Documente Academic
Documente Profesional
Documente Cultură
Neck Pain: MR Purnajyoti Banerjee FRCS (Orth)
Încărcat de
Madhusree Ghosh0 evaluări0% au considerat acest document util (0 voturi)
61 vizualizări30 pagini1) Neck pain is common, affecting 30-60% of adults during their lifetime. It is often caused by degeneration of the intervertebral discs or facet joints which can irritate nearby nerves.
2) Cervical radiculopathy occurs when a nerve root is compressed, typically causing pain that radiates into the arm. It may be caused by issues like disc herniation or bone spurs. Conservative care often provides relief but surgery may be considered if symptoms persist.
3) Cervical myelopathy results from spinal cord compression and can cause problems like difficulty walking. Timely surgery can help prevent further neurological decline if conservative options fail to provide relief from symptoms.
Descriere originală:
How to assess and mange neck pain in adults
Titlu original
Neck Pain
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PPTX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest document1) Neck pain is common, affecting 30-60% of adults during their lifetime. It is often caused by degeneration of the intervertebral discs or facet joints which can irritate nearby nerves.
2) Cervical radiculopathy occurs when a nerve root is compressed, typically causing pain that radiates into the arm. It may be caused by issues like disc herniation or bone spurs. Conservative care often provides relief but surgery may be considered if symptoms persist.
3) Cervical myelopathy results from spinal cord compression and can cause problems like difficulty walking. Timely surgery can help prevent further neurological decline if conservative options fail to provide relief from symptoms.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPTX, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
61 vizualizări30 paginiNeck Pain: MR Purnajyoti Banerjee FRCS (Orth)
Încărcat de
Madhusree Ghosh1) Neck pain is common, affecting 30-60% of adults during their lifetime. It is often caused by degeneration of the intervertebral discs or facet joints which can irritate nearby nerves.
2) Cervical radiculopathy occurs when a nerve root is compressed, typically causing pain that radiates into the arm. It may be caused by issues like disc herniation or bone spurs. Conservative care often provides relief but surgery may be considered if symptoms persist.
3) Cervical myelopathy results from spinal cord compression and can cause problems like difficulty walking. Timely surgery can help prevent further neurological decline if conservative options fail to provide relief from symptoms.
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPTX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 30
Neck pain
Mr Purnajyoti Banerjee FRCS (orth)
Introduction
• 30%-60% of adults experience significant neck
or radicular pain during lifetime
• Point prevalence 5-10%
• History of previous trauma to cervical spine
increases risk of developing significant axial
neck pain or radiculopathy
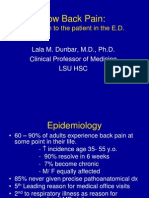
Epidemiology
• 30% + of population has significant neck pain
in lifetime
• ~15% of population with chronic neck pain of
> 6 months
• ~5% of population has disabling symptoms
Pathophysiology
• Afferent nociceptors in facet joint synovium and
degenerative intervertebral discs likely responsible for most
neck pain
• Loss of disc height, facet arthrosis, osteophyte formation,
and listhesis can all contribute to pathological loading of
facet joints and intervertebral disc
• Fibromyalgia may be perceived as neck pain, often localizes
to trapezium, associated with decreased blood flow, high
resting muscle tension and intramuscular metabolic
derangement
• Although controversial because of the potential for
secondary gain, cervical injury including whiplash as a risk
factor for axial neck pain
Axial neck pain
