Documente Academic
Documente Profesional
Documente Cultură
MENINGITIS
Încărcat de
Jobelle Acena0 evaluări0% au considerat acest document util (0 voturi)
17 vizualizări53 paginiTitlu original
MENINGITIS.pptx
Drepturi de autor
© © All Rights Reserved
Formate disponibile
PPTX, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPTX, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
17 vizualizări53 paginiMENINGITIS
Încărcat de
Jobelle AcenaDrepturi de autor:
© All Rights Reserved
Formate disponibile
Descărcați ca PPTX, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 53
MENINGITIS
• Meningitis is an inflammation of the membranes (meninges)
surrounding your brain and spinal cord.
• The swelling associated with meningitis often triggers the
"hallmark" signs and symptoms of this condition, including
headache, fever and a stiff neck.
• Most cases of meningitis in the U.S. are caused by a viral infection,
but bacterial and fungal infections also can lead to meningitis.
• Depending on the cause of the infection, meningitis can get better on
its own in a couple of weeks — or it can be a life-threatening
emergency requiring urgent antibiotic treatment.
• Early treatment of bacterial meningitis can prevent serious
complications.
Symptoms
• It's easy to mistake the early signs and symptoms of meningitis for the
flu (influenza).
• Meningitis signs and symptoms may develop over several hours or
over one or two days.
The signs and symptoms that may occur Signs in Newborns
in anyone older than age of 2 include:
• Sudden high fever Newborns and infants may not have
the classic signs and symptoms of
• Severe headache that isn't easily headache and stiff neck. Instead, signs
confused with other types of of meningitis in this age group may
headache include:
• Stiff neck • High fever
• Vomiting or nausea with headache • Constant crying
• Confusion or difficulty • Excessive sleepiness or irritability
concentrating • Inactivity or sluggishness
• Seizures • Poor feeding
• Sleepiness or difficulty waking up • A bulge in the soft spot on top of a
• Sensitivity to light baby's head (fontanel)
• Lack of interest in drinking and • Stiffness in a baby's body and neck
eating Infants with meningitis may be
difficult to comfort, and may even cry
• Skin rash in some cases, such as in harder when picked up.
meningococcal meningitis
Causes
• Meningitis usually results from a viral infection, but the cause may
also be a bacterial infection.
• Less commonly, a fungal infection may cause meningitis.
• Because bacterial infections are the most serious and can be life-
threatening, identifying the source of the infection is an important
part of developing a treatment plan.
Bacterial Meningitis
• Acute bacterial meningitis usually occurs when bacteria enter the
bloodstream and migrate to the brain and spinal cord. But it can also
occur when bacteria directly invade the meninges, as a result of an
ear or sinus infection, or a skull fracture, or rarely, after some
surgeries.
A number of strains of bacteria can cause acute bacterial meningitis. The most common include:
• Streptococcus pneumoniae (pneumococcus) - • Haemophilus influenzae (haemophilus) -
This bacterium is the most common cause of Haemophilus influenzae type b (Hib) bacterium
bacterial meningitis in infants, young children used to be the leading cause of bacterial
and adults in the United States. It more meningitis in children. But new Hib vaccines —
commonly causes pneumonia or ear or sinus available as part of the routine childhood
infections. There is a vaccine to help reduce the immunization schedule in the United States —
occurrence of this infection. have greatly reduced the number of cases of this
type of meningitis.
• Neisseria meningitidis (meningococcus) - This
bacterium is another leading cause of bacterial • Listeria monocytogenes (listeria) - These
bacteria can be found in soft cheeses, hot dogs
meningitis. Meningococcal meningitis
and luncheon meats. Fortunately, most healthy
commonly occurs when bacteria from an upper
people exposed to listeria don't become ill,
respiratory infection enter your bloodstream. although pregnant women, newborns, older
This infection is highly contagious. It affects adults and people with weakened immune
mainly teenagers and young adults, and may systems tend to be more susceptible. Listeria
cause local epidemics in college dormitories, can cross the placental barrier, and infections in
boarding schools and military bases. There is a late pregnancy may cause a baby to be stillborn
vaccine to help reduce the occurrence of this or die shortly after birth. People with weakened
infection. immune systems, due to disease or medication
effect, are most vulnerable.
Viral Meningitis
• Each year, viruses cause a greater number of cases of meningitis than
do bacteria.
• Viral meningitis is usually mild and often clears on its own.
• A group of viruses known as enteroviruses is responsible for most
viral meningitis cases in the United States.
• These viruses tend to circulate in late summer and early fall.
• Viruses such as herpes simplex virus, HIV, mumps, West Nile virus and
others also can cause viral meningitis.
Fungal Meningitis
• Fungal meningitis is relatively uncommon and causes chronic
meningitis.
• Occasionally it can mimic acute bacterial meningitis.
• However, this form of meningitis isn't contagious from person to
person.
• Cryptococcal meningitis is a common fungal form of the disease that
affects people with immune deficiencies, such as AIDS.
• It's life-threatening if not treated with an antifungal medication.
• In 2012, fungal meningitis made the news because contaminated
corticosteroid injections caused a multistate outbreak.
• Fungal meningitis cases were associated with contaminated
medication injected into the spine for back or neck pain.
Other Meningitis Causes
• Meningitis can also result from noninfectious causes, such as
chemical reactions, drug allergies, some types of cancer and
inflammatory diseases such as sarcoidosis.
