Documente Academic
Documente Profesional
Documente Cultură
Management of High Grade Bladder Cancer & Carcinoma in Situ
Încărcat de
SakuntalaPalanki0 evaluări0% au considerat acest document util (0 voturi)
115 vizualizări26 paginiG3pT1 most difficult to manage because of conflicting good and bad prognostic (high grade) features. Established risk factors for progression of superficial bladder cancer are - presence of lamina propria invasion - high grade (grade 3) - carcinoma in situ T1G3 tumors are also at high risk of life-long progression.
Descriere originală:
Titlu original
Bladder Cancer Management
Drepturi de autor
© Attribution Non-Commercial (BY-NC)
Formate disponibile
PPT, PDF, TXT sau citiți online pe Scribd
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentG3pT1 most difficult to manage because of conflicting good and bad prognostic (high grade) features. Established risk factors for progression of superficial bladder cancer are - presence of lamina propria invasion - high grade (grade 3) - carcinoma in situ T1G3 tumors are also at high risk of life-long progression.
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca PPT, PDF, TXT sau citiți online pe Scribd
0 evaluări0% au considerat acest document util (0 voturi)
115 vizualizări26 paginiManagement of High Grade Bladder Cancer & Carcinoma in Situ
Încărcat de
SakuntalaPalankiG3pT1 most difficult to manage because of conflicting good and bad prognostic (high grade) features. Established risk factors for progression of superficial bladder cancer are - presence of lamina propria invasion - high grade (grade 3) - carcinoma in situ T1G3 tumors are also at high risk of life-long progression.
Drepturi de autor:
Attribution Non-Commercial (BY-NC)
Formate disponibile
Descărcați ca PPT, PDF, TXT sau citiți online pe Scribd
Sunteți pe pagina 1din 26
Management of High
Grade Bladder Cancer
& Carcinoma In Situ
Presented by –HARADIKAR VARADARAJ
Instructor – Mr.D.MURPHY
Urology Registrars Teaching session – 10/11/2003
GRADES OF BLADDER CANCER
G1 Well differentiated
G2 moderately differentiated
G3 Poorly differentiated
(Advisable for consistency not to use Grade 4)
G3pT1 most difficult to manage because of conflicting
good prognostic (superficial) and bad prognostic (high
grade) features.
G3pT1 – inconsistency of diagnosis
Without reference Pathology review as many as 30% of
cases may be incorrectly or inconsistently diagnosed.
High-Risk Superficial BC (1)
• Established risk factors for progression of
superficial bladder cancer are
• - presence of lamina propria invasion
• - high grade ( grade 3)
• - carcinoma in situ
• T1G3 disease – 10 times the chance of muscle
invasion & death than with other Ta
• Overall 40% of T1G3 tumors will progress
High-Risk Superficial BC (2)
Ta G3 tumors are also at high risk of life-long
progression, not very different from that of
patients with T1G3 tumors
125 such patients followed for 15 years and
progression observed in 39% and cancer related
death in 26%
Herr et al J Urol 2000; 163:60-2
Prognostic Factors (1)
Neither T category nor Grade significantly influence the
recurrence rate: this rate depends mainly on
1) the number of tumors (single tumor, 51%
recurrence at 5 years; multiple tumors, 91%)
2) the previous recurrence rate or recurrence at
3 months
3) The size of the tumors; those >3 cm carry worse prog.
Oosterlink W. The management of superficial bladder cancer,
BJU Int 2001;87:135-41
Treatment of aggressive SBC
Not Clearly defined and followed
1999 BAUS Cancer Audit showed only a small
minority of patients newly presenting with
CIS or T1 lesion had optimal treatment
* 15% of CIS – receiving BCG therapy
* 58% of T1 lesions being treated TUR alone
Endoscopic Assessment
At initial diagnostic cystoscopy it is necessary to document the foll:
Tumor – Size, Number, Position
Growth pattern ( Papillary or Solid)
Mucosa – Normal, red areas or area of red,
irregular mucosa
Lower tract – The Urethra, The Prostate
Bimanual - Is there mass before resection ?
exam Is there mass after resection ?