• Cervical injury may precede onset of neck pain
-Significant neck pain after trauma common even in
patients who have already settled resulting litigation
presumably decreasing secondary gain
• Axial neck pain should not be painful to palpation, and is
likely to be worse in extension and/or rotation
• Suboccipital pain suggests involvement of the occiput-C1 or
C1-C2 level
• Trigger points associated with fibromyalgia in the region of
the cervical spine are located in the: occiput, lateral aspect
of low cervical spine, trapezius and medial origin of the
supraspinatus
Physical examination
• Range of motion of cervical spine – often limited by
spondylosis
• Palpation of trigger points to evaluate for fibromyalgia
• Also: lateral condyle, medial knee joint line, greater
trochanter, medial 2nd rib and upper, outer quadrant of
buttocks
• Complete sensory, strength, gait and reflex evaluation
• Although a patient’s pain may be predominantly in the
neck, this does not preclude myelopathy or an
unrecognised motor deficit
Investigation
• Anteroposterior, lateral, and lateral flexion
and extension radiographs establish baseline
evaluations and may show dynamic instability
• MRI is gold standard for evaluation of disc
pathology such as annular injury, disc
dessication and facet arthritis
• Caution needed because of high prevalence of
findings in asymptomatic population
Natural History
• At 15 year follow-up with nonoperative care, 79% of patients had
symptom improvement in comparison to pain level at presentation
• 43% were pain-free, 32% had moderate/severe pain
• Factors associated with persistent pain:
- severe pain on presentation
-history of related injury
• Axial neck pain rarely progresses to myelopathy
• ~20% of patients presenting with severe pain will still be
significantly disabled at 5 years
Conservative treatment
• May include: steroids, NSAIDs, narcotics,
muscle-relaxants
• Physiotherapy
• Traction has not been shown to offer any
benefit
• Ill defined but can be beneficial with
favourable natural history
Surgical treatment
• Axial neck pain is a contraindication to cervical
disc replacement
• Anterior cervical discectomy and fusion is the
procedure of choice for carefully selected
patients who fail nonoperative treatment
• Retrospective studies report good/excellent
results in 60-80% with poor results in 5-20%
Cervical Radiculopathy
• Mechanical compression of nerve roots can result from several
causes:
- Loss of disc height, facet arthritis, uncovertebral joint osteophytes,
ligamentum flavum hypertrophy and disc herniation
• Chemical irritation of nerve roots occurs with exposure to
herniated nucleus pulposus mediated by TNF-alpha contained
within degenerative disc
• Foraminal stenosis and associated instability can cause symptom
worsening with extension or rotation to the ipsilateral side as the
neural foramen cross-sectional area decreases in these positions
• Conversely, arm abduction causes relative lengthening of cervical
roots and may result in pain relief
Presentation
• Patients typically present with pain in a
dermatomal distribution in upper extremity
• Pain may be burning, sharp or electric, can be
accompanied by motor weakness or sensory
changes
• Positional changes in foraminal area may lead
patients to turn their head to the opposite side or
abduct their arm overhead (shoulder abduction
sign)
• Neck pain also present in 80%
Physical examination
• Important to identify dermatomes/myotomes affected
through history and physical examination to treat only
symptomatic levels
• Spurling’s test – exacerbation of pain with extension
and rotation of head toward painful side
• Complete sensory, strength, gait and reflex evaluation
• Patients may present with concomitant myelopathy
• Pain, motor and sensory dysfunction can also result
from peripheral nerve entrapment and thoracic outlet
syndrome which must be ruled out
Investigations
• MRI is gold standard for evaluation of nerve