Risk Factors
• Skipping vaccinations. An individual hasn't completed the recommended
childhood or adult vaccination schedule, the risk of meningitis is higher.
• Age. Most cases of viral meningitis occur in children younger than age 5. Bacterial
meningitis commonly affects people under 20, especially those living in
community settings.
• Living in a community setting. College students living in dormitories, personnel
on military bases, and children in boarding schools and child care facilities are at
increased risk of meningococcal meningitis. This increased risk likely occurs
because the bacterium is spread by the respiratory route and tends to spread
quickly wherever large groups congregate.
• Pregnancy. If a pregnant, or an individual at increased risk of contracting
listeriosis — an infection caused by listeria bacteria, which also may cause
meningitis. If a pregnant has listeriosis, her unborn baby is at risk, too.
• Compromised immune system. Factors that may compromise immune system —
including AIDS, alcoholism, diabetes and use of immunosuppressant drugs — also
make more susceptible to meningitis. Removal of spleen, an important part of
immune system, also may increase risk.
Diagnosis
• Blood cultures. Blood drawn from a vein • Spinal tap (lumbar puncture). The
is sent to a laboratory and placed in a definitive diagnosis of meningitis requires
an analysis of the cerebrospinal fluid (CSF),
special dish to see if it grows which is collected during a procedure
microorganisms, particularly bacteria. A known as a spinal tap. In people with
sample may also be placed on a slide to meningitis, the CSF fluid often shows a low
sugar (glucose) level along with an
which stains are added (Gram's stain), increased white blood cell count and
then examined under a microscope for increased protein.
bacteria. • CSF analysis may also help the doctor
• Imaging. X-rays and computerized identify the exact bacterium that's causing
the illness. If the doctor suspects viral
tomography (CT) scans of the head, chest meningitis, he may order a DNA-based
or sinuses may reveal swelling or test known as a polymerase chain reaction
inflammation. These tests can also help (PCR) amplification or a test to check for
antibodies against certain viruses to check
the doctor look for infection in other for the specific causes of meningitis. This
areas of the body that may be associated helps to determine proper treatment and
with meningitis. prognosis.
Treatment
The treatment depends on the type of meningitis.
Bacterial meningitis
• Acute bacterial meningitis requires prompt treatment with intravenous antibiotics and,
more recently, cortisone medications, to ensure recovery and reduce the risk of
complications, such as brain swelling and seizures. The antibiotic or combination of
antibiotics that the doctor may choose depends on the type of bacteria causing the
infection. The doctor may recommend a broad-spectrum antibiotic until he can
determine the exact cause of the meningitis.
• Infected sinuses or mastoids — the bones behind the outer ear that connect to the
middle ear — may need to be drained.
Viral meningitis
• Antibiotics can't cure viral meningitis, and most cases improve on their own in several
weeks. Treatment of mild cases of viral meningitis usually includes:
• Bed rest
• Plenty of fluids
• Over-the-counter pain medications to help reduce fever and relieve body aches
• If the cause of your meningitis is a herpes virus, an antiviral medication is available.
Other types of meningitis
• If the cause of the meningitis is unclear, the doctor may start antiviral and
antibiotic treatment while a cause is being determined.
• Fungal meningitis is treated with antifungal medications. However, these
medications can have serious side effects, so treatment may be deferred
until a laboratory can confirm that the cause is fungal. Chronic meningitis is
treated based on the underlying cause, which is often fungal.
• Noninfectious meningitis due to allergic reaction or autoimmune disease
may be treated with cortisone medications. In some cases, no treatment
may be required, because the condition can resolve on its own. Cancer-
related meningitis requires therapy for the individual cancer
FEBRILE SEIZURE
• A febrile seizure is a convulsion in a child triggered by a fever.
Causes
• A febrile seizure can be very frightening for any parent or caregiver.
• Most of the time, a febrile seizure does not cause any harm and the
child usually does not have a more serious long-term health problem.
• Febrile seizures occur most often in otherwise healthy children
between ages 9 months and 5 years.
• Toddlers are most commonly affected.
• Febrile seizures often run in families.
• Most febrile seizures occur in the first 24 hours of an illness, and may
not occur when the fever is highest.
• Ear infections, a cold or viral illness may trigger a febrile seizure.
Symptoms
• A febrile seizure may be as mild as the child's eyes rolling or limbs
stiffening.
• A simple febrile seizure stops by itself within a few seconds to 10 minutes.
It is often followed by a brief period of drowsiness or confusion.
• Symptoms may include any of the following:
• Sudden tightening (contraction) of muscles on both sides of a child's
body. The muscle tightening may last for several seconds or longer.
• The child may cry or moan.
• If standing, the child will fall.
• The child may vomit or bite their tongue.
• Sometimes, children do not breathe and may begin to turn blue.
• The child's body may then begin to jerk rhythmically. The child will not
respond to the parent's voice.
• Urine may be passed.
• A seizure lasting longer than 15 minutes, is in just one part of the
body, or occurs again during the same illness is not a normal febrile
seizure.
• The health care provider may diagnose febrile seizure if the child has
a grand mal seizure but does not have a history of seizure disorders
(epilepsy).
• A grand mal seizure involves the entire body.
• In infants and young children, it is important to rule out other causes
of a first-time seizure, especially meningitis (bacterial infection of the
covering of the brain and spinal cord).
Diagnosis
• With a typical febrile seizure, the examination usually is normal, other than
symptoms of the illness causing the fever.