Size of mass and mobility
Ensuring Correct diagnosis (1)
Proper TURBT & resection should be complete;
pT1G3 tumor recurring at same site suggests
often resection is incomplete.
Two kinds of error
- foci of T1 cancer are left
- first resection fails to diagnose muscle
invasive cancer ( =/ > T2)
Ensuring Correct diagnosis (2)
48% T1 tumors under-staged if no muscle present in TUR
specimen
14% T1 tumor under-staged if muscle present in specimen
was not involved with tumor
(Herr HW. Urol Oncol 1996; 2:92-5)
Data from patients undergoing cystectomy for “T1” disease
show that
- 30% actually have muscle invasive disease
- 50% initial tumor not completely resected
(Amling CL et al. J Urol 1994; 151: 31-36)
Ensuring Correct diagnosis (3)
THE SECOND RESECTION
second TURBT in all pts with pT1 tumors 10 days and no
later than 2-3 weeks
(to facilitate the choice of cystectomy or conservative tx)
SECOND RESECTION to seek
- foci of T1 tumor not completely resected
- any infiltration of muscularis propria not
recognised previously
Ensuring Correct diagnosis (4)
Random Biopsies often useless & do not contribute to
choice of therapy after TURBT
(EORTC study Eur Urol 1999;35:267-71)
Random Biopsies indicated if there is severe dysplasia
or CIS in adjoining or distant epithelium as these
increase risk of progression
- progression in 8% of T1 tumors with no dysplasia
and in 38% with concomitant mild or severe dysplasia
( Heney et al, Herr et al)
Biospy of Prostatic Urethra
Management (1)
Subject of debate always between those Urologists who
advocate Conservative approach and risk “missing the
boat” AND those with aggresive immediate cystectomy
approach who could be removing far too many bladders
Immediate cystectomy
- treats occult muscle invasive disease
- avoids need for very reg. Bladder surveillance
- may result in 5 year survival in 80% patients
- 2-3% risk of treatment related death
- loss of QOL associated with urinary diversion & impotence
Management (2)
EORTC study (2435 patients from six clinical trials,
median FU 7.8 years)
- intravesical chemotherapy ↓ long-term
recurrence rate but not disease progression
or mortality
(Kurth KH et al . J Urol 1996:156; 1934-41)
Therefore unlikely that TURBT with
intravesical chemotherapy could decrease the
risk of progression of T1G3 SBC
Management (3)
Intravesical BCG immunotherapy reducing
progression & mortality is based on few trials
*10-year progression-free rate was 62% for
TURBT with BCG & 37% for TURBT alone
* Disease specific survival – 75% & 55% resp.
(Herr et all in 1988 & 1995, Silverio et al 1997, Herr & Lamm)
Large retrospective study has shown BCG does not
influence recurrence, progression or survival in T1G3
disease
(Struder et al. J Urol 2000; 163 (suppl.1):151,A672)
Management (4)
AUA Guidelines panel reported …..“ there is no evidence that
any intravesical therapy affects the rate of progression to
muscle invasive disease”
SWOG study 391 patients – 4 year survival was 86% for those
treated with inductive BCG regimen and 92% for those on
maintenance schedule (m.s)
{m.s- 3W @ 3 & 6 months & every 6 months for 3 years}
(Lamm et al. J Urol 2000; 165:1124-1129)
Despite the evidence maintenance schedule of intravesical
BCG is currently the best option that can be advocated for
patients with T1G3 SBC
Management (5)
When to stop conservative treatment of
T1G3 tumors ?
