Documente Academic
Documente Profesional
Documente Cultură
Communicable Diseases
Încărcat de
Raquel M. Mendoza0 evaluări0% au considerat acest document util (0 voturi)
10 vizualizări14 paginilecture
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PPTX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentlecture
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPTX, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
10 vizualizări14 paginiCommunicable Diseases
Încărcat de
Raquel M. Mendozalecture
Drepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPTX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 14
MALARIA
Vector-borne disease caused by protozoan parasites
called Plasmodium
Transmitted through the bite of an infected Anopheles
mosquito
May also be transmitted through transfusing blood
that is:
positive for malaria parasites
sharing of IV needles
transplacental mechanism
Malaria in the Philippines
Four Common Species of Malaria parasites in the
Philippines:
Plasmodium falciparum – 70% of malaria cases
Plasmodium vivax – 30% malaria cases
Plasmodium malariae
Plasmodium ovale
P. falciparum malaria, if not treated immediately, can
lead to severe malaria, such as cerebral malaria
P. vivax malaria does not lead to cerebral malaria but it
causes relapse if treatment was not completed
The adult female Anopheles mosquito that can
become infective and therefore carries the malaria
parasite after she bites a person infected with malaria
Bites from dusk to dawn and it breeds in clear, slow
flowing streams that are flow in mountainous/forested
areas or in brackish water where salt and fresh water
meet. This is usually found in coastal areas.
Certain Philippine municipalities of the 63 provinces
are endemic for malaria
Persons who are living in malaria endemic areas may
develop partial immunity to the disease
However, the may not manifest symptoms of malaria
but when their blood smear is examined under the
microscope, one can see malaria parasites in his/her
blood smear
Malaria Control Program
Utilizes a two-pronged approach to the control and
elimination of malaria:
Vector Control
use of chemically treated mosquito nets
larva-eating fish
environmental clean-up of stagnant water
use of anti-mosquito soap
chemoprophylaxis of chloroquine 1-2 weeks before
entering a high malaria-risk area continuous until 4-6
weeks after leaving the area
Second Strategy:
early detection and treatment of cases through early
recognition, prevention, and control of malaria
epidemics
requires the identification of a patient with malaria as
soon as he is examined
may be done through clinical signs and symptoms,
microscopic examination of blood smear, or a history
of visit or travel to an endemic or high malaria-risk
area
In the event of an imminent epidemic occurs:
mass blood smear collection
immediate confirmation and follow-up of cases
insecticide-treatment of mosquito nets must be done
Treatment for Malaria
Treated by taking the appropriate anti-malarial
medicines against the particular malaria species found
in the blood smear of the patient
A blood smear has to be done to find out what
particular species is present in the patient’s blood
It is also advised to complete the dosage of anti-
malarial medicine prescribed to the patient
At present, there is no vaccine against malaria.
However, malaria vaccine development is still on-
going
Preventive Measures against
Malaria
For those living in a malaria-risk area, the following are
recommended:
Sleep inside an insecticide-treated mosquito net every
night
Screen windows and doors or in the sleeping area
Wear long sleeves and long pants during night time
activities
Use insect repellant during night time activities
Consult immediately to the nearest health facility when
experiencing symptoms of malaria and complete the
medications as instructed. Do not self-medicate
For those persons who are going to a malaria endemic
area, the following may be necessary:
Consult the Provincial Health office or Rural Health
Unit of the province/area for medical advice
Chemoprophylaxis is given as follows:
o Doxycycline 100mg daily for 2-3days before going to
an endemic area, continue while in the endemic area
and continue for 4 more weeks after leaving the
endemic area
o Doxycycline is contraindicated in pregnant women
and children 8 years and below.