• Often, the child will not need a full seizure workup, which includes an EEG,
head CT, and lumbar puncture (spinal tap).
• Further testing may be needed if the child:
• Is younger than 9 months or older than 5 years.
• Has a brain, nerve, or developmental disorder.
• Had the seizure in only one part of the body.
• Had the seizure last longer than 15 minutes.
• Had more than one febrile seizure in 24 hours.
• Has abnormal findings when examined.
Treatment
• During the seizure, take the following measures to keep the child safe:
• Do not restrain the child or try to stop the seizure movements.
• Lay the child on the ground in a safe area. Clear the area of furniture or
other sharp objects.
• Slide a blanket under the child if the floor is hard.
• Move the child only if they are in a dangerous location.
• Loosen tight clothing, especially around the neck. If possible, open or
remove clothes from the waist up.
• If the child vomits or if saliva and mucus build up in the mouth, turn the
child to the side or on the stomach. This is also important if it looks like
the tongue is getting in the way of breathing.
• Do not force anything into the child's mouth to prevent biting the
tongue. This increases the risk of injury.
• Focus your attention on bringing the fever down:
• Insert an acetaminophen suppository (if there is some) into the child's
rectum.
• Do not give anything by mouth.
• Apply cool washcloths to the forehead and neck. Sponge the rest of the
body with lukewarm (not cold) water. Cold water or alcohol can make
the fever worse.
• After the seizure is over and your child is awake, give the normal dose
of ibuprofen or acetaminophen.
• After the seizure, the most important step is to identify the cause of the
fever.
• Meningitis can cause a few cases of febrile seizures. It should always be
considered, especially in children younger than 1 year old, or in children
who still look ill when the fever comes down.
WILM’S TUMOR
• Wilms' tumor is a rare kidney cancer that primarily affects children.
• Also known as nephroblastoma, Wilms' tumor is the most common
cancer of the kidneys in children.
• Wilms' tumor most often affects children ages 3 to 4 and becomes
much less common after age 5.
• Wilms' tumor most often occurs in just one kidney, though it can
sometimes be found in both kidneys at the same time.
• Improvements in the diagnosis and treatment of Wilms' tumor have
improved the prognosis for children with this disease.
• The outlook for most children with Wilms' tumor is very good.
Symptoms
• Wilms' tumor doesn't always cause signs and symptoms.
• Children with Wilms' tumor may appear healthy, or they may experience:
• Abdominal swelling
• An abdominal mass you can feel
• Abdominal pain
• Fever
• Blood in the urine or discoloration of urine
• Constipation
• Abdominal discomfort
• Nausea
• Loss of appetite
• High blood pressure
• Increase and uneven growth of one side of body
Causes
• It's not clear what causes Wilms' tumor.
• Doctors know that cancer begins when cells develop errors in their
DNA.
• The errors allow the cells to grow and divide uncontrollably and to go
on living when other cells would die.
• The accumulating cells form a tumor. In Wilms' tumor, this process
occurs in the kidney cells.
• In a small number of cases, the errors in DNA that lead to Wilms'
tumor are passed from parents to children.
• In most cases, there is no known connection between parents and
children that may lead to cancer
• In most cases, Wilms tumor cannot be linked to a specific cause.
• Studies are under way to determine whether environmental factors,
such as drugs, chemicals, or infectious agents, can cause Wilms
tumor.
• Some children have genetic factors that increase their risk of
developing the disease, including certain syndromes that are
associated with Wilms tumor.
• One such condition is Beckwith-Wiedemann syndrome, which is a
growth disorder that causes body and organ enlargement.
• Other abnormalities associated with this cancer include a missing iris
in the eye and the enlargement of one side of the body.
Risk Factors
• Factors that may increase the risk of Wilms' tumor include:
• Being black. Black children have a slightly higher risk of developing Wilms' tumor
than do children of other races. Children of Asian descent appear to have a lower
risk than do children of other races.
• Having a family history of Wilms' tumor. If someone in your child's family has had
Wilms' tumor, then your child has an increased risk of developing the disease.
• Wilms' tumor occurs more frequently in children with certain abnormalities present at
birth, including:
• Aniridia. In this condition the iris — the colored portion of the eye — forms only
partially or not at all.
• Hemihypertrophy. A condition that occurs when one side of the body is noticeably
larger than the other side.
• Undescended testicles. One or both testicles fail to descend into the scrotum
(cryptorchidism).
• Hypospadias. The urinary (urethral) opening is not at the tip of the penis, but is on
the underside.
• Wilms' tumor can occur as part of rare syndromes, including:
• WAGR syndrome. This syndrome includes Wilms' tumor, aniridia,
abnormalities of the genitals and urinary system, and mental
retardation.
• Denys-Drash syndrome. This syndrome includes Wilms' tumor,
kidney disease and male pseudohermaphroditism, in which a boy
is born with testicles but may exhibit female characteristics.
• Beckwith-Wiedemann syndrome. Signs of this syndrome include
abdominal organs that protrude into the base of the umbilical
cord, a large tongue (macroglossia) and enlarged internal organs.
Diagnosis
• To diagnose Wilms' tumor, the child's doctor may recommend:
• A physical examination. The doctor will look for possible signs of
Wilms' tumor.
• Blood and urine tests. Blood tests can't detect Wilms' tumor, but they
can provide the child's doctor with an overall assessment of the child's
health.