1) When there is systemic or local toxicity
from intravesical therapy
2) When patient is not compliant
3) persistence of tumor despite therapy
4) tumor progression
Management (6)
When interval between initial tumor & recurrence is
>21 months the risk of progression is very low
Risk of progression is highest (100% in 3 years) for
patients with T1G3 on follow-up cystoscopy at
6 months
Such refractory T1 tumors have a 50% chance of
developing into muscle invasive disease within
5 years
(Herr et al)
Management (7)
Radiotherapy has been reported to give good long
term disease control for pT1G3 tumors with
preservation of the bladder BUT NOT in randomised
controlled trials
(Duncan et al. Br J Urol 1986, 58:147)
MRC has a trial running comparing RT to either
TUR alone or to intravesical therapy with BCG or
chemotherapy – until this trial is completed we will
not know if RT has a place in treating pT1G3 disease.
Carcinoma In Situ (1)
CIS of bladder is a serious condition characterised by
malignant change in urothelium without invasion
through basement membrane or papillary growth.
CIS will progress to deeply invasive bladder cancer
unless aggressively and adequately treated
CIS first described by Melicow in 1952 as full
thickness replacement of the urothelium by
cytologically malignant cells
Carcinoma In Situ (2)
Prognosis for patients treated by endoscopic
surgery alone is very poor, with 40-85%
progressing to invasive cancer.
Intravesical BCG therapy has become
mainstay.
Review of 18 studies (718 patients) suggested a
72% response rate to the first course of BCG
(Lamm DL, CIS Urol Clin North Am; 1992 Aug: 19(3) : 499-508 )
Carcinoma In Situ (3)
Aims of intravesical treatment
- to treat residual disease
- to prevent recurrence
- to prevent progression
- to conserve the bladder
- to prolong survival
Little agreement about the following
- who should be treated
- when should treatment start
- how should complications be treated
- how many instillations per course
- how many courses and how often
- does maintainance therapy improve survival
CIS Treatment (1)
Traditional 6-week induction course of weekly BCG
therapy has no scientific or immunological basis and is
traditional.
Two courses is better than one with improved response
rates from 35% to 70%
{SWOG8507, Kavoussi et al, J Urol;139 (5) 1988: 935-40 }
(6+3) 6 weeks then 3 weeks @ 3 & 6 months & every 3
monthly for 3 years (27 instillations) - ? Gold standard
- 82% long term tumor free response
- toxicity more severe, non completion of course
CIS Treatment (2)
What is Reasonable clinical practise in CIS ?
1) Patchy, minimal primary CIS & CIS associated with non
invasive papillary TCC should receive 6 weekly instillation of
BCG & review cystoscopy & biopsies one month later
(CIS lesions can be made to fluoresce by prior treatment with
5-amino levulinic acid. This technique is used for
photodynamic detection of CIS)
2) Evidence of progression at above cystoscopy means change of
treatment strategy needed
Proper to have LOW THRESHOLD for cystectomy.
CIS Treatment (3)
3) Failure of the CIS to clear or absence of CIS on biopsy – indication
for SWOG regimen intravesical BCG
70% will have complete response and 64% of responders
will remain disease free at 5 years
Most recurrences occur during the first 5 years of followup
BCG therapy failure have a 48% risk of developing muscle
invasive cancer
CIS gives rise to poorly diff. invasive cancer –
50% disease related mortality in this group = G3 TCC
Finally regarding pT1G3 & CIS
High risk bladder cancers and need to closely monitored
? Followup schedule
urine cytology (urine tests bladder ca- low sensitivity)
Word “superficial” may encourage false reassurance &
even complacency with check cystoscopy done by
junior staff ….time word “superficial” was dropped
from classification !
Treatment failures must be recognised and conservative
treatment abandoned in good time.