compression, pathology must correlate with
dermatomal complaints when indicating
surgery
• EMG useful to differentiate cervical from
peripheral nerve compression
Conservative treatment
• Natural History
• 70-90% of patients have good outcome with
nonoperative care
• Pain typically resolves within 6-12 weeks
• Conservative treatment
• Early treatment – brief course of opioiates if
necessary, brief immobilization with soft collar,
short steroid course may be helpful
• Later treatment may include: NSAIDs, muscle-
relaxants, physical therapy and stretching
Surgical management
• Anterior Approach – Fusion
- Indicated for soft disc herniation, bilateral
symptoms, significant neck pain, kyphotic cervical
alignment
- Usually not performed when addressing more
than 3 levels as nonunion rates rise unless posterior
instrumentation used
• Anterior Approach – Cervical Disc Replacement-
-Theoretical benefit of reducing adjacent level
disease
-Elimination of increased load seen by motion
segment adjacent to fusion, not yet proven
clinically
Posterior Approach
• Indicated for soft posterolateral HNP
– lateral recess or foraminal stenosis
– facet arthropathy with posterior compression
– > 3 level surgery
• Must have cervical lordosis for
decompression to be effective (> 10°)
Cervical Myelopathy
• Myelopathy likely with cord narrowing >40% or
banana-shaped cord on axial MRI images
• While degenerative changes often cause
myelopathy in older population (most common at
C5-6 and C6-7), younger patients may become
myelopathic due to untreated HNP
• Congenital stenosis (canal diameter <13mm
predisposes patients to myelopathy
• Gait and bladder disturbances likely secondary to
spinothalamic and cortico spinal tract
compression
Presentation
• May present with isolated myelopathy or with
radicular pain plus signs of cord compression
• Typical history often includes: difficulty
writing, trouble with buttons or zippers,
dropping objects, gait disturbances or
clumsiness, and falls
Physical examination
• Evaluation of gait and balance
• Repetitive tasks such as rapid tapping of thumb and index
finger pads or slapping thigh alternating between palm and
dorsum of hand will be difficult and slow in patients with
myelopathy
• Complete sensory, strength, and reflex evaluation
• May see clonus or hyperactive reflexes
• Radicular and myelopathic symptoms often coexist so can
find sensory or motor deficiencies on examination
• Special signs
- Lhermitte’s sign – electric pain in back of neck on flexion
- Babinski’s sign – great toe dorsiflexion on plantar stroke
- Hoffman’s reflex – thumb IP flexion with flicking of 3rd or
4th fingernail
Investigations
• Anteroposterior, lateral, and lateral flexion and
extension radiographs
• Pavlov ratio to screen for congenital stenosis
• AP diameter canal/AP diameter body <0.8 is
pathologic
• MRI is gold standard for evaluation of neural
impingement and may demonstrate cord signal
changes with severe compression
• Prognostic value of cord signal changes unclear,
however
Natural history
• Insidious onset of symptoms with long periods of
stability without deterioration
• These stable periods are punctuated by episodic
worsening of symptoms after which a new
functional baseline is established and function
rarely regained
• ~5% have rapid onset of symptoms with no
further progression
• Delay of 1 year in mild cases does not affect
surgical outcome
Conservative treatment
• Possible for elderly patients with minimal
symptoms and in patients with severe medical
co-morbidities
• May include: NSAIDs, physical therapy
• Patients with myelopathy should avoid
activities that will put them at risk for spinal
cord injury given the reduced tolerance for
trauma
Anterior approach
• Patients with mild symptoms may not benefit from
surgery,
• especially in the elderly
• Indications based around level of disability, degree of
pain
• Milder symptoms may be indication in younger
