Documente Academic
Documente Profesional
Documente Cultură
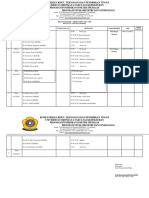
Menentukan Penurunan Kepala Janin Dengan Station Dan Perlimaan
Încărcat de
Rakhmad Hidayat0 evaluări0% au considerat acest document util (0 voturi)
118 vizualizări21 paginii
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PPTX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documenti
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPTX, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
118 vizualizări21 paginiMenentukan Penurunan Kepala Janin Dengan Station Dan Perlimaan
Încărcat de
Rakhmad Hidayati
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPTX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 21
Dr. H.
Amir Fauzi, SpOG(K)
LUT can be divided into:
1. The bladder: consists of
the detrusor muscle
covered by an adventitia and serosa over its dome,
lined by a submucosa and transitional cell epithelium
2. Urethra:
holds urine in the bladder determine urinary continenceprimary factor responsible
for stress incontinence.
> 50% of stress incontinence is directly attributable to max urethra closure pressure
The urethra is a complex tubular viscus extending below
3. the vesical neck : at the junction
1. Bladder: muscle within the detrusor
2. Urethra: sphincter urethra, urethrovaginal sphincter, compressor
urethrae
3. Vesical neck: urogenital sphincter muscle
1. Pelvic Diaphragm: the urethral lumen traverses the bladder wall before
becoming surrounded by the urethral wall. It contains portions of the bladder
muscle, and also elements that continue into the urethra.
2. The pelvic floor relates to:
Micturition
Continence
pelvic organ support: bladder and urethra depend upon attachments to the pelvic floor
for their shape and position
I. Outlet dysfunction: bladder outlet and pelvic floor
A. Underactive outlet (decreased urethral resistance)
Symptomatic: Stress urinary incontinence (SUI)
1. Anatomical support defects (SUI-A) (types I and II SUI): anatomical motion creates inequities in
transmission pressures to bladder and outlet, overcoming urethral resistance, and/or and conformational
changes caused by vaginal wall motion disrupt outlet integrity.
2. ISD (SUI-ISD) (type III) (LUCP): deficiency of the urethral closure mechanism secondary to decreased
innervation, vascularization or trauma to mucosa, submucosa or smooth, non-striated skeletal or skeletal
musculature of urethra–intrinsic deficiency of the closure mechanism.
3. Combined SUI (SUI-A-ISD): a degree of both anatomical motion and sphincter dysfunction.
4. Failure to inhibit the detrusor: decreased pelvic fl oor inhibitory activity of bladder (etiology for OAB–see
C): failure to contract pelvic floor releases detrusor reflex and decreases ability to inhibit active contraction.
B. Overactive outlet (increased urethral resistance)
Symptomatic: overflow incontinence/retention; frequency–urgency.
I. Outlet dysfunction: bladder outlet and pelvic floor
A. Underactive outlet (decreased urethral resistance)
B. Overactive outlet (increased urethral resistance): overflow incontinence/retention; frequency–urgency.
1. Anatomical obstruction (physical blockage): increased outlet resistance
secondary to compression or narrowing.
2. Functional obstruction (failure of relaxation): increased outlet resistance–
inappropriate contraction or failure of normal relaxation.
3. Combined anatomical and functional obstruction
4. Inhibition of detrusor activity: increased pelvic floor activity: failure to relax
pelvic floor inhibits initiation of detrusor activity and inhibits ability to develop
or continue a sustained
(a) Neurological: (suprasacral) overactivity/hyperreflexia (dyssynergia pelvic floor
activity)
(b) Behavioural: failure to relax pelvic floor (learned, acquired, maladaptive,
psychogenic).
(c) Situational: “voluntary” inhibition secondary to environment or pain.
I. Outlet dysfunction: bladder outlet and pelvic floor
II. Bladder dysfunction
A. Detrusor overactivity (increased intravesical pressure)
Symptomatic: urgency incontinence (with or without sensation)– (OAB) wet.