TNM Classification of Bladder tumors
Tis Carcinoma in situ
Tis pu Carcinoma in situ in prostatic urethra
Ta Non invasive papillary carcinoma
T1 Tumor invades subepithelial conn tissue
T2 Tumor invades muscle
T2a – invades sup muscle (inner half)
T2b – invades deep muscle (outer half)
T3 Tumor invades Perivesical tissue
T3a – Microscopically
T3b – Macroscopically (extravesical mass)
T4 Tumor invades any- prostate, uterus, vagina,
pelvic wall, abdominal wall
S-ar putea să vă placă și
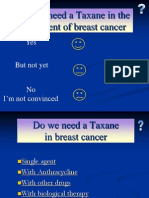
- Taxenes in Breast Cancer (Sharm)Document76 paginiTaxenes in Breast Cancer (Sharm)safasayedÎncă nu există evaluări
- Benign and Malignant Lesion of Lower GIDocument45 paginiBenign and Malignant Lesion of Lower GIAhmad Alzu3beÎncă nu există evaluări
- D105 APBI Future - My Point of ViewDocument70 paginiD105 APBI Future - My Point of ViewSoc. Portuguesa de Radioterapia OncologiaÎncă nu există evaluări
- CARCINOGENESIS CRC Prof RiwantoDocument48 paginiCARCINOGENESIS CRC Prof Riwantoand3sgr3atÎncă nu există evaluări
- Skin Cancer in HKDocument6 paginiSkin Cancer in HKChiu ChunÎncă nu există evaluări
- Japanese Classification of Esophageal CancerDocument25 paginiJapanese Classification of Esophageal CancerppcloverÎncă nu există evaluări
- Gastric Carcinoma: Professor Ravi KantDocument44 paginiGastric Carcinoma: Professor Ravi KantAna Quintana100% (1)
- BIO 2 MergedDocument132 paginiBIO 2 Mergedsubham ghoshÎncă nu există evaluări
- MANAGEMENT OF CARCINOMA CERVIXDocument68 paginiMANAGEMENT OF CARCINOMA CERVIXInsighte Behavioral CareÎncă nu există evaluări
- EARLY CRC (Peran Bedah Dokter Dalam Diagnosis Dini Karsinoma Kolo-Rectal) Prof - Dr.dr. Ing - Riwanto, SPB-KBDDocument31 paginiEARLY CRC (Peran Bedah Dokter Dalam Diagnosis Dini Karsinoma Kolo-Rectal) Prof - Dr.dr. Ing - Riwanto, SPB-KBDHengky TanÎncă nu există evaluări
- Penis Cancer, A Simple Guide To The Condition, Treatment And Related ConditionsDe la EverandPenis Cancer, A Simple Guide To The Condition, Treatment And Related ConditionsÎncă nu există evaluări
- Case Control StudyDocument23 paginiCase Control StudySwapna JaswanthÎncă nu există evaluări
- Hypometabolism: A Clinical Study of 308 Consecutive CasesDe la EverandHypometabolism: A Clinical Study of 308 Consecutive CasesÎncă nu există evaluări
- Mucoepidermoid Carcinomaof The External Auditory Canal (Eac)Document4 paginiMucoepidermoid Carcinomaof The External Auditory Canal (Eac)IJAR JOURNALÎncă nu există evaluări
- Basics of Radiation Therapy: Elaine M. Zeman, Eric C. Schreiber, and Joel E. TepperDocument33 paginiBasics of Radiation Therapy: Elaine M. Zeman, Eric C. Schreiber, and Joel E. TepperCeren AtahanÎncă nu există evaluări
- Radiotherapy in Management of Head and Neck CancerDocument51 paginiRadiotherapy in Management of Head and Neck CancerKassim OboghenaÎncă nu există evaluări
- 3DCRT Dan IMRTDocument57 pagini3DCRT Dan IMRTMisael Christian100% (1)
- Trimodality Therapy in Bladder CancerDocument12 paginiTrimodality Therapy in Bladder CancerStirÎncă nu există evaluări
- Gynecological Brachytherapy GuideDocument8 paginiGynecological Brachytherapy GuideChristy Sitorus100% (1)