S-ar putea să vă placă și
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- 6 Infancy Diseases 1Document135 pagini6 Infancy Diseases 1Raquel M. MendozaÎncă nu există evaluări
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- Unit Ii Leadership in Nursing: A. Nurse in The OrganizationDocument25 paginiUnit Ii Leadership in Nursing: A. Nurse in The OrganizationRaquel M. MendozaÎncă nu există evaluări
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- 3 Problems With The Passenger and Powers of LaborDocument105 pagini3 Problems With The Passenger and Powers of LaborRaquel M. MendozaÎncă nu există evaluări
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- ExpandedroleofnursesDocument17 paginiExpandedroleofnursesRaquel M. MendozaÎncă nu există evaluări
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- FNCPDocument17 paginiFNCPRaquel M. MendozaÎncă nu există evaluări
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- Growth and Development of ChildrenDocument53 paginiGrowth and Development of ChildrenRaquel M. MendozaÎncă nu există evaluări
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- 1 The High Risk MotherDocument161 pagini1 The High Risk MotherRaquel M. MendozaÎncă nu există evaluări
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- Difference Between Adult and Fetal CirculationDocument6 paginiDifference Between Adult and Fetal CirculationRaquel M. MendozaÎncă nu există evaluări
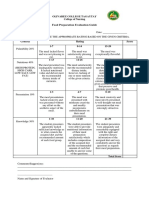
- Criteria Grading Scale Completion 5 4 3 2: Total PTS: 20Document1 paginăCriteria Grading Scale Completion 5 4 3 2: Total PTS: 20Raquel M. MendozaÎncă nu există evaluări
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Guidelines in PortfolioDocument3 paginiGuidelines in PortfolioRaquel M. Mendoza100% (1)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- Activity and Exercise PatternDocument20 paginiActivity and Exercise PatternRaquel M. MendozaÎncă nu există evaluări
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Sample Design Framework Data Types Units Variables Longitudinal Study ThemesDocument1 paginăSample Design Framework Data Types Units Variables Longitudinal Study ThemesRaquel M. MendozaÎncă nu există evaluări
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- Gordon's Functional Health AssessmentDocument11 paginiGordon's Functional Health AssessmentRaquel M. Mendoza100% (1)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
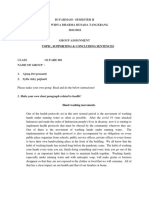
- Food Preparation Evaluation Guide: Olivarez College Tagaytay College of NursingDocument2 paginiFood Preparation Evaluation Guide: Olivarez College Tagaytay College of NursingRaquel M. MendozaÎncă nu există evaluări
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- Assessment of The Musculo-Skeletal SystemDocument46 paginiAssessment of The Musculo-Skeletal SystemRaquel M. MendozaÎncă nu există evaluări
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Grief, Loss, Death and DyingDocument47 paginiGrief, Loss, Death and DyingRaquel M. MendozaÎncă nu există evaluări
- Qualities of A Healthcare ProviderDocument6 paginiQualities of A Healthcare ProviderRaquel M. Mendoza50% (2)
- Practice Teaching A Reflective Approach Chap 7 Classroom Observation in Teaching PracticeDocument3 paginiPractice Teaching A Reflective Approach Chap 7 Classroom Observation in Teaching PracticeRaquel M. Mendoza0% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- Anatomy Physiology of Integumentary SystemDocument26 paginiAnatomy Physiology of Integumentary SystemRaquel M. Mendoza100% (1)
- Introduction To Environmental ScienceDocument34 paginiIntroduction To Environmental ScienceRaquel M. MendozaÎncă nu există evaluări
- Science, Matter, Energy and EcosystemsDocument43 paginiScience, Matter, Energy and EcosystemsRaquel M. MendozaÎncă nu există evaluări
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- Economics, Politics, Worldviews and The EnvironmentDocument17 paginiEconomics, Politics, Worldviews and The EnvironmentRaquel M. MendozaÎncă nu există evaluări
- Summary of BSN CoursesDocument3 paginiSummary of BSN CoursesRaquel M. MendozaÎncă nu există evaluări
