surrounding the heart, which can be performed to diagnose the cause of a pericardial effusion, relieve symptoms of cardiac tamponade, or for other therapeutic reasons. The document describes the indications, contraindications, equipment, steps, techniques including ultrasound-guided and ECG-monitored approaches, assessments after the procedure, possible complications, and post-procedure care for pericardiocentesis.
Descriere originală:
Titlu original
PERICARDIOCENTESIS.pptx
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PPTX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentPericardiocentesis is a procedure to remove fluid from the pericardial sac surrounding the heart, which can be performed to diagnose the cause of a pericardial effusion, relieve symptoms of cardiac tamponade, or for other therapeutic reasons. The document describes the indications, contraindications, equipment, steps, techniques including ultrasound-guided and ECG-monitored approaches, assessments after the procedure, possible complications, and post-procedure care for pericardiocentesis.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPTX, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
759 vizualizări25 paginiPERICARDIOCENTESIS
Încărcat de
rastaPericardiocentesis is a procedure to remove fluid from the pericardial sac surrounding the heart, which can be performed to diagnose the cause of a pericardial effusion, relieve symptoms of cardiac tamponade, or for other therapeutic reasons. The document describes the indications, contraindications, equipment, steps, techniques including ultrasound-guided and ECG-monitored approaches, assessments after the procedure, possible complications, and post-procedure care for pericardiocentesis.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPTX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 25
PERICARDIOCENTESIS
Definition
Pericardiocentesis is the removal of fluid from the
pericardial space surrounding the heart. The fluid is
usually aspirated with a needle and syringe.
This may be performed for diagnosis, to obtain
pericardial fluid; to relieve a pericardial effusion and
improve cardiac output; or as a lifesaving measure to
relieve a cardiac tamponade.
Cardiac Tamponade
Cardiac tamponade is a clinical syndrome caused by
the accumulation of fluid in the pericardial space,
resulting in reduced ventricular filling and subsequent
hemodynamic compromise.
Beck's triad of muffled heart sounds, hypotension,
and jugular venous distention is associated with
cardiac tamponade. Almost all patients with cardiac
tamponade will have at least one of these signs.
Diagnostic Finding
Indication Contraindication
Emergent: Small, loculated, or
posteriorly located effusions
The presence of life threatening
hemodynamic changes in a in a stable patient
patient with suspected cardiac
tamponade
Traumatic pericardial efusion
with unstable vital sign
Nonemergent:
Myocardial rupture
The aspiration of pericardial
fluid in hemodynamically stable Aortic dissection
patient for diagnostic or
palliative reasons, performed Severe bleeding disorder
under USG, CT, or flouroscopic
visualization
Equipment
Code cart and resucitation
equipment
Hemodynamic monitoring
device
Ultrasound machine
ECG machine
18 G spinal needle
Three way stopcock
20 ml syringe
Antibacterial Skin Cleanser
Wire with alligator clips
Sterile gloves
Patient Preparation
Explain the procedure to the
patient and/or their
representative.
If possible, place the patient
semirecumbent at a 30 to 45
degree angle.. The supine
position is an acceptable
alternative.
Assess the patient for any
mediastinal shift.
Apply the cardiac monitor, pulse
oximeter, BP monitor and
supplemental oxygen to the
patient.
Insert a nasogastric tube to
decompress the stomach..
1. Identify the anatomic
landmarks. The needle
can be inserted at
numerous sites. These
include the following:
below the xiphoid process,
at the right sternocostal
margin, at the left
sternocostal margin
(subxiphoid approach)
In the left or right fifth
intercostal space
parasternally (parasternal
approach)
in the left fifth intercostal
space at the midclavicular
line (apical approach).
2. Apply povidone iodine solution to the xiphoid and
subxiphoid areas and allow it to dry.
3. If time allows, apply sterile drapes to delineate a sterile
surgical field. Reidentify the anatomic landmarks. Put on
sterile gloves and mask, dress in a sterile gown.
4. Infiltrate local anesthetic solution at the chosen site by first
creating a skin wheal and then infiltrating the subcutaneous
and deeper tissues.
5. Puncture the skin using a No. 11 blade scalpel at the
chosen site
6. Connect a 20 or 60 ml syringe to the spinal needle, aspirate
5 ml of normal saline onto the syringe.
Blind Insertion Technique
1. Grasp the syringe with the
dominant hand. Insert the
spinal needle (16-18 G)
through the skin at a 45
degree angle to the
midsagittal plane and at a
45 degree angle to the
abdominal wall.