• Imaging tests. Imaging tests that create images of the child's kidneys
can help the doctor determine whether the child has a kidney tumor.
Imaging tests may include ultrasound, computerized tomography (CT)
and magnetic resonance imaging (MRI).
• Surgery. If the child has a kidney tumor, the doctor may recommend
removing the tumor or the entire kidney to determine if the tumor is
cancerous. The removed tissue is analyzed in a laboratory to determine
whether cancer is present and what types of cells are involved. This
surgery may also serve as treatment for Wilms' tumor.
Staging
• Once the child's doctor has diagnosed Wilms' tumor, he works to determine the
extent (stage) of the cancer. The child's doctor may recommend a chest X-ray,
chest CT scan and bone scan to determine whether the cancer has spread beyond
the kidneys.
• The doctor assigns the child's cancer a stage, which helps determine the
treatment options. The stages of Wilms' tumor are:
• Stage I. The cancer is found only in one kidney and generally can be completely
removed with surgery.
• Stage II. The cancer has spread to the tissues and structures near the affected
kidney, such as fat or blood vessels, but it can still be completely removed by
surgery.
• Stage III. The cancer has spread beyond the kidney area to nearby lymph
nodes or other structures within the abdomen, and it may not be completely
removed by surgery.
• Stage IV. The cancer has spread to distant structures, such as the lungs, liver,
bones or brain.
• Stage V. Cancer cells are found in both kidneys.
Treatment
• Treatment for Wilms' tumor usually involves surgery and
chemotherapy.
• But treatments may vary by the stage of the cancer.
• Because this type of cancer is rare, the doctor may recommend that
you seek treatment at a children's cancer center that has experience
treating this type of cancer.
Surgery to remove all or part of a kidney
• Treatment for Wilms' tumor usually begins with surgery to remove all or part of a kidney
(nephrectomy). Surgery is also used to confirm the diagnosis, since the tissue removed
during surgery is sent to a laboratory to determine whether it is cancerous.
• Surgery for Wilms' tumor may include:
• Removing part of the affected kidney. Partial nephrectomy involves removal of the
tumor and part of the kidney tissue surrounding it. Partial nephrectomy may be an
option if your child's cancer is very small or if your child has only one functioning
kidney.
• Removing the affected kidney and surrounding tissue. In a radical nephrectomy,
doctors remove the kidney and surrounding tissues, including the ureter and adrenal
gland. Neighboring lymph nodes also may be removed. The remaining kidney can
increase its capacity and take over the entire job of filtering the blood.
• Removing all or part of both kidneys. If your child's cancer affects both kidneys, the
surgeon works to remove as much cancer as possible from both kidneys. In a small
number of cases, this may mean removing both kidneys, which means your child
would then undergo kidney dialysis. A kidney transplant may be an option so that your
child will no longer need dialysis.
• Chemotherapy
• Chemotherapy uses powerful drugs to kill cancer cells throughout
the body. Chemotherapy treatment usually involves a combination
of drugs that work together to kill cancer cells. Chemotherapy can
be administered through a vein or taken in pill form.
• Radiation therapy
• Radiation therapy uses high-energy beams, such as X-rays, to kill
cancer cells.
CEREBRAL PALSY
• Cerebral palsy is a disorder of movement, muscle tone or posture that
is caused by an insult to the immature, developing brain, most often
before birth.
• Signs and symptoms appear during infancy or preschool years. In
general, cerebral palsy causes impaired movement associated with
exaggerated reflexes, floppiness or rigidity of the limbs and trunk,
abnormal posture, involuntary movements, unsteadiness of walking,
or some combination of these.
• People with cerebral palsy may have difficulty with swallowing and
commonly have eye muscle imbalance. People with cerebral palsy
may have reduced range of motion at various joints of their bodies
due to muscle stiffness.
• The effect of cerebral palsy on functional abilities varies greatly. Some
people are able to walk while others aren't able to walk. Some people
show normal to near normal intellectual function, but others may
have intellectual disabilities. Epilepsy, blindness or deafness also may
be present.
• People with cerebral palsy often have underlying developmental brain
abnormalities.
Symptoms
• Signs and symptoms can vary greatly. • Delays in reaching motor skills
Movement and coordination problems milestones, such as pushing up on
associated with cerebral palsy may arms, sitting up alone or crawling
include: • Favoring one side of the body, such as
• Variations in muscle tone, such as reaching with only one hand or
being either too stiff or too floppy dragging a leg while crawling
• Stiff muscles and exaggerated reflexes • Difficulty walking, such as walking on
(spasticity) toes, a crouched gait, a scissors-like
• Stiff muscles with normal reflexes gait with knees crossing or a wide gait
(rigidity) • Difficulty with sucking or eating
• Lack of muscle coordination (ataxia) • Delays in speech development or
• Tremors or involuntary movements difficulty speaking
• Slow, writhing movements (athetosis) • Difficulty with precise motions, such
as picking up a crayon or spoon
• Excessive drooling or problems with
swallowing
• The disability associated with cerebral palsy may be limited primarily to one limb
or one side of the body, or it may affect the whole body.
• The brain disorder causing cerebral palsy doesn't change with time, so the
symptoms usually don't worsen with age, although the shortening of muscles and
muscle rigidity may worsen if not treated aggressively.
