Documente Academic
Documente Profesional
Documente Cultură
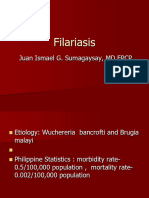
FILARIASIS
Încărcat de
Aries TiongsonDescriere originală:
Drepturi de autor
Formate disponibile
Partajați acest document
Partajați sau inserați document
Vi se pare util acest document?
Este necorespunzător acest conținut?
Raportați acest documentDrepturi de autor:
Formate disponibile
FILARIASIS
Încărcat de
Aries TiongsonDrepturi de autor:
Formate disponibile
FILARIASIS
afflicts Filipino living in the endemic areas chronic, debilitating and disfiguring unnoticed and unfamiliar to health workers 45 out of 78 provinces Accdg to Filariasis Control Unit (FCU)- Regions 5, 8, II and CARAGA Marinduque and Sarangani 0.2-100.8 per 1,000- Sulu highest/ Cebu lowest
Infectious Agents Wuchereria bancrofti. Brugia malayi and/or Brugia timori found in blood Life span of adult parasite- 10 years (but a 40-year-life-span has been reported) microfilariae live for about a year at the most Mode of Transmission Through bites of infected female mosquito Aedes poecilius Bites at night
Incubation Period Variable ranges from 8-16 months Asymptomatic Stage Characterized by the presence of microfilariae in the peripheral blood No clinical signs and symptoms of the disease Some remain asymptomatic for years and in some instances for life Others progress to acute and chronic stages Microfilariae rate increase with age and then levels off In most endemic areas including the Philippines, men have higher micronlariae rate than women
Acute Stage Starts when there are already manifestation such as: Lymphadenitis (inflammation of lymph nodes) Lymphangitis (inflammation of lymph vessels) In some cases, the male genitalia is af fected leading to funiculitis, epidydimitis, or orchitis (redness, painful and tender scrotum)
Chronic Stage Develops 10-15 years from the onset of the first attack. Immigrants from areas where Filariasis is not endemic tend to develop this stage more often and much sooner (1 -2 years) than do the indigenous population of endemic areas.
Chronic Signs and Symptoms Hydrocoele (swelling of the scrotum) Lymphedema (temporary swelling of the upper and lower extremities) Elephantiasis (enlargement and thickening of the skin of the lower and/or upper extremities, scrotum, breast) Diagnosis Physical examination is done in the main health center or during scheduled survey bites in the community History taking Observation of the major and minor signs and symptoms
Laboratory examination Nocturnal Blood Examination (NBE) blood are taken from the patient at the patients residence or in the hospital after 8:00 pm Immunochromatographic Test (ICT) it is the rapid assessment method, it is an antigen test that can be done at daytime. Treatment Treatment of cases in endemic communities Compliance Diethylcarbamazine Citrate (DEC) or Hetrazan
Mass Treatment Distribution to all population Endemic and infected or not infected with filariasis in established endemic areas The dosage is 6 mg/kg body weight taken as a single dose per year Surgical Treatment Chronic manifestation such as elephantiasis and hydrocoele can be handled through surgery. This is usually referred to hospitals for management. Mild cases of lymphedema can be treated by lymphovenous anastomosis distal to the site of the lymphatic destruction. Chyluria is operated on by ligation and stripping of the lymphatics of the pedicle of the af fected kidney while hydrocoeles can be managed by inversion or resection of the tunic vaginalis.
Supportive Care For Filariasis Observe personal hygiene Wash area with soap and water Prevention and Control Measures aimed to control the vector Environmental sanitation such as proper drainage and cleanliness of surroundings Spraying with insecticides (may also produce harmful ef fects)
Measures aimed to protect the individual & Families in endemic areas Use of mosquito nets Use of long sleeves, long pants and socks Application of insect repellants Screening of houses Health education
S-ar putea să vă placă și
- FILIRIASISDocument25 paginiFILIRIASISJoy Gao-ayÎncă nu există evaluări
- FilariasisDocument4 paginiFilariasisapi-371817475% (4)
- FILARIASIS: A Chronic Parasitic InfectionDocument8 paginiFILARIASIS: A Chronic Parasitic InfectionTheeya QuigaoÎncă nu există evaluări
- Catarrhal Stage: 1-2 Weeks Coryza, FeverDocument45 paginiCatarrhal Stage: 1-2 Weeks Coryza, FeverAbigail BrillantesÎncă nu există evaluări
- Filariasis: Bancrofti That Is Released by Infected Mosquitos. It Can Be Performed Any Time of The DayDocument2 paginiFilariasis: Bancrofti That Is Released by Infected Mosquitos. It Can Be Performed Any Time of The Daychristian quiaoitÎncă nu există evaluări
- Filariasis in NepalDocument41 paginiFilariasis in NepalBinaya100% (1)
- Cdnursing PPT 2021Document37 paginiCdnursing PPT 2021yuuki konnoÎncă nu există evaluări
- Communicable Diseases: Roberto M. Salvador Jr. R.N.,M.D. Infectious and Tropical Disease SpecialistDocument846 paginiCommunicable Diseases: Roberto M. Salvador Jr. R.N.,M.D. Infectious and Tropical Disease SpecialistGrn Mynjrkxz100% (1)
- DOH tuberculosis prevention programsDocument9 paginiDOH tuberculosis prevention programsalzysamÎncă nu există evaluări
- COVID-19 Epidemiology and Response: Group IV OCTOBER 24, 2020Document50 paginiCOVID-19 Epidemiology and Response: Group IV OCTOBER 24, 2020Lemlem ArgawÎncă nu există evaluări
- Renal Transplant: 1) Steps Involved in Kidney TransplantationDocument4 paginiRenal Transplant: 1) Steps Involved in Kidney TransplantationNadia SalwaniÎncă nu există evaluări
- Manage Seasonal FluDocument7 paginiManage Seasonal FluAJEET KUMAR PANDEYÎncă nu există evaluări
- Understanding Lymphatic FilariasisDocument5 paginiUnderstanding Lymphatic FilariasisawilakÎncă nu există evaluări
- Feco-orally Transmitted DiseasesDocument133 paginiFeco-orally Transmitted DiseasesTekletsadikÎncă nu există evaluări
- Syphilis "The Great Pretender": By: Bruce MartinDocument28 paginiSyphilis "The Great Pretender": By: Bruce MartinChatie PipitÎncă nu există evaluări
- Case Study of Most Common Communicable DiseasesDocument13 paginiCase Study of Most Common Communicable DiseasesnesjynÎncă nu există evaluări
- Gonorrhoea: Signs, Symptoms, Treatment and PreventionDocument16 paginiGonorrhoea: Signs, Symptoms, Treatment and PreventionBerle Joy VillanuevaÎncă nu există evaluări
- FilariasisDocument11 paginiFilariasishahahahaaaaaaa100% (1)
- Filariasis Control ProgramDocument3 paginiFilariasis Control ProgramCate LagradaÎncă nu există evaluări
- Chapt 19.3 PDFDocument98 paginiChapt 19.3 PDFkasunswiftÎncă nu există evaluări
- Belluomini - Clean Needle TechniqueDocument81 paginiBelluomini - Clean Needle Techniquealbertomtch75% (4)
- Syphilis+in+pregnancy Clinical+Guideline