B. Underactive bladder (decreased intravesical pressure)
Symptomatic: overflow incontinence/retention
III. Combined outlet and bladder dysfunction (I and II)
IV. Disorders of sensation:
A. Decreased sensation: denervation, myopathy, behavioral, pharmacological
B. Increased sensation: neuropathic, inflammatory, mucosal permeability defect, psychogenic,
afferent amplification
Assessment of Urethral Anatomy
Physical Examination
Ultrasound
Fluoroscopy (Videourodynamics): a diagnostic tool that incorporates urodynamics with simultaneous
imaging of the LUT during bladder filling & voiding for determining the site of bladder outlet
obstruction, the integrity of the sphincter mechanism, and the presence of VU reflux, bladder
diverticula, fistulae, and trabeculation
A. Detrusor External Sphincter Dyssynergia (DESD)
B. Acquired Voiding Dysfunction (AVD)—Hinman’s Syndrome
Abdominal Leak Point Pressure (ALPP): The lowest bladder pressure at which
leakage occurs, correlated with bladder volume, Cough vs. Valsalva to Measure
ALPP
Detrusor leak point pressure (DLPP)
Valsalva leak point pressure (VLPP)
1. Pura (Urethral Pressure) Profile = UPP (Urethral Pressure Profile):
provides information regarding the functional status of the urethra.
obtained under non-voiding conditions with the urethra at
rest
during coughing (stress Pura profile) and voiding
(micturition Pura profile) to obtain functional information
of the urethra
2. Retrograde Pura Profile: Urethral Retro-resistance Pressure (URP): the pressure
required to achieve and maintain an open sphincter
1. Elctromyogrphy (EMG) :
is the extracellular recording of bioelectrical activity generated by muscle fibers
is used to make the diagnosis of Detrusor External Sphincter Dyssynergia (DESD), and used
to distinguish the three types of DESD
EMG Changes After Vaginal Delivery : complicated vaginal delivery decreased
intramuscular nerve density in the urethral sphincter and decreased muscular tissue
incontinence and pelvic organ prolapse
2. Conduction Studies of The Sacral Motor System: Testing Conduction of Nerves and
Nervous Pathways Function
Three age tiers to the
Prevalence of prevalence of regular
incontinence (USA) incontinence in women
among women 60 years
• 15 to 34 years (4–5.5%)
and older living in the
• 35 to 74 years (8.8–11.9%)
community : 38% • 75 years and older (16–16.2%)
In Asia, the prevalence of UI in the study population was
14.8% (359/2422)
Nearly half of the incontinent individuals (47.9%) presented
with the mixed type.
81 women (22.6%) had stress incontinence
10% presented with urge incontinence
improve bladder control by teaching
patients skills for preventing urine
loss
Improving bladder function through
voiding schedules, such as with bladder
training
Another approach targets the bladder
outlet, such as pelvic floor muscle training
and exercise.
safe and without risks
side effects associated with
some other therapies
Bladder training is a behavioral intervention to break the cycle
of urgency and frequency using consistent and incremental
voiding schedules
Bladder training (BT) requires patients to resist the sensation of
urgency, to postpone voiding, and to urinate by the clock rather
than in response to an urge.
Mechanisms of action are bladder retraining improves cortical
inhibition over detrusor contractions, facilitates cortical ability
over urethral closure during bladder filling, strengthens pelvic
striated muscles, and alters behaviors that affect continence
Pelvic physiotherapy is often considered as first line treatment
In stress urinary incontinence (SUI), physiotherapy is especially aimed on strength
improvement and coordination of the periurethral and pelvic floor muscles (PFMs)
For detrusor overactivity,physiotherapy is aimed at the reduction or elimination of
involuntary detrusor muscle contractions through reflex inhibition.
Treatment modalities are patient information and education, toilet training, bladder
(re-)training, or behavioral therapy
Electrical stimulation, and magnetic stimulation. Especially, electrical therapy to be
an effective treatment modality.