• Other neurological problems
• Brain abnormalities associated with cerebral palsy also may contribute to
other neurological problems. People with cerebral palsy may also have:
• Difficulty with vision and hearing
• Intellectual disabilities
• Seizures
• Abnormal touch or pain perceptions
• Oral diseases
• Mental health (psychiatric) conditions
• Urinary incontinence
Causes
• Cerebral palsy is caused by an abnormality or disruption in brain
development, usually before a child is born. In many cases, the exact
trigger of this abnormality isn't known.
• Factors that may lead to problems with brain development include:
• Random mutations in genes that control brain development.
• Maternal infections that affect the developing fetus.
• Fetal stroke, a disruption of blood supply to the developing brain.
• Lack of oxygen to the brain (asphyxia) related to difficult labor or
delivery. This is rarely a cause.
• Infant infections that cause inflammation in or around the brain.
• Traumatic head injury to an infant from a motor vehicle accident
or fall.
Risk Factors
• A number of factors are associated with an increased risk of cerebral
palsy.
Maternal Health
• Certain infections or health problems during pregnancy can significantly increase
the risk of giving birth to a baby with cerebral palsy. Infections of particular
concern include:
• German measles (rubella). Rubella is a viral infection that can cause serious
birth defects. It can be prevented with a vaccine.
• Chickenpox (varicella). Chickenpox is a contagious viral infection that causes
itching and rashes, and it can cause pregnancy complications. It can be
prevented with a vaccine.
• Cytomegalovirus. Cytomegalovirus is a common virus that causes flu-like
symptoms and may lead to birth defects if a mother experiences her first active
infection during pregnancy.
• Toxoplasmosis. Toxoplasmosis is a parasitic infection caused by a parasite
found in contaminated food, soil and the feces of infected cats.
• Syphilis. Syphilis is a sexually transmitted bacterial infection.
• Exposure to toxins. Exposure to toxins, such as methyl mercury, can increase
the risk of birth defects.
• Other conditions. Other conditions may increase the risk of cerebral palsy, such
as thyroid problems, intellectual disabilities or seizures.
Infant Illness
• Illnesses in a newborn baby that can greatly increase the risk of cerebral
palsy include:
• Bacterial meningitis. This is a bacterial infection that causes inflammation
in the membranes that surround the brain and spinal cord.
• Viral encephalitis. This viral infection causes inflammation in the
membranes that surround the brain and spinal cord.
• Severe or untreated jaundice. Jaundice is a condition that appears as a
yellowing of the skin. Jaundice occurs when certain byproducts of "used"
blood cells aren't filtered from the bloodstream.
Other Factors of Pregnancy and Birth
• Other factors of pregnancy or birth that are associated with an increased risk
of cerebral palsy include:
• Premature birth. A normal pregnancy lasts 40 weeks. Babies who are
born fewer than 37 weeks into the pregnancy are at higher risk of
cerebral palsy. The earlier the baby is born, the greater the risk of cerebral
palsy.
• Low birth weight. Babies who weigh less than 5.5 pounds (2.5 kilograms)
are at higher risk of developing cerebral palsy. This risk increases as birth
weight drops.
• Breech births. Babies with cerebral palsy are more likely to be in a feet-
first position (breech presentation) at the beginning of labor rather than
in a headfirst position.
• Multiple babies. The risk of cerebral palsy increases with the number of
babies sharing the uterus. If one or more of the babies die, the chance
that the survivors may have cerebral palsy increases.
Diagnosis
• If the doctor or pediatrician suspects that the child has cerebral palsy,
he will evaluate the child's signs and symptoms, review the child's
medical history, and conduct a physical evaluation.
• The doctor may refer to a doctor trained in treating children with
brain and nervous system conditions (pediatric neurologist).
• The doctor will also order a series of tests to make a diagnosis and
rule out other possible causes.
BRAIN SCANS
• Brain-imaging technologies can reveal areas of damage or abnormal development in
the brain. These tests may include the following:
• Magnetic resonance imaging (MRI). An MRI uses radio waves and a magnetic field
to produce detailed 3-D or cross-sectional images of your child's brain. An MRI can
often identify any lesions or abnormalities in your child's brain.
This test is painless, but it's noisy and can take up to an hour to complete. The child
will likely receive a mild sedative before the test. An MRI is usually the preferred
imaging test.
• Cranial ultrasound. This can be obtained during infancy. A cranial ultrasound uses
high-frequency sound waves to obtain images of the brain. An ultrasound doesn't
produce a detailed image, but it may be used because it's quick and inexpensive,
and it can provide a valuable preliminary assessment of the brain.
• Computerized tomography (CT) scan. A CT scan uses X-rays to obtain cross-
sectional images of your child's brain. A CT scan may be used to identify
abnormalities in your child's brain.
Scanning is painless and takes about 20 minutes. Because your child will need to be
very still during the test, he or she will likely receive a mild sedative.
ELECTROENCEPHALOGRAM (EEG)
• If the child has had seizures, the doctor may order an
electroencephalogram (EEG) to determine if he has epilepsy, which
often occurs in people with cerebral palsy. In an EEG test, a series of
electrodes are affixed to the child's scalp.
• The EEG records the electrical activity of the child's brain. If he has
epilepsy, it's common for there to be changes in normal patterns of
brain waves.
LABORATORY TESTS
• The child's blood may need to be checked to rule out other
conditions, such as blood-clotting disorders that can cause strokes,
which may mimic cerebral palsy signs and symptoms. Laboratory tests
may also screen for genetic or metabolic problems.