patients, those with evidence of congenital canal
stenosis on imaging
• Anterior surgical indications (ACDF or corpectomy):
-One to three affected levels
- Any number of levels with loss of cervical lordosis
-Should not be used for congenital stenosis or posterior
based cord compression
• Significant axial neck pain
Posterior surgery
• Laminectomy or laminoplasty:
- More than 3 affected levels with preserved
lordosis
- Cervical kyphosis with concomitant anterior
procedure
• Need wide decompression so
laminoforaminotomy not indicated
• Technique and surgical considerations same as for
radiculopathy
• Recovery of function depends on severity of
preoperative myelopathy
Thank you
Questions
S-ar putea să vă placă și
- Assessment of Racchimedular Injury by NursingDe la EverandAssessment of Racchimedular Injury by NursingÎncă nu există evaluări
- Management of Back Pain in AdultsDocument41 paginiManagement of Back Pain in AdultsMadhusree GhoshÎncă nu există evaluări
- Spinal Cord DisordersDocument50 paginiSpinal Cord DisordersIsaac Mwangi100% (1)
- Cervical Myelopathy - ERHDocument42 paginiCervical Myelopathy - ERHAries RHÎncă nu există evaluări
- LOW Back Pain: Pamela Rockwell, DODocument57 paginiLOW Back Pain: Pamela Rockwell, DODania ZaidÎncă nu există evaluări
- Pathology and Management of Low Back PainDocument33 paginiPathology and Management of Low Back PainSam100% (1)
- Spine Trauma: Dr. Elvira CesarenaDocument65 paginiSpine Trauma: Dr. Elvira CesarenadrelvÎncă nu există evaluări
- Neurological Aspect in Musculoskeletal Diseases Entrapment and CompressionDocument38 paginiNeurological Aspect in Musculoskeletal Diseases Entrapment and CompressionBakingpancakesÎncă nu există evaluări
- Low Back Pain HPNDocument39 paginiLow Back Pain HPNRussel Janolo100% (1)
- Dr. Yossi Maryanti, M.biomed, Sp. S - Neck and Back PainDocument50 paginiDr. Yossi Maryanti, M.biomed, Sp. S - Neck and Back PainFreade AkbarÎncă nu există evaluări
- Spinal Injury & Spinal Cord Injury: For General PracticeDocument60 paginiSpinal Injury & Spinal Cord Injury: For General PracticeRheselle LacuataÎncă nu există evaluări
- Spinal Deformities (Congenital)Document27 paginiSpinal Deformities (Congenital)deathmetal017Încă nu există evaluări
- Transverse MyelitisDocument18 paginiTransverse MyelitisNaveen KumarÎncă nu există evaluări
- Red Flag: MSK Services Pathway - Elbow PathologyDocument7 paginiRed Flag: MSK Services Pathway - Elbow PathologyMuhammed ElgasimÎncă nu există evaluări
- Kyphosis Lordosis Defined This Drawing Represents The Spinal Condition ofDocument36 paginiKyphosis Lordosis Defined This Drawing Represents The Spinal Condition ofSoare Elena-CosminaÎncă nu există evaluări
- Differential Diagnosis of Thoracic, Lumbar & Sacrum SpineDocument59 paginiDifferential Diagnosis of Thoracic, Lumbar & Sacrum Spinekashmala afzalÎncă nu există evaluări
- Assignment: Cervical SpondylosisDocument14 paginiAssignment: Cervical SpondylosisJaspreet kaurÎncă nu există evaluări
- Low Back Pain + Spinal StenosisDocument67 paginiLow Back Pain + Spinal StenosiswildanmalikÎncă nu există evaluări
- Carpal Tunnel Syndrome AntyDocument22 paginiCarpal Tunnel Syndrome Antyamel015Încă nu există evaluări
- 1 Materi Kuliah Spine, Dr. AzharuddinDocument59 pagini1 Materi Kuliah Spine, Dr. AzharuddinfazliahÎncă nu există evaluări
- Spinal InjuriesDocument65 paginiSpinal InjuriesDenuna EnjanaÎncă nu există evaluări
- Lower Back Pain: DR Robert Ramcharan MBBS, Frcsed, DM (Neurosurgery) NeurosurgeonDocument69 paginiLower Back Pain: DR Robert Ramcharan MBBS, Frcsed, DM (Neurosurgery) NeurosurgeonShimmering MoonÎncă nu există evaluări
- Anatomy 3Document52 paginiAnatomy 3Balsam TeineÎncă nu există evaluări
- Low Back Pain:: Approach To The Patient in The E.DDocument39 paginiLow Back Pain:: Approach To The Patient in The E.DLidiaAMonroyRÎncă nu există evaluări
- 43-44 - Muscuskeletal DisordersDocument39 pagini43-44 - Muscuskeletal DisordersTaif SalimÎncă nu există evaluări