2. Advance the spinal needle 4
to 5 cm while applying
negative pressure to the
syringe until a return of fluid
is visualized, cardiac
pulsations are felt, or an
abrupt change in the ECG
waveform is noted.
Notes:
If the ECG shows an injury
pattern, slowly withdraw the
needle (1-2mm) until the
pattern returns to normal
While advancing the needle,
inject 0.25 to 0.50 mL of
saline occasionally to ensure
that the needle remains
patent.
6. When the pericardial space is entered and fluid is
aspirated, there should be a marked improvement in the
patient's clinical status. Withdraw as much fluid as possible.
When the syringe is filled with fluid, stop withdrawing the
plunger. Replace the syringe with a new one.
7. An alternative setup to replacing syringes is using a 3-way
stopcock and intravenous tubing, which allows the
physician to aspirate pericardial fluid into the syringe and
eject the fluid into a basin or collection bag.
8. As pericardial fluid is aspirated, the needle may move
closer to the heart, and if an injury pattern appears on the
ECG waveform, then the needle should be slowly
withdrawn.
9. Remove the needle when fluid can no longer be aspirated.
ECG-Monitored Technique
The purpose of ECG monitoring is to prevent accidental
ventricular puncture with the spinal needle.
Attach one alligator clip to the base of the spinal needle and
the other to the V1 lead of the ECG machine. The V1 lead
will serve as an active electrode based at the tip of the
spinal needle.
As the spinal needle is advanced, an injury pattern noted by
ST-segment elevation will be seen if the myocardium is
contacted or penetrated by the spinal needle.
If an injury pattern or premature ventricular complexes are
seen on the ECG monitor, withdraw the needle in 1 to 2 mm
increments until the injury pattern disappears.
Seldinger Technique
An indwelling catheter may be placed in the pericardial
cavity to drain the pericardial fluid
This may be done in cases of medical or traumatic
pericardial effusions, since the pericardial fluid often
reaccumulates. An indwelling catheter allows
intermittent drainage of pericardial fluid without the
potential complications associated with repeated
needle sticks from a pericardiocentesis.
Ultrasound-Guided Technique
The ultrasound is used to localize the area of the
largest effusion. The point of needle insertion will be
where the pericardial fluid is maximal.
The transducer is used to locate the area of largest
effusion and the needle is inserted suitably close by
and advanced toward the maximal effusion. Proper
needle placement can be further confirmed by injecting
saline that has been shaken to produce bubbles. The
bubbles will show well on the ultrasound.
Confirmation
Clotting: intracardiac blood forms a clot, whereas
pericardial aspirate should not form a clot.
Hematocrit or hemoglobin measurement: the
pericardial aspirate should have a lower hemoglobin
concentration than the patient’s peripheral blood.
ASSESSMENT
a significant improvement in the patient's clinical status
should be observed after successful drainage of the
pericardial space.
The patient's blood pressure and cardiac output should
increase while intracardiac pressure and
intrapericardial pressure decrease.
Obtain a chest radiograph after the procedure to rule
out a hemothorax and/or pneumothorax.
AFTERCARE
Secure the catheter with sutures to the skin and check for
stability.
Monitor patients for reaccumulation of pericardial fluid and
for hemodynamic instability.
If fluid reaccumulates, the procedure should be repeated or
the stopcock opened and the pericardial space reaspirated.
Flush with sterile saline after each aspiration to maintain the
patency of the catheter.
Consult a Thoracic Surgeon if purulent fluid is aspirated in
medical patients.
All patients must be admitted to an intensive care unit for
further monitoring, evaluation, and treatment.