ADDITIONAL TESTS
• If the child is diagnosed with cerebral palsy, he'll likely be referred to
specialists for assessments of other conditions that are often
associated with the disorder. These tests may identify:
• Vision impairment
• Hearing impairment
• Speech delays or impairments
• Intellectual disabilities
• Other developmental delays
• Movement disorders
Treatment
• Children and adults with cerebral palsy require long-term care with a
medical care team. This team may include:
• Pediatrician or physiatrist. A pediatrician oversees the treatment plan
and medical care.
• Pediatric neurologist. A doctor trained in diagnosing and treating
children with brain and nervous system (neurological) disorders may be
involved in your child's care.
• Orthopedic surgeon. A doctor trained in treating muscle and bone
disorders may be involved in diagnosing and treating muscle conditions.
• Physical therapist. A physical therapist may help your child improve
strength and walking skills, and stretch muscles.
• Occupational therapist. An occupational therapist can provide therapy
to your child to develop daily skills and to learn to use adaptive
products that help with daily activities.
• Speech-language pathologist. A doctor trained in diagnosing and
treating speech and language disorders may work with your child if your
child has difficulties with speech, swallowing or language.
• Developmental therapist. A developmental therapist may provide
therapy to help your child develop age-appropriate behaviors, social
skills and interpersonal skills.
• Mental health specialist. A mental health specialist, such as a
psychologist or psychiatrist, may be involved in your child's care. He or
she may help you and your child learn to cope with your child's
disability.
• Social worker. A social worker may be involved in assisting your family
with finding services and planning for transitions in care.
• Special education teacher. A special education teacher addresses
learning disabilities, determines educational needs and identifies
appropriate educational resources.
MEDICATIONS
• Medications that can lessen the tightness of muscles may be used to
improve functional abilities, treat pain and manage complications related
to spasticity or other cerebral palsy symptoms.
• It's important to talk about the risk of drug treatments with the doctor and
discuss whether medical treatment is appropriate for the child's needs. The
selection of medications depends on whether the problem affects only
certain muscles (isolated) or the whole body (generalized).
• Drug treatments may include the following:
• Isolated spasticity. When spasticity is isolated to one muscle group,
your doctor may recommend injections of onabotulinumtoxinA (Botox)
directly into the muscle, nerve or both. Botox injections may help to
improve drooling. Your child will need injections about every three
months.
Side effects may include pain, bruising or severe weakness. Other more-
serious side effects include difficulty breathing and swallowing.
• Generalized spasticity. If the whole body is affected, oral muscle
relaxants may relax stiff, contracted muscles. These drugs include
diazepam (Valium), dantrolene (Dantrium) and baclofen (Gablofen).
There is some risk of dependency with diazepam, so it's not
recommended for long-term use. Its side effects include drowsiness,
weakness and drooling.
Side effects of dantrolene include sleepiness, nausea and or diarrhea.
Side effects of baclofen include sleepiness, confusion and nausea.
Baclofen may also be pumped directly into the spinal cord with a tube.
The pump is surgically implanted under the skin of the abdomen.
• The child also may be prescribed medications to reduce drooling such as
trihexyphenidyl, scopolamine (Scopace) or glycopyrrolate (Robinul, Robinul
Forte) may be helpful.
THERAPIES
• A variety of nondrug therapies can help a person with cerebral palsy to
enhance functional abilities. These include the following:
• Physical therapy. Muscle training and exercises may help your child's
strength, flexibility, balance, motor development and mobility. You will
also learn how to safely care for your child's everyday needs at home,
such as bathing and feeding your child.
Braces or splints may be recommended for your child. Some of these
supports are used to help with function, such as improved walking.
Others may stretch stiff muscles to help prevent rigid muscles
(contractures).
• Occupational therapy. Using alternative strategies and adaptive
equipment, occupational therapists work to promote your child's
independent participation in daily activities and routines in the home,
the school and the community.
Adaptive equipment may include walkers, quadrupedal canes, seating
systems or electric wheelchairs.
• Speech and language therapy. Speech-language pathologists can help
improve your child's ability to speak clearly or to communicate using
sign language.
Speech-language pathologists can also teach your child to use
communication devices, such as a computer and voice synthesizer, if
communication is difficult.
Another communication device may be a board covered with pictures
of items and activities your child may see in daily life. Sentences can be
constructed by pointing to the pictures.
Speech therapists may also address difficulties with muscles used in
eating and swallowing.
• Recreational therapy. Some children may benefit from recreational
therapies, such as therapeutic horseback riding. This type of therapy
can help improve your child's motor skills, speech and emotional well-
being.
SURGICAL OR OTHER PROCEDURES
• Surgery may be needed to lessen muscle tightness or correct bone
abnormalities caused by spasticity. These treatments include:
• Orthopedic surgery. Children with severe contractures or
deformities may need surgery on bones or joints to place their
arms, hips or legs in their correct positions.
Surgical procedures can also lengthen muscles and tendons that
are proportionally too short because of severe contractures. These
corrections can lessen pain and improve mobility. These
procedures may also make it easier to use a walker, braces or
crutches.
• Severing nerves. In some severe cases, when other treatments
haven't helped, surgeons may cut the nerves serving the spastic
muscles in a procedure called selective dorsal rhizotomy. This
relaxes the muscle and reduces pain, but can also cause
numbness.