In patients with detrusor overactivity electrical stimulation theoretically stimulates
the detrusor inhibition reflex (DIR) and pacifies the micturition reflex, resulting in a
decrease of overactive bladder dysfunction
LUT uropharmacology
addresses the innervations
and receptor contents of
the bladder, urethra, and
pelvic floor
S-ar putea să vă placă și
- LutsDocument24 paginiLutsJaneva SihombingÎncă nu există evaluări
- Stress IncontinenceDocument44 paginiStress IncontinenceswatisinghnigeriaÎncă nu există evaluări
- Urinary IncontinenceDocument14 paginiUrinary Incontinencehussain AltaherÎncă nu există evaluări
- Null - PDF 2Document30 paginiNull - PDF 2مهند حسام محمد سعيد عبدÎncă nu există evaluări
- Diagnosis & Management of Urinary Incontinence: G. M. Punarbawa RSUD Prov NTB/FK UNRAMDocument39 paginiDiagnosis & Management of Urinary Incontinence: G. M. Punarbawa RSUD Prov NTB/FK UNRAMfarlamayanti100% (1)
- Defecation NcbiDocument19 paginiDefecation NcbimuthiaÎncă nu există evaluări
- BladderDocument66 paginiBladderPatel Alapkumar Kanubhai100% (1)
- Detrusor InstabilityDocument7 paginiDetrusor Instabilityapi-3705046Încă nu există evaluări
- Hemorroid Shin2015Document9 paginiHemorroid Shin2015agusÎncă nu există evaluări
- Urinary IncontinenceDocument66 paginiUrinary Incontinencedr_asaleh100% (1)
- INCONTINENCE3Document12 paginiINCONTINENCE3allthingali217Încă nu există evaluări
- Neurogenic Bladder (Emedicine) : Physiology Filling PhaseDocument4 paginiNeurogenic Bladder (Emedicine) : Physiology Filling PhaseReni FahrianiÎncă nu există evaluări
- Sacral Neuromodulation For Bowel Dysfunction: Weledji EP and Marti LDocument11 paginiSacral Neuromodulation For Bowel Dysfunction: Weledji EP and Marti LPetrina Theda PhilothraÎncă nu există evaluări
- Urogynecology and Pelvic ReconstructionDocument28 paginiUrogynecology and Pelvic ReconstructionIKM FKUNSOEDÎncă nu există evaluări
- Canine Urinary IncontinenceDocument9 paginiCanine Urinary IncontinenceAsesino GuerreroÎncă nu există evaluări
- IncontinenceDocument9 paginiIncontinenceHanaÎncă nu există evaluări
- Inkontinensia UrinDocument24 paginiInkontinensia UrinBenny Wegah Nulis100% (9)
- The Blood Supply of EsophagusDocument4 paginiThe Blood Supply of EsophagusSaman SarKoÎncă nu există evaluări
- Neurogenic Bladder Dysfunction: Mariano Marcos State UniversityDocument6 paginiNeurogenic Bladder Dysfunction: Mariano Marcos State Universitychazney casianoÎncă nu există evaluări
- كوزرملا حاضو .د .م.أ لباب ةعماج/ بطلا ةيلك 2019 Urinary Incontinence. Involuntary loss of urine in sufficient amount or frequency to constituteDocument8 paginiكوزرملا حاضو .د .م.أ لباب ةعماج/ بطلا ةيلك 2019 Urinary Incontinence. Involuntary loss of urine in sufficient amount or frequency to constitutewzeer mohammedÎncă nu există evaluări
- Urinary IncontinenceDocument18 paginiUrinary IncontinenceShatha QudahÎncă nu există evaluări
- Presentation 3Document34 paginiPresentation 3Chidube UkachukwuÎncă nu există evaluări
- Lec.18 Genitourinary DysfunctionDocument37 paginiLec.18 Genitourinary Dysfunctionشريف محمد حسين شريف يوسفÎncă nu există evaluări
- Konsep Kebutuhan EliminasiDocument7 paginiKonsep Kebutuhan EliminasiFifi LestariÎncă nu există evaluări
- Assessment of The Urinary System: Chelsye Marviyouna Dearianto 1814201018Document19 paginiAssessment of The Urinary System: Chelsye Marviyouna Dearianto 1814201018Sinta WuLandariÎncă nu există evaluări
- Pathophysiology of Chronic ConstipationDocument7 paginiPathophysiology of Chronic Constipationcc vere100% (1)