COMPLICATION
Aspiration of ventricular blood instead of pericardial blood
Laceration of ventricular epicardium/myocardium
Laceration of coronary artery or vein
New hemopericardium
Ventricular fibrillation
Pneumotorax
Puncture of great vessels with worsening of pericardial tamponade
Puncture of esophagus with subsequent mediastinitis
Puncture of peritoneum with subsequent peritonitis or false
positive aspirate
S-ar putea să vă placă și
- Percutaneous Transluminal Coronary AngioplastyDocument22 paginiPercutaneous Transluminal Coronary AngioplastyArya Gaunker100% (1)
- Abg AnalysisDocument9 paginiAbg AnalysisLakshmi RjÎncă nu există evaluări
- Hemodynamic Monitoring 1Document10 paginiHemodynamic Monitoring 1Savita HanamsagarÎncă nu există evaluări
- Sister Nivedita Govt. Nursing College Igmc, ShimlaDocument10 paginiSister Nivedita Govt. Nursing College Igmc, ShimlashivaniÎncă nu există evaluări
- IV Cannulation and Fixation Infusion PumpDocument23 paginiIV Cannulation and Fixation Infusion PumpUday Kumar0% (1)
- Inhalation or Aerosols Therapy1Document21 paginiInhalation or Aerosols Therapy1drnasir31Încă nu există evaluări
- Assignment ON: TOPIC: PTCA (Percutaneous Transluminous Coronary Angioplasty)Document7 paginiAssignment ON: TOPIC: PTCA (Percutaneous Transluminous Coronary Angioplasty)soniya josephÎncă nu există evaluări
- BVCCT-501 Cardiac Catheterization Laboratory BasicsDocument52 paginiBVCCT-501 Cardiac Catheterization Laboratory BasicsManisha khan100% (1)
- Case Study On PacemakersDocument6 paginiCase Study On PacemakersBalamuruganÎncă nu există evaluări
- Bone Marrow AspirationDocument43 paginiBone Marrow AspirationDr. Pawan KumarÎncă nu există evaluări
- 0347burst AbdomenDocument24 pagini0347burst AbdomenSathishKumar100% (1)
- Nasogastric Aspiration: Preparation of ArticlesDocument2 paginiNasogastric Aspiration: Preparation of ArticlesVarun ToshniwalÎncă nu există evaluări
- Centrel Venous CatheterizationDocument77 paginiCentrel Venous CatheterizationAli100% (1)
- Cardiac MonitoringDocument6 paginiCardiac MonitoringAIMÎncă nu există evaluări
- ETT IntubationDocument10 paginiETT IntubationPoova RagavanÎncă nu există evaluări
- Lumbar PunctureDocument18 paginiLumbar PunctureJaspreet KangÎncă nu există evaluări
- Atrial Septal DefectDocument3 paginiAtrial Septal Defectmu_crÎncă nu există evaluări
- Blood Transfusion PDFDocument7 paginiBlood Transfusion PDFBaboolal100% (2)
- Assisting Central Venous Catheter (CVC) Insertion (Procedure1)Document7 paginiAssisting Central Venous Catheter (CVC) Insertion (Procedure1)BsBs A7medÎncă nu există evaluări
- Sub - Medical Surgical Nursing: Assignment On CVP MonitoringDocument11 paginiSub - Medical Surgical Nursing: Assignment On CVP Monitoringkamini ChoudharyÎncă nu există evaluări
- Lumbar Puncture (LP)Document10 paginiLumbar Puncture (LP)Fady Jehad ZabenÎncă nu există evaluări
- Angiography: Presented By: Mulituba, Nairah DDocument9 paginiAngiography: Presented By: Mulituba, Nairah DAkazukin AineÎncă nu există evaluări
- Allen's TestDocument8 paginiAllen's TestJustineMaeMadroñalÎncă nu există evaluări
- Defibrillation TypedDocument8 paginiDefibrillation TypedValarmathiÎncă nu există evaluări
- Bone Marrow AspirationDocument2 paginiBone Marrow AspirationJClaudz PilapilÎncă nu există evaluări
- ANGIOGRAPHYDocument8 paginiANGIOGRAPHYAkazukin AineÎncă nu există evaluări
- Heart Block: BY DR - AriyalakshmiDocument26 paginiHeart Block: BY DR - AriyalakshmiDiksha chaudharyÎncă nu există evaluări
- On Emergency DrugsDocument25 paginiOn Emergency DrugsBikram Chhetry100% (1)
- Chest TraumaDocument79 paginiChest TraumaAnusha VergheseÎncă nu există evaluări
- Monitoring of Critically Ill PatientDocument11 paginiMonitoring of Critically Ill PatientAnusikta PandaÎncă nu există evaluări