- Meralgia ParestheticaDocument22 paginiMeralgia ParestheticaWahyu Tri KusprasetyoÎncă nu există evaluări
- Lumbar SpondylosisDocument59 paginiLumbar SpondylosisKURBULDKÎncă nu există evaluări
- Injuries Around The ShoulderDocument81 paginiInjuries Around The ShoulderMisoÎncă nu există evaluări
- Low Back Pain - 1-07Document39 paginiLow Back Pain - 1-07Nur Sabriany LihawaÎncă nu există evaluări
- Subaxial Cervical Spine TruamaDocument46 paginiSubaxial Cervical Spine TruamaWasim R. IssaÎncă nu există evaluări
- Principles of Management of Low Back Pain1Document39 paginiPrinciples of Management of Low Back Pain1Emmanuel DanielsÎncă nu există evaluări
- Slipped Capital Femoral EpiphysisDocument40 paginiSlipped Capital Femoral EpiphysisDrAshesh Desai100% (2)
- Lumbar Canal StenosisDocument19 paginiLumbar Canal StenosisMohamed ElMeligieÎncă nu există evaluări
- Chapter 7, Spine and Spinal Cord TraumaDocument26 paginiChapter 7, Spine and Spinal Cord TraumaAlen NotanubunÎncă nu există evaluări
- Neck Pain Or: Cervical SyndromeDocument13 paginiNeck Pain Or: Cervical SyndromeranikaikranÎncă nu există evaluări
- Medical Approach To Dizzy PatientsDocument52 paginiMedical Approach To Dizzy PatientsYudith Kattiarni Aisyah, MDÎncă nu există evaluări
- Spine Disease and Fractures For StudentsDocument79 paginiSpine Disease and Fractures For StudentsAbdullah MohdÎncă nu există evaluări
- 1 - Vestibular Disorders 1-13-16Document55 pagini1 - Vestibular Disorders 1-13-16lsucharlieÎncă nu există evaluări
- Spinal Cord InjuryDocument17 paginiSpinal Cord InjuryPrincess Gutierrez RositaÎncă nu există evaluări
- Low Back PainDocument53 paginiLow Back PainSahara EffendyÎncă nu există evaluări
- Cervical SpondylosisDocument26 paginiCervical SpondylosisAditya Anandito100% (2)
- Thoracic Outlet SyndromeDocument16 paginiThoracic Outlet SyndromeDeepak RajÎncă nu există evaluări
- Textbook Reading (THE SPINE BY ROTHMANDocument73 paginiTextbook Reading (THE SPINE BY ROTHMANLanny F. TjioeÎncă nu există evaluări
- Herniated Nucleus Pulposus TreatmentDocument19 paginiHerniated Nucleus Pulposus Treatmentvicky174Încă nu există evaluări
- Spinal Cord Injuries: Gabriel C. Tender, MDDocument49 paginiSpinal Cord Injuries: Gabriel C. Tender, MDCathyCarltonÎncă nu există evaluări
- Spinal Cord Injuries: Gabriel C. Tender, MDDocument49 paginiSpinal Cord Injuries: Gabriel C. Tender, MDGatotÎncă nu există evaluări
- Spinal Cord Injury: DR Sanjay Gupta SR Consultant NeurosurgeonDocument25 paginiSpinal Cord Injury: DR Sanjay Gupta SR Consultant Neurosurgeonsgupta_532847Încă nu există evaluări
- Low Back Pain Red Flags 1stBRAINSDocument59 paginiLow Back Pain Red Flags 1stBRAINSSofina Lusia HarahapÎncă nu există evaluări
- Handout Lat Elbow Pain PDFDocument47 paginiHandout Lat Elbow Pain PDFgemichan26Încă nu există evaluări
- Neck Pain and Lower Back Pain. Med Clin N Am. 2019.Document14 paginiNeck Pain and Lower Back Pain. Med Clin N Am. 2019.Jose Fernando Diez100% (1)
- Treatment of Cervical Spondylotic MyelopathyDocument49 paginiTreatment of Cervical Spondylotic MyelopathyencrownterÎncă nu există evaluări
- Whiplash Injury Spondylosis, Spondolysis and SpondylolisthesisDocument58 paginiWhiplash Injury Spondylosis, Spondolysis and SpondylolisthesistoobaÎncă nu există evaluări
- Spinal Cord InjuriesDocument49 paginiSpinal Cord Injuriesjustin_saneÎncă nu există evaluări
- Family Medicine DepartmentDocument45 paginiFamily Medicine Departmentسليمان فايزÎncă nu există evaluări
- Anesthetic Considerations in Patients Posted For Surgery With Ankylosing SpondylitisDocument43 paginiAnesthetic Considerations in Patients Posted For Surgery With Ankylosing Spondylitisanuk_1129Încă nu există evaluări
- Birth TraumaDocument57 paginiBirth TraumaAbu HajerahÎncă nu există evaluări
- REVISION TKR DR Hamad DammamDocument108 paginiREVISION TKR DR Hamad DammamFahad MÎncă nu există evaluări