INTUSSUSCEPTION
S-ar putea să vă placă și
- Shoe Dog: A Memoir by the Creator of NikeDe la EverandShoe Dog: A Memoir by the Creator of NikeEvaluare: 4.5 din 5 stele4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDe la EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeEvaluare: 4 din 5 stele4/5 (5794)
- Assessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale Evaluation Short Term Goal Independent: Short Term GoalDocument5 paginiAssessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale Evaluation Short Term Goal Independent: Short Term GoalJobelle AcenaÎncă nu există evaluări
- Case StudyDocument10 paginiCase StudyJobelle AcenaÎncă nu există evaluări
- Geriatric Case StudyDocument15 paginiGeriatric Case StudyJobelle AcenaÎncă nu există evaluări
- Pediatric Case StudyDocument21 paginiPediatric Case StudyJobelle AcenaÎncă nu există evaluări
- Date/Schedule Activities Expected Output Verified/Checked by Area in ChargeDocument2 paginiDate/Schedule Activities Expected Output Verified/Checked by Area in ChargeJobelle AcenaÎncă nu există evaluări
- Assessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationDocument10 paginiAssessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationJobelle Acena100% (2)
- Union Christian College School of Health and Sciences City of San Fernando La UnionDocument11 paginiUnion Christian College School of Health and Sciences City of San Fernando La UnionJobelle AcenaÎncă nu există evaluări
- ER Protocols in The PhilippinesDocument9 paginiER Protocols in The PhilippinesJobelle Acena100% (1)
- NCM 107 Leadership and Management RLEDocument4 paginiNCM 107 Leadership and Management RLEJobelle AcenaÎncă nu există evaluări
- DRUG STUDY (Lung Cancer)Document10 paginiDRUG STUDY (Lung Cancer)Jobelle AcenaÎncă nu există evaluări
- Case Study (Lung Cancer)Document17 paginiCase Study (Lung Cancer)Jobelle Acena100% (1)
- Subjective: Ventilation AssistanceDocument3 paginiSubjective: Ventilation AssistanceJobelle Acena100% (2)
- NCPsDocument11 paginiNCPsJobelle AcenaÎncă nu există evaluări
- Online LectureDocument9 paginiOnline LectureJobelle AcenaÎncă nu există evaluări
- Er Drugs StudyDocument80 paginiEr Drugs StudyJobelle AcenaÎncă nu există evaluări
- PHARMAfdDocument7 paginiPHARMAfdJobelle AcenaÎncă nu există evaluări
- Psychiatric Nursing Michael Jimenez, PENTAGON Slovin'S Formula: N 1 + NeDocument10 paginiPsychiatric Nursing Michael Jimenez, PENTAGON Slovin'S Formula: N 1 + NeJobelle AcenaÎncă nu există evaluări
- Nursing: Core Values of NursingDocument14 paginiNursing: Core Values of NursingJobelle AcenaÎncă nu există evaluări
- DRUG STUDY (Appendicitis)Document14 paginiDRUG STUDY (Appendicitis)Jobelle AcenaÎncă nu există evaluări
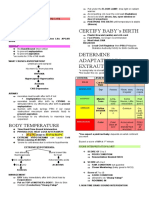
- Certify Baby'S Birth: Body TemperatureDocument9 paginiCertify Baby'S Birth: Body TemperatureJobelle Acena100% (1)
- Case Study On Pulmonary EmbolismDocument12 paginiCase Study On Pulmonary EmbolismJobelle Acena100% (2)
- DRUG STUDY (Preeclampsia)Document11 paginiDRUG STUDY (Preeclampsia)Jobelle AcenaÎncă nu există evaluări
- Drug Study (Pe)Document15 paginiDrug Study (Pe)Jobelle AcenaÎncă nu există evaluări
- Notes On Obstetrics: Normal Labor (Theories of Labor Onset)Document22 paginiNotes On Obstetrics: Normal Labor (Theories of Labor Onset)Jobelle Acena100% (1)
- Assessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationDocument10 paginiAssessment Nursing Diagnosis Inference Objectives Nursing Intervention Rationale EvaluationJobelle AcenaÎncă nu există evaluări
- Case Study (Preeclampsia)Document6 paginiCase Study (Preeclampsia)Jobelle AcenaÎncă nu există evaluări
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDe la EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceEvaluare: 4 din 5 stele4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)De la EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Evaluare: 4 din 5 stele4/5 (98)
- Grit: The Power of Passion and PerseveranceDe la EverandGrit: The Power of Passion and PerseveranceEvaluare: 4 din 5 stele4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDe la EverandThe Little Book of Hygge: Danish Secrets to Happy LivingEvaluare: 3.5 din 5 stele3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDe la EverandThe Emperor of All Maladies: A Biography of CancerEvaluare: 4.5 din 5 stele4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDe la EverandNever Split the Difference: Negotiating As If Your Life Depended On ItEvaluare: 4.5 din 5 stele4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDe la EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyEvaluare: 3.5 din 5 stele3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDe la EverandOn Fire: The (Burning) Case for a Green New DealEvaluare: 4 din 5 stele4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDe la EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureEvaluare: 4.5 din 5 