- Internationalization of Higher Education InstitutionsDocument12 paginiInternationalization of Higher Education InstitutionsRaquel M. MendozaÎncă nu există evaluări
- ImplementingOutcome BasedEducationDocument11 paginiImplementingOutcome BasedEducationRaquel M. MendozaÎncă nu există evaluări
- Study Id71915 Coronavirus Covid 19 PhilippinesDocument61 paginiStudy Id71915 Coronavirus Covid 19 PhilippinesBarneyÎncă nu există evaluări
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Tis 5-Suspect - A - Urinary - Tract - Infection - Brochure - MA - Coalition - FinalDocument4 paginiTis 5-Suspect - A - Urinary - Tract - Infection - Brochure - MA - Coalition - FinalzaheerbdsÎncă nu există evaluări
- Certificat de Vaccinare Vaccination CertificateDocument2 paginiCertificat de Vaccinare Vaccination CertificateCorinaCerneiÎncă nu există evaluări
- Bfp9 Health Declaration FormDocument1 paginăBfp9 Health Declaration FormGelli Jane GurdielÎncă nu există evaluări
- Methodological Instructions - Module 2Document60 paginiMethodological Instructions - Module 2Frt TrfÎncă nu există evaluări
- Assessment Dianosis Planning Intervention Rationale EvaluationDocument2 paginiAssessment Dianosis Planning Intervention Rationale Evaluationkyaw100% (1)
- Dengue-WPS OfficeDocument20 paginiDengue-WPS OfficeAnnamalai MÎncă nu există evaluări
- Take On Tuberculosis InfographicDocument1 paginăTake On Tuberculosis InfographicJeane Irish EgotÎncă nu există evaluări
- Using Antimicrobial Agents To Control Mirobial Growth in VivoDocument39 paginiUsing Antimicrobial Agents To Control Mirobial Growth in VivoHannah BuquironÎncă nu există evaluări
- Handout CompilationDocument199 paginiHandout CompilationG Fab100% (2)
- 77 PAG LINKS-Danni-Vaccini PDFDocument77 pagini77 PAG LINKS-Danni-Vaccini PDFAntonio MartiniÎncă nu există evaluări
- ID RC Antimicrobial Stewardship Workbook 2022 FINAL T229141Document29 paginiID RC Antimicrobial Stewardship Workbook 2022 FINAL T229141Mohamed RatebÎncă nu există evaluări
- Asiclovir LeafletDocument1 paginăAsiclovir LeafletSiuuuÎncă nu există evaluări
- Tarun Kumar ReportDocument1 paginăTarun Kumar Reportnavdeep madheshiyaÎncă nu există evaluări
- Parasitic ArthropodsDocument3 paginiParasitic ArthropodsVicky V. HerpworldÎncă nu există evaluări
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- Zika Virus: Emerging Arboviral Threat To BangladeshDocument17 paginiZika Virus: Emerging Arboviral Threat To BangladeshlkokodkodÎncă nu există evaluări
- Literasi Bahasa Inggris - 260124Document2 paginiLiterasi Bahasa Inggris - 260124abcdefvinsÎncă nu există evaluări
- National Minimum Prevention MPPI GuideDocument20 paginiNational Minimum Prevention MPPI GuideEmmanuel Umo EffiongÎncă nu există evaluări
- 2 0CommDiseaseIMPTVisionDocument3 pagini2 0CommDiseaseIMPTVisionAndrea Patricia DaquialÎncă nu există evaluări
- Meningitis FinalDocument22 paginiMeningitis Finalshielamaygo05Încă nu există evaluări
- Introduction To Microbial Pathogenicity: Presented byDocument11 paginiIntroduction To Microbial Pathogenicity: Presented byAy GlassesÎncă nu există evaluări
- SyphilisDocument20 paginiSyphilisDhebra Mia Inot Suano100% (3)
- Group Task-Topic SentenceDocument2 paginiGroup Task-Topic SentenceajengdwiprasantiÎncă nu există evaluări
- Risk For Infection - NCPDocument3 paginiRisk For Infection - NCPHamil BanagÎncă nu există evaluări
- Clinical Microbiology Reviews-2002-Cox-595.full PDFDocument19 paginiClinical Microbiology Reviews-2002-Cox-595.full PDFMUHAMMAD IQBALÎncă nu există evaluări
- Unit Plan - 2018Document26 paginiUnit Plan - 2018Aparna AbyÎncă nu există evaluări
- Emerging & Re-Emerging Infections in India - An OverviewDocument19 paginiEmerging & Re-Emerging Infections in India - An Overviewjadu777Încă nu există evaluări
- Hepatitis B VaccineDocument3 paginiHepatitis B VaccineChoox PriiÎncă nu există evaluări
- URI Case (2 Lab Lecture) Patient Presentation: Chief ComplaintDocument2 paginiURI Case (2 Lab Lecture) Patient Presentation: Chief ComplaintMOHANNADÎncă nu există evaluări
- Rifqi Ben Bany - 3A: Patietn CaseDocument1 paginăRifqi Ben Bany - 3A: Patietn CaseRifqi Ben BanyÎncă nu există evaluări