- Fecal IncontinenceDocument57 paginiFecal Incontinenceiqiqiqiqiq100% (1)
- Aranilla-HW-Micturition-Dr. SalazarDocument3 paginiAranilla-HW-Micturition-Dr. SalazarHanako Sasaki AranillaÎncă nu există evaluări
- Urinary Incontinence: Genet Gebremedhin (MD) April 4 2017Document34 paginiUrinary Incontinence: Genet Gebremedhin (MD) April 4 2017bemnetÎncă nu există evaluări
- Ein Uti Kelompok 4Document21 paginiEin Uti Kelompok 4Eni MuslihahÎncă nu există evaluări
- GBHLN5 PR QHNP 5 Sy 5 CJDJ DFSDocument8 paginiGBHLN5 PR QHNP 5 Sy 5 CJDJ DFSyasmim16catarinaÎncă nu există evaluări
- Paralytic IleusDocument5 paginiParalytic IleusKimoy MacabungaÎncă nu există evaluări
- Urinary Incontinence in The Older Adult: by Kristen Cook, Pharm.D., BCPS and Linda M. Sobeski, Pharm.D., BCPSDocument18 paginiUrinary Incontinence in The Older Adult: by Kristen Cook, Pharm.D., BCPS and Linda M. Sobeski, Pharm.D., BCPSNurul HafizaÎncă nu există evaluări
- Neurogenic BladderDocument38 paginiNeurogenic Bladderminnalesri100% (1)
- Lec. 3 - Urogynaecology and Urinary ProlapseDocument9 paginiLec. 3 - Urogynaecology and Urinary ProlapseDr-Saja O. DmourÎncă nu există evaluări
- Diagnosis: 1 Lithotomy. The Labia Are Spread and The Protrusion Identified. The Patient Is Then AskedDocument3 paginiDiagnosis: 1 Lithotomy. The Labia Are Spread and The Protrusion Identified. The Patient Is Then AskedMona AryatiÎncă nu există evaluări
- Female Pelvic RelaxationDocument28 paginiFemale Pelvic RelaxationHafid IqbalÎncă nu există evaluări
- 25.2 Gross Anatomy of Urine Transport - Anatomy and Physiology 2e - OpenStaxDocument5 pagini25.2 Gross Anatomy of Urine Transport - Anatomy and Physiology 2e - OpenStaxMarlene AngwaforÎncă nu există evaluări
- Grand Rounds Index UTMB Otolaryngology Home PageDocument12 paginiGrand Rounds Index UTMB Otolaryngology Home Pagegdudex118811Încă nu există evaluări
- Urinary Incontinence in Elderly: DefinitionDocument13 paginiUrinary Incontinence in Elderly: DefinitionTarek AhmedÎncă nu există evaluări
- Amyotrophic Lateral Sclerosis (ALS)Document29 paginiAmyotrophic Lateral Sclerosis (ALS)Krisia Mhel Buyagao MollejonÎncă nu există evaluări
- Fecal IncontinenceDocument5 paginiFecal IncontinenceDaniel Galindo SotomayorÎncă nu există evaluări
- Urinary Incontinence HandoutDocument6 paginiUrinary Incontinence HandoutGautam ReddyÎncă nu există evaluări
- Sci Bladder ProtocolDocument45 paginiSci Bladder ProtocolAbbas JafarzadehabbasÎncă nu există evaluări
- Susah BabDocument45 paginiSusah BabaghniaÎncă nu există evaluări
- IncontinenceDocument9 paginiIncontinencehussain AltaherÎncă nu există evaluări
- Inkontinensia UrinDocument36 paginiInkontinensia UrinWhydia Wedha SutedjaÎncă nu există evaluări
- Genito Urinary AssessmentDocument31 paginiGenito Urinary AssessmentMuskan RastogiÎncă nu există evaluări
- Obstructed DefecationDocument35 paginiObstructed DefecationHerrDr MidoÎncă nu există evaluări
- 1-5-22 OMM Repro Considerations MasterDocument67 pagini1-5-22 OMM Repro Considerations MasterTanner HancockÎncă nu există evaluări
- Urinary Incontinence: 2 PathophysiologyDocument8 paginiUrinary Incontinence: 2 PathophysiologyZiedTrikiÎncă nu există evaluări
- Urinary Incontinence Has Sesven TypesDocument55 paginiUrinary Incontinence Has Sesven TypesDhonat Flash100% (1)
- Pelvic Organ ProlapseDocument9 paginiPelvic Organ ProlapseSonny Dizon PareñasÎncă nu există evaluări