stele4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDe la EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryEvaluare: 3.5 din 5 stele3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDe la EverandTeam of Rivals: The Political Genius of Abraham LincolnEvaluare: 4.5 din 5 stele4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDe la EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaEvaluare: 4.5 din 5 stele4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDe la EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersEvaluare: 4.5 din 5 stele4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDe la EverandThe Unwinding: An Inner History of the New AmericaEvaluare: 4 din 5 stele4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDe la EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreEvaluare: 4 din 5 stele4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)De la EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Evaluare: 4.5 din 5 stele4.5/5 (121)
- Her Body and Other Parties: StoriesDe la EverandHer Body and Other Parties: StoriesEvaluare: 4 din 5 stele4/5 (821)
- 9700 s15 Ms 23 PDFDocument7 pagini9700 s15 Ms 23 PDFRuthÎncă nu există evaluări
- Jackie Virology AssignmentDocument6 paginiJackie Virology AssignmentDumisani NguniÎncă nu există evaluări
- Molecular Basis of InheritanceDocument8 paginiMolecular Basis of InheritancePriyanshu ShivamÎncă nu există evaluări
- CV Prof. Dr. Drh. I Gusti Ngurah Kade MahardikaDocument6 paginiCV Prof. Dr. Drh. I Gusti Ngurah Kade MahardikaM. Arfan LesmanaÎncă nu există evaluări
- Em100 Connect - Clsi m100 Ed31 - 2021Document13 paginiEm100 Connect - Clsi m100 Ed31 - 2021Mdu MakhosiniÎncă nu există evaluări
- Vinca Alkaloids: Maryam Moudi, Rusea Go, Christina Yong Seok YienDocument5 paginiVinca Alkaloids: Maryam Moudi, Rusea Go, Christina Yong Seok YienRIFKI ALIYUSIDIKÎncă nu există evaluări
- Types of Immunity & VaccinationDocument11 paginiTypes of Immunity & VaccinationMuhammad Saad Tariq100% (2)
- Chapter 8Document53 paginiChapter 8contactrafiakhuramÎncă nu există evaluări
- Platelet Rich Plasma For Bone Healing and RegenerationDocument21 paginiPlatelet Rich Plasma For Bone Healing and RegenerationAnonymous Yr9JXHYpPAÎncă nu există evaluări
- XI Bio Chapter 02 Biological ClassificationDocument13 paginiXI Bio Chapter 02 Biological ClassificationSanaÎncă nu există evaluări
- Erythroplasia of Queyrat - Refractory To Photodynamic TherapyDocument3 paginiErythroplasia of Queyrat - Refractory To Photodynamic TherapyOzheanAMÎncă nu există evaluări
- Ch05 Lecture-Cell Membranes and SignalingDocument95 paginiCh05 Lecture-Cell Membranes and SignalingbearreÎncă nu există evaluări
- New IG SubclassDocument13 paginiNew IG SubclassBrîndușa PetruțescuÎncă nu există evaluări
- Senior Biology 1 Q1 - M6 For PrintingDocument47 paginiSenior Biology 1 Q1 - M6 For PrintingMARIBETH RAMOSÎncă nu există evaluări
- Biology SSC I SolutionDocument11 paginiBiology SSC I SolutionFaisal SamiÎncă nu există evaluări
- Antimicrobial Resistance Surveillance in Ethiopia: Implementation Experiences and Lessons LearnedDocument4 paginiAntimicrobial Resistance Surveillance in Ethiopia: Implementation Experiences and Lessons LearnedRajihaÎncă nu există evaluări
- Updated Antibiotic Chart - 2016 PDFDocument2 paginiUpdated Antibiotic Chart - 2016 PDFmugenzi eric100% (1)
- What Is BacteriaDocument33 paginiWhat Is Bacteriaapi-19862227100% (1)
- B.SC Biotech Syllabus-1Document41 paginiB.SC Biotech Syllabus-1Dr. Maruti K. R SDM Degree College UjireÎncă nu există evaluări
- PharmacologyDocument53 paginiPharmacologyapi-3743565Încă nu există evaluări
- MUST To KNOW in Immunology and SerologyDocument18 paginiMUST To KNOW in Immunology and SerologyRona Salando50% (2)
- Bleeding Disorders and Periodontology: P V & K PDocument13 paginiBleeding Disorders and Periodontology: P V & K PAdyas AdrianaÎncă nu există evaluări
- Hema 2 - Prelim Topic 1-Intro To HemostasisDocument4 paginiHema 2 - Prelim Topic 1-Intro To HemostasisLowenstein JenzenÎncă nu există evaluări
- Sylvia Mader BiotechnologyDocument55 paginiSylvia Mader Biotechnologykevin_ramos007Încă nu există evaluări
- Hepatitis B VaccineDocument4 paginiHepatitis B VaccineShantal AbelloÎncă nu există evaluări
- Escherichia Coli-A Gram-Negative, Facultative Anaerobic, Rod-Shaped, Coliform Bacterium of The GenusDocument2 paginiEscherichia Coli-A Gram-Negative, Facultative Anaerobic, Rod-Shaped, Coliform Bacterium of The GenusKent Justin RizonÎncă nu există evaluări
- Vere Chip TMDocument12 paginiVere Chip TMRubi RubiandaniÎncă nu există evaluări
- Introduction To ParasiteDocument51 paginiIntroduction To Parasiteprabad dunusingheÎncă nu există evaluări
- QUIZ 01 (Answer Key)Document1 paginăQUIZ 01 (Answer Key)Tego Shei Harumi100% (1)
- Reviews: Fracture Healing: Mechanisms and InterventionsDocument10 paginiReviews: Fracture Healing: Mechanisms and InterventionsFatrika DewiÎncă nu există evaluări