- Cancer: Causes and Risks FactorsDocument88 paginiCancer: Causes and Risks FactorsClancy Anne Garcia NavalÎncă nu există evaluări
- Brachytherapy 140129094056 Phpapp02Document77 paginiBrachytherapy 140129094056 Phpapp02KAZOBA FRANCISÎncă nu există evaluări
- Role For Radiation Therapy in MelanomaDocument13 paginiRole For Radiation Therapy in MelanomaHendry HuangÎncă nu există evaluări
- ILRT Dr. Sarbani-1 PDFDocument48 paginiILRT Dr. Sarbani-1 PDFdurgesh kumar100% (1)
- Recent Advances in Radiation Oncology: DR M Spoorthi Shelometh Department of Radiation OncologyDocument53 paginiRecent Advances in Radiation Oncology: DR M Spoorthi Shelometh Department of Radiation Oncologyspoorthi shelomethÎncă nu există evaluări
- Cancer Basics PDFDocument16 paginiCancer Basics PDFPrashant Chari100% (1)
- Radiotherapy in Penile Carcinoma: Dr. Ayush GargDocument32 paginiRadiotherapy in Penile Carcinoma: Dr. Ayush GargMohammad Mahfujur RahmanÎncă nu există evaluări
- Update of Radiotherapy For Skin Cancer: Review ArticlesDocument8 paginiUpdate of Radiotherapy For Skin Cancer: Review ArticlesOscar Frizzi100% (1)
- Adenoid Cystic CarcinomaDocument7 paginiAdenoid Cystic CarcinomalonadiolandaÎncă nu există evaluări
- Faculty of Medicine NR - Ii Department of Surgery NR - Ii: Diseases of The Biliary TractDocument40 paginiFaculty of Medicine NR - Ii Department of Surgery NR - Ii: Diseases of The Biliary TractGalina LozovanuÎncă nu există evaluări
- COLORECTAL CANCER FINAL PPT To Be PresentedDocument53 paginiCOLORECTAL CANCER FINAL PPT To Be Presentedamanuel100% (1)
- Sentinal Lymph Node BiopsyDocument12 paginiSentinal Lymph Node BiopsySahirÎncă nu există evaluări
- Management of Breast CancerDocument53 paginiManagement of Breast CancerGaoudam NatarajanÎncă nu există evaluări
- Thyroid Cancer Types, Diagnosis, TreatmentDocument39 paginiThyroid Cancer Types, Diagnosis, TreatmentFaheem SarwarÎncă nu există evaluări
- Overview of CancerDocument31 paginiOverview of Cancersamarth kaulÎncă nu există evaluări
- Medicine2 - Complications of Cancer Treatment 2007Document76 paginiMedicine2 - Complications of Cancer Treatment 2007api-3762917Încă nu există evaluări
- Ovarian CancerDocument7 paginiOvarian CancerAndi AliÎncă nu există evaluări
- Clinical Presentation, Diagnosis, and Staging of Colorectal Cancer - UpToDate PDFDocument41 paginiClinical Presentation, Diagnosis, and Staging of Colorectal Cancer - UpToDate PDFVali MocanuÎncă nu există evaluări
- Breast Cancer PowerpointDocument13 paginiBreast Cancer PowerpointCara DeaÎncă nu există evaluări
- CancerDocument231 paginiCancerJoshua EsparteroÎncă nu există evaluări
- Molecular Pathology of Breast CancerDocument42 paginiMolecular Pathology of Breast CancerleartaÎncă nu există evaluări
- Breast Cancer in Women - A Narrative Literature ReviewDocument7 paginiBreast Cancer in Women - A Narrative Literature ReviewAnnie McSolsticeÎncă nu există evaluări
- Liquid Biopsy in Urogenital Cancers and its Clinical UtilityDe la EverandLiquid Biopsy in Urogenital Cancers and its Clinical UtilitySeyed Mohammad Kazem AghamirÎncă nu există evaluări