- Lower Urinary Tract Symptoms (LUTS) in Middle-Aged and Elderly MenDocument6 paginiLower Urinary Tract Symptoms (LUTS) in Middle-Aged and Elderly MenIrfanArifZulfikarÎncă nu există evaluări
- Irregular Bowel HabitDocument66 paginiIrregular Bowel Habitfahim ahamedÎncă nu există evaluări
- Neurogenic Bladder: Mobility Clinic Case-Based Learning ModuleDocument11 paginiNeurogenic Bladder: Mobility Clinic Case-Based Learning ModuleJamaicaÎncă nu există evaluări
- Pathophysiology of Female LUTS: 1 Storage DysfunctionDocument10 paginiPathophysiology of Female LUTS: 1 Storage DysfunctionJaneva SihombingÎncă nu există evaluări
- Alteración MicciónDocument14 paginiAlteración MicciónMarie-charlotte CarrouxÎncă nu există evaluări
- Basic Gastroenterology: Including Diseases of the LiverDe la EverandBasic Gastroenterology: Including Diseases of the LiverÎncă nu există evaluări
- A Simple Guide to Disorders of Pelvic Floor Organs, Diagnosis, Treatment and Related ConditionsDe la EverandA Simple Guide to Disorders of Pelvic Floor Organs, Diagnosis, Treatment and Related ConditionsÎncă nu există evaluări
- BallardScore ScoresheetDocument1 paginăBallardScore ScoresheetIsabel BarradasÎncă nu există evaluări
- Daily Ok Igd Vai 140519Document26 paginiDaily Ok Igd Vai 140519Rakhmad HidayatÎncă nu există evaluări
- Lubchenco Curve PDFDocument1 paginăLubchenco Curve PDFWarren Lie25% (4)
- Pre Operative Planning MONDAY, December 31 2018: Resident On DutyDocument17 paginiPre Operative Planning MONDAY, December 31 2018: Resident On DutyRakhmad HidayatÎncă nu există evaluări
- GER Konkli 31.03.2019Document66 paginiGER Konkli 31.03.2019Rakhmad HidayatÎncă nu există evaluări
- Rekap Mingguan Stase Chief Poli GinekologiDocument2 paginiRekap Mingguan Stase Chief Poli GinekologiRakhmad HidayatÎncă nu există evaluări
- Daily Ok Igd Vai 140519Document26 paginiDaily Ok Igd Vai 140519Rakhmad HidayatÎncă nu există evaluări
- Absen Konsulen KosongDocument1 paginăAbsen Konsulen KosongRakhmad HidayatÎncă nu există evaluări
- Konkli Obsos VnyDocument1 paginăKonkli Obsos VnyRakhmad HidayatÎncă nu există evaluări
- Konkli Obsos Vny SlideDocument5 paginiKonkli Obsos Vny SlideRakhmad HidayatÎncă nu există evaluări
- Konkli 1 September Kai IbeDocument51 paginiKonkli 1 September Kai IbeRakhmad HidayatÎncă nu există evaluări
- Vaginal Misoprostol Compared With Buccal.20 PDFDocument6 paginiVaginal Misoprostol Compared With Buccal.20 PDFRakhmad HidayatÎncă nu există evaluări
- What Is New in Gynecologic Ultrasonography Best.31 PDFDocument3 paginiWhat Is New in Gynecologic Ultrasonography Best.31 PDFRakhmad HidayatÎncă nu există evaluări
- Myoma UterineDocument12 paginiMyoma Uterineevy_silviania8873Încă nu există evaluări
- Contraceptive Clinic, Lactation-Puerperal Outpatient and OperativeDocument13 paginiContraceptive Clinic, Lactation-Puerperal Outpatient and OperativeRakhmad HidayatÎncă nu există evaluări
- First Trimester Screening For AneuploidyDocument11 paginiFirst Trimester Screening For AneuploidyRakhmad HidayatÎncă nu există evaluări
- A Low-Costintervention To Improve The Management Ofeclamp SiaDocument5 paginiA Low-Costintervention To Improve The Management Ofeclamp SiaRakhmad HidayatÎncă nu există evaluări
- FIGOCEDocument11 paginiFIGOCEAldwin TanuwijayaÎncă nu există evaluări
- Vaginal Misoprostol Compared With Buccal.20Document6 paginiVaginal Misoprostol Compared With Buccal.20Rakhmad HidayatÎncă nu există evaluări
- What Is New in Gynecologic Ultrasonography Best.31Document3 paginiWhat Is New in Gynecologic Ultrasonography Best.31Rakhmad HidayatÎncă nu există evaluări