- Bone Marrow AspirationDocument6 paginiBone Marrow AspirationSai PardhuÎncă nu există evaluări
- Dialyzer Reprocessing Flow ChartDocument1 paginăDialyzer Reprocessing Flow ChartGrafe ChuaÎncă nu există evaluări
- Preparation For EndosDocument17 paginiPreparation For EndoscsngiuÎncă nu există evaluări
- Cardio Pulmonary ResuscitationDocument13 paginiCardio Pulmonary Resuscitationaparna100% (1)
- Needle Cricothyroidotomy 2 - Hatem AlsrourDocument32 paginiNeedle Cricothyroidotomy 2 - Hatem Alsrourhatem alsrour100% (2)
- Cardiac MonitoringDocument5 paginiCardiac MonitoringAmit Kl100% (1)
- Central Venous Pressure Monitoring ManualDocument6 paginiCentral Venous Pressure Monitoring ManualCristina L. JaysonÎncă nu există evaluări
- Disorders of AortaDocument25 paginiDisorders of Aortavani reddyÎncă nu există evaluări
- SP42 Thoracentesis (Adult)Document7 paginiSP42 Thoracentesis (Adult)Adam HuzaibyÎncă nu există evaluări
- Lesson Plan BMA&BDocument14 paginiLesson Plan BMA&BLoma Waghmare (Jadhav)Încă nu există evaluări
- Cardio Vascular Assessment: Manali H Solanki F.Y.M.Sc - Nursing J G College of NursingDocument46 paginiCardio Vascular Assessment: Manali H Solanki F.Y.M.Sc - Nursing J G College of NursingmeghanaÎncă nu există evaluări
- Aetiology Heart Diasease in Children May Be Congenital or AcquiredDocument23 paginiAetiology Heart Diasease in Children May Be Congenital or AcquiredkasondaÎncă nu există evaluări
- Medical-Surgical EmergenciesDocument78 paginiMedical-Surgical EmergenciesGopala Hari100% (8)
- Equipment EditedDocument6 paginiEquipment EditedCHRISTINE JOY. MOLINAÎncă nu există evaluări
- Seminar On PacemakerDocument14 paginiSeminar On Pacemakerjyothi50% (4)
- Advanced Cardiac ProcedureDocument9 paginiAdvanced Cardiac ProcedureSachin DwivediÎncă nu există evaluări
- OT Equipments: Hold The Highest Standard With Best Pieces of EquipmentsDocument71 paginiOT Equipments: Hold The Highest Standard With Best Pieces of Equipmentsradhika333100% (1)
- VentilatorDocument9 paginiVentilatorSheeba StephenÎncă nu există evaluări
- Institute of Nursing and Allied Health SciencesDocument2 paginiInstitute of Nursing and Allied Health Sciencesshadow gonzalezÎncă nu există evaluări
- Pulse Oximetry IDocument4 paginiPulse Oximetry IFriends Forever100% (1)
- Purbanchal University Shree Medical and Technical College Bharatpur 10, ChitwanDocument10 paginiPurbanchal University Shree Medical and Technical College Bharatpur 10, Chitwansushma shresthaÎncă nu există evaluări
- Bone Marrow Aspiration and BiopsyDocument2 paginiBone Marrow Aspiration and Biopsyprince10120% (1)
- ThoracentesisDocument4 paginiThoracentesisCyntia Theresia Lumintang100% (1)
- Care of Chest Tube Drainage & Nursing Manangement SHDocument82 paginiCare of Chest Tube Drainage & Nursing Manangement SHJoanna RemollinoÎncă nu există evaluări
- Procedural Checklist For Care of TracheostomyDocument2 paginiProcedural Checklist For Care of TracheostomyAbegail TabuniagÎncă nu există evaluări
- PericarditisDocument45 paginiPericarditisBrenda WardshoneÎncă nu există evaluări
- Mitral Stenosis: Dr. Mohammed Asrafur Rahman MBBS, Bcs (H), MD Resident (Internal Medicine) (P-A) Chattogram Medical CollegeDocument16 paginiMitral Stenosis: Dr. Mohammed Asrafur Rahman MBBS, Bcs (H), MD Resident (Internal Medicine) (P-A) Chattogram Medical CollegeAsrafur RahmanÎncă nu există evaluări
- Arterial LineDocument2 paginiArterial LineRaghav Goyal100% (1)
- Lumbar PunctureDocument27 paginiLumbar PunctureWitneyGrace100% (1)
- PericardiocintesisDocument20 paginiPericardiocintesisKarelau KarniaÎncă nu există evaluări
- Dolor CVNADocument15 paginiDolor CVNAStephania MendozaÎncă nu există evaluări