- Folfiri Beva Gi Col PDocument12 paginiFolfiri Beva Gi Col Pvera docÎncă nu există evaluări
- LiverDocument27 paginiLiverAndi Arwan AgusnawanÎncă nu există evaluări
- CT Scan CA ColonDocument31 paginiCT Scan CA ColonNadia IndriÎncă nu există evaluări
- Benign Prostate Hyperplasia: Div. of Urology, Dept. Surgery Medical Faculty, University of Sumatera UtaraDocument56 paginiBenign Prostate Hyperplasia: Div. of Urology, Dept. Surgery Medical Faculty, University of Sumatera UtaraJessica PurbaÎncă nu există evaluări
- Concurrent ChemoRadiotherapyDocument51 paginiConcurrent ChemoRadiotherapyJalal EltabibÎncă nu există evaluări
- Locally Advanced Breast CarcinomaDocument31 paginiLocally Advanced Breast Carcinomaapi-3701915100% (1)
- Glottic Cancer BMJDocument54 paginiGlottic Cancer BMJManling JaoÎncă nu există evaluări
- Systemic Therapies of CRC: Johan KurniandaDocument56 paginiSystemic Therapies of CRC: Johan KurniandaANISA RACHMITA ARIANTI 2020Încă nu există evaluări
- Sarcomas of The Head and Neck: Dr. DarwitoDocument60 paginiSarcomas of The Head and Neck: Dr. DarwitolaurasheerÎncă nu există evaluări
- Cervical Intraepithelial Neoplasia and Cervical CancerDocument28 paginiCervical Intraepithelial Neoplasia and Cervical CancerNatnael100% (1)
- Colorectal CancerDocument39 paginiColorectal CancerFernando AnibanÎncă nu există evaluări
- Diagnosis and Treatment of MelanomaDocument14 paginiDiagnosis and Treatment of MelanomaAnonymous Af24L7Încă nu există evaluări
- Breast Cancer Detection and Treatment GuideDocument35 paginiBreast Cancer Detection and Treatment GuidePrima MedikaÎncă nu există evaluări
- Transposition of The Great Arteries PDFDocument6 paginiTransposition of The Great Arteries PDFSakuntalaPalanki100% (2)
- Preoperative Diagnostic Considerations for Transposition of the Great ArteriesDocument38 paginiPreoperative Diagnostic Considerations for Transposition of the Great ArteriesSakuntalaPalankiÎncă nu există evaluări
- Q. Discuss Gangrene?: OCT/NOV 2010, PAPER 1Document14 paginiQ. Discuss Gangrene?: OCT/NOV 2010, PAPER 1SakuntalaPalanki100% (1)
- Aberrations of Normal Development and Involution (Andi)Document32 paginiAberrations of Normal Development and Involution (Andi)SakuntalaPalankiÎncă nu există evaluări
- UROLOGYDocument222 paginiUROLOGYBeso DavitashviliÎncă nu există evaluări
- Cancer de Cervix 2019pdfDocument6 paginiCancer de Cervix 2019pdfCristian RodríguezÎncă nu există evaluări
- Bladder Cancer 1Document31 paginiBladder Cancer 1Anas HamadÎncă nu există evaluări
- NMIBC Guide: Diagnosis and Management of Non-Muscle Invasive Bladder CancerDocument20 paginiNMIBC Guide: Diagnosis and Management of Non-Muscle Invasive Bladder CancerMade Moniaga PrawiraÎncă nu există evaluări
- Predictive BiosciencesDocument25 paginiPredictive BiosciencesMaxs Christian100% (1)
- Brfo193 Radiotherapy Dose Fractionation Third-Edition PDFDocument137 paginiBrfo193 Radiotherapy Dose Fractionation Third-Edition PDFMed MedÎncă nu există evaluări
- Pathogenesis Bladder CADocument9 paginiPathogenesis Bladder CAHannah LeiÎncă nu există evaluări
- The Epiconus Syndrome Presenting Radicular-Type NeDocument5 paginiThe Epiconus Syndrome Presenting Radicular-Type NeAndjela KosticÎncă nu există evaluări