- Sources of Homeopathic DrugsDocument35 paginiSources of Homeopathic Drugsnadiida83% (6)
- Jordan University of Science and TechnologyDocument33 paginiJordan University of Science and TechnologyNourAldin AbuSalehÎncă nu există evaluări
- Trust Me, Im A (Junior) Doctor (Pemberton, Max (Pemberton, Max) )Document234 paginiTrust Me, Im A (Junior) Doctor (Pemberton, Max (Pemberton, Max) )Rakshith BalajiÎncă nu există evaluări
- OITE Review 2013Document263 paginiOITE Review 2013addison wood100% (2)
- Risk Factors Pathophysiology and Management of HypertensionDocument13 paginiRisk Factors Pathophysiology and Management of HypertensionDominggas RusunwullyÎncă nu există evaluări
- Raja Sir CampDocument6 paginiRaja Sir CampNivedan KothekarÎncă nu există evaluări
- Health Policy Memo MgenoviaDocument5 paginiHealth Policy Memo Mgenoviaapi-302138606Încă nu există evaluări
- Classification of Drugs Are: Hepatoprotective Drugs E.g.: Silymarin Antibiotics E.G.Document2 paginiClassification of Drugs Are: Hepatoprotective Drugs E.g.: Silymarin Antibiotics E.G.Navya Sara SanthoshÎncă nu există evaluări
- The ConjungtivaDocument111 paginiThe ConjungtivaLuvita Amallia SyadhatinÎncă nu există evaluări
- LorazepamDocument4 paginiLorazepamapi-3797941Încă nu există evaluări
- Rosen's Emergency Medicine Concepts and Clinical PracticeDocument15 paginiRosen's Emergency Medicine Concepts and Clinical PracticeMusdal RahmatÎncă nu există evaluări
- Be Happy Healthy Wealthy SAMPLEDocument30 paginiBe Happy Healthy Wealthy SAMPLERosie GonzalesÎncă nu există evaluări
- Leaflet Glycophos 1 (Spesifikasi Produk)Document2 paginiLeaflet Glycophos 1 (Spesifikasi Produk)Irhamna FauziahÎncă nu există evaluări
- Methods of ToiletDocument180 paginiMethods of Toiletathegeha100% (2)
- Health Sector EHSMS Requirements-June 2012Document31 paginiHealth Sector EHSMS Requirements-June 2012Aya MahmoudÎncă nu există evaluări
- Inguinal HerniaDocument9 paginiInguinal HerniaAmanda RapaÎncă nu există evaluări
- Chapter 7: Emotional and Behavioural Problems: DR Jessie EarleDocument28 paginiChapter 7: Emotional and Behavioural Problems: DR Jessie EarlejajmajÎncă nu există evaluări
- Rectal ProlapseDocument9 paginiRectal ProlapseAnjani Putri RetnaninggalihÎncă nu există evaluări
- HerbalismDocument18 paginiHerbalismmieÎncă nu există evaluări
- AJODO 1993 Facial Keys To Orth DX and TX Plann Part I ARNETTDocument14 paginiAJODO 1993 Facial Keys To Orth DX and TX Plann Part I ARNETTCarito Aguirre Lindo100% (1)
- Nursing Management HydrocephalusDocument4 paginiNursing Management HydrocephalusPrecious Mae Benologa100% (1)
- 10 Hip Replacement SurgeryDocument13 pagini10 Hip Replacement SurgeryDIA PHONG THANGÎncă nu există evaluări
- HbA1c - I Chrome DuoDocument3 paginiHbA1c - I Chrome DuoAnnisa Chaerani100% (1)
- What Is Speech TherapyDocument42 paginiWhat Is Speech Therapyiamoliver_31Încă nu există evaluări
- Ais YesDocument15 paginiAis YesLauriz Dillumas MachonÎncă nu există evaluări
- NSCA Tools and Resources PDFDocument3 paginiNSCA Tools and Resources PDFkunal mishraÎncă nu există evaluări
- ABR Workout GuideDocument13 paginiABR Workout GuideGJONES80100% (1)
- +bashkir State Medical UniversityDocument2 pagini+bashkir State Medical UniversityCB SharmaÎncă nu există evaluări
- Age-Related Dry Eye Lactoferrin and Lactobionic Acid: Mini ReviewDocument6 paginiAge-Related Dry Eye Lactoferrin and Lactobionic Acid: Mini ReviewldÎncă nu există evaluări
- FCBDocument26 paginiFCBsprapurÎncă nu există evaluări