- Paper Lips1Document11 paginiPaper Lips1dominiqueÎncă nu există evaluări
- Male Catheterization (Indwelling)Document43 paginiMale Catheterization (Indwelling)Dan Floyd FernandezÎncă nu există evaluări
- Digestive SystemDocument10 paginiDigestive SystemLindsay AnquiloÎncă nu există evaluări
- DR Sourabh Patwardhan's Phaco Handbook Ed 1-2Document106 paginiDR Sourabh Patwardhan's Phaco Handbook Ed 1-2Nounzia Boucherit BoubekriÎncă nu există evaluări
- AIIMS Nursing Officer Question Paper With Key 2019-1Document35 paginiAIIMS Nursing Officer Question Paper With Key 2019-1shubham vermaÎncă nu există evaluări
- Data Sarana PrasaranaDocument18 paginiData Sarana PrasaranaFlora Indah FajarwattyÎncă nu există evaluări
- Terminologi Kedokteran Patologi KlinikDocument12 paginiTerminologi Kedokteran Patologi KlinikchristobawelleÎncă nu există evaluări
- Total Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Post-OperativeDocument2 paginiTotal Abdominal Hysterectomy Bilateral Salpingo Oophorectomy (Tahbso) Nursing Responsibilities Rationale Post-OperativeMiar QuestÎncă nu există evaluări
- Meta 4 - de Jong DM - 2022Document13 paginiMeta 4 - de Jong DM - 2022matheus.verasÎncă nu există evaluări
- Retinoblastoma and Management - A Post-Graduate Pocket Book Manjandavida FPDocument18 paginiRetinoblastoma and Management - A Post-Graduate Pocket Book Manjandavida FPSyeda F AmbreenÎncă nu există evaluări
- Esthetic Depigmentation of Anterior Gingiva: A Case: Indian Dental JournalDocument3 paginiEsthetic Depigmentation of Anterior Gingiva: A Case: Indian Dental JournalSaatvik AtriÎncă nu există evaluări
- 45 Min FibulaDocument3 pagini45 Min FibulaTor ChiuÎncă nu există evaluări
- Signs and Symptoms Of: How Does Your Kidneys Do?Document2 paginiSigns and Symptoms Of: How Does Your Kidneys Do?Afia TawiahÎncă nu există evaluări
- Impression HonigumDocument4 paginiImpression Honigumandrian_10Încă nu există evaluări
- Radiology Dissertation TopicsDocument4 paginiRadiology Dissertation TopicsWriteMyPaperForCheapCanada100% (1)
- Sesap16 Volume 1Document459 paginiSesap16 Volume 1Kamil Hanna0% (1)
- Operative Exam Questions DR Hatem Sahar 2012-2013Document2 paginiOperative Exam Questions DR Hatem Sahar 2012-2013Abdallah GamalÎncă nu există evaluări
- 133-Article Text-648-3-10-20190525 PDFDocument6 pagini133-Article Text-648-3-10-20190525 PDFyantiÎncă nu există evaluări
- Mitsuo Ochi, Konsei Shino, Kazunori Yasuda, Masahiro Kurosaka (Eds.) - ACL Injury and Its Treatment-Springer Japan (2016) PDFDocument546 paginiMitsuo Ochi, Konsei Shino, Kazunori Yasuda, Masahiro Kurosaka (Eds.) - ACL Injury and Its Treatment-Springer Japan (2016) PDFdrbaneÎncă nu există evaluări
- Cardiac Catheterization and Coronary AngiographyDocument5 paginiCardiac Catheterization and Coronary Angiographyedem100% (1)
- Nurs 603 Assignment 2Document6 paginiNurs 603 Assignment 2api-429205355Încă nu există evaluări
- Cardiac Surgery Basic KnowledgeDocument28 paginiCardiac Surgery Basic KnowledgeGinwong100% (1)
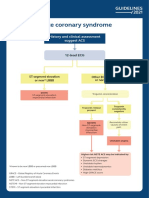
- Acute Coronary Syndrome: History and Clinical Assessment Suggest ACSDocument12 paginiAcute Coronary Syndrome: History and Clinical Assessment Suggest ACSginongÎncă nu există evaluări
- CraniotomyDocument10 paginiCraniotomyUzma KhanÎncă nu există evaluări
- Extensor Tendon InjuriesDocument35 paginiExtensor Tendon InjuriesPk Nutsuklo100% (1)
- Anatomy Lower LimbDocument4 paginiAnatomy Lower Limbch yaqoobÎncă nu există evaluări
- MCQ 123Document13 paginiMCQ 123Satya Asatya67% (3)
- Indravati PCPNDT 2 MoDocument6 paginiIndravati PCPNDT 2 MoDr Sachin Chitnis M O UPHC AiroliÎncă nu există evaluări
- Procedure Guide For Bag Technique Part 3Document2 paginiProcedure Guide For Bag Technique Part 3CrishaGarraÎncă nu există evaluări