- Intra Individual Comparison of 18F PSMA1007 and 18F-FDG PETCT in The Evaluation of Patients With Prostate CancerDocument8 paginiIntra Individual Comparison of 18F PSMA1007 and 18F-FDG PETCT in The Evaluation of Patients With Prostate CancerJoaquín Escobar FloresÎncă nu există evaluări
- Chiranjeevi New Package List 2022Document109 paginiChiranjeevi New Package List 2022Shivam MittalÎncă nu există evaluări
- Oncology Drills With Answers and RationalesDocument41 paginiOncology Drills With Answers and RationalesCarol Kayas100% (1)
- Cervical Cancer Staging - TNM and FIGO Classifications For Cervical CancerDocument5 paginiCervical Cancer Staging - TNM and FIGO Classifications For Cervical CancerIrina100% (1)
- Sarkees v. E. I. DuPont de Nemours & Co. - 2020 U.S. DisDocument24 paginiSarkees v. E. I. DuPont de Nemours & Co. - 2020 U.S. DisKirk HartleyÎncă nu există evaluări
- Instilatii BCGDocument3 paginiInstilatii BCGAlina GheÎncă nu există evaluări
- Jco 20 03282Document10 paginiJco 20 03282AKÎncă nu există evaluări
- Orthopedic Surgery Notes: Fractures, Injuries, ProceduresDocument157 paginiOrthopedic Surgery Notes: Fractures, Injuries, Procedureswertfghuji100% (7)
- 3 Urine and Bladder WashingsDocument23 pagini3 Urine and Bladder WashingsnanxtoyahÎncă nu există evaluări
- TURBT Procedure GuideDocument80 paginiTURBT Procedure GuideWindelyn GamaroÎncă nu există evaluări
- Bookshelf NBK305022Document500 paginiBookshelf NBK305022cedricÎncă nu există evaluări
- Congenital Anomalies of Urinary BladderDocument102 paginiCongenital Anomalies of Urinary Bladdernancy voraÎncă nu există evaluări
- Cystic and Solid Tumors of The Urachus vs. Gynecologic Tract Tumors: Similarities and DifferencesDocument15 paginiCystic and Solid Tumors of The Urachus vs. Gynecologic Tract Tumors: Similarities and DifferencesleartaÎncă nu există evaluări
- (2017) Bladder BrachyDocument7 pagini(2017) Bladder BrachyStirÎncă nu există evaluări
- Abstract Book Asmiua 2022Document203 paginiAbstract Book Asmiua 2022Lutfi Aulia RahmanÎncă nu există evaluări
- Non Muscle Invasive Bladder Cancer JUDocument9 paginiNon Muscle Invasive Bladder Cancer JUita maghfirah IlhamjayaÎncă nu există evaluări
- Atypical Extended Immune-Related Neutropenia in Patient Treated With PembrolizumabDocument3 paginiAtypical Extended Immune-Related Neutropenia in Patient Treated With PembrolizumabentannabilakasdyÎncă nu există evaluări
- Oncology NotesDocument6 paginiOncology NotesKSY JanedoeÎncă nu există evaluări
- EAUN15 Guideline Intravesical InstillationDocument90 paginiEAUN15 Guideline Intravesical InstillationRafael RojasÎncă nu există evaluări
- Taj Pharma's FDA-Approved Generic Version, Cisplatin InjectionDocument1 paginăTaj Pharma's FDA-Approved Generic Version, Cisplatin InjectionTAJ PHARMA — A Health Care ProviderÎncă nu există evaluări
- Surgery Sixer For NBEDocument60 paginiSurgery Sixer For NBEamr elfaresy100% (6)
- TURBT - Transurethral Resection of Bladder TumorDocument6 paginiTURBT - Transurethral Resection of Bladder TumorDaywalker PedragozaÎncă nu există evaluări