- Lecture 6 Spinal Cord InjuriesDocument26 paginiLecture 6 Spinal Cord InjuriesMahroosh KhanÎncă nu există evaluări
- Kyphosis - Lecture 2013Document70 paginiKyphosis - Lecture 2013Dibyendunarayan BidÎncă nu există evaluări
- Birth Injuries: Julniar M Tasli Herman Bermawi Afifa RamadantiDocument30 paginiBirth Injuries: Julniar M Tasli Herman Bermawi Afifa RamadantiiqiqiqiqiqÎncă nu există evaluări
- Pyschiatric Nursing SummarizeDocument39 paginiPyschiatric Nursing SummarizeKyssel Seyer100% (1)
- Ayur MedicinesDocument21 paginiAyur Medicineskm_ananth100% (1)
- AtelectasisDocument9 paginiAtelectasisArni ZulsitaÎncă nu există evaluări
- Astrinita Lestari Suyata c11108174 STEMIDocument30 paginiAstrinita Lestari Suyata c11108174 STEMIjefrizalzainÎncă nu există evaluări
- AnophthalmaDocument17 paginiAnophthalmaMarvellous OkonobohÎncă nu există evaluări
- Dfs FSDF FSDFSDFDocument2 paginiDfs FSDF FSDFSDFJean ValjeanÎncă nu există evaluări
- Rizaldy M. Quitoriano, Petitioner, G.R. No. 179868Document6 paginiRizaldy M. Quitoriano, Petitioner, G.R. No. 179868danexrainierÎncă nu există evaluări
- Complet1e Bacteriology Notes From Levinson by Medical Study CenterDocument1 paginăComplet1e Bacteriology Notes From Levinson by Medical Study CenterGanesh NaikÎncă nu există evaluări
- Clerkship Case Write Up 2Document7 paginiClerkship Case Write Up 2Pir HarisÎncă nu există evaluări
- Narrative Report in School Clinic Sy 2018 - 2019Document8 paginiNarrative Report in School Clinic Sy 2018 - 2019Daiseree Salvador100% (7)
- PrognosisDocument8 paginiPrognosisallkhusairy6tuansiÎncă nu există evaluări
- The Essential Guide To The New FRCR Part 2A and Radiology BoardsDocument208 paginiThe Essential Guide To The New FRCR Part 2A and Radiology Boardsbana galaxyÎncă nu există evaluări
- Zang-Fu Syndrome Differentiation - UERMDocument113 paginiZang-Fu Syndrome Differentiation - UERMNathaniel P. Peralta0% (1)
- Pigeon Racing PigeonDocument7 paginiPigeon Racing Pigeonsundarhicet83Încă nu există evaluări
- Acupressure PointsDocument15 paginiAcupressure PointsVeda Thakkar100% (2)
- Practical Medical Microbiology PDFDocument5 paginiPractical Medical Microbiology PDFveena3Încă nu există evaluări
- NLE PreBoard QuestionsDocument73 paginiNLE PreBoard QuestionsAaron Johnson Fantastico JarrellÎncă nu există evaluări
- Biochemistry Reagents - ITA Kits - Promotional Tool 27th - August-2019-2Document23 paginiBiochemistry Reagents - ITA Kits - Promotional Tool 27th - August-2019-2Ajay DataniyaÎncă nu există evaluări
- NICUDocument190 paginiNICUsafasayedÎncă nu există evaluări
- Health Guide Lines For Ramadan FastingDocument4 paginiHealth Guide Lines For Ramadan Fastingmaidul.islamÎncă nu există evaluări
- FPSC No: 39 Mcqs On Submission Deadline: 5 April 2011: Oral Health in Primary CareDocument4 paginiFPSC No: 39 Mcqs On Submission Deadline: 5 April 2011: Oral Health in Primary Carev_vijayakanth7656100% (2)
- Pathophysiology MCQ With Answers PDFDocument4 paginiPathophysiology MCQ With Answers PDF02 Babar Saurabh NavnathÎncă nu există evaluări
- Mairs R Et Al 2016Document8 paginiMairs R Et Al 2016Camilla ValeÎncă nu există evaluări
- PCV Vaccine ProfileDocument6 paginiPCV Vaccine ProfileLhemmuel FiestaÎncă nu există evaluări
- 1.13.2 Clinical Localization and History in NeurologyDocument42 pagini1.13.2 Clinical Localization and History in Neurologyfikrah sharifÎncă nu există evaluări
- Number Surveyed Number Responding "Poor": ExercisesDocument2 paginiNumber Surveyed Number Responding "Poor": ExercisesJohn J. GómezÎncă nu există evaluări
- Comparison of Inflammatory Markers in HTNDocument6 paginiComparison of Inflammatory Markers in HTNDan JohnstonÎncă nu există evaluări
- Exercises PresentationDocument36 paginiExercises Presentationmeh wishÎncă nu există evaluări
- Laboratory Activity 9 Miley VirusDocument5 paginiLaboratory Activity 9 Miley VirusJade BalanÎncă nu există evaluări
- Gastritis in DogsDocument2 paginiGastritis in DogsPamela BriceñoÎncă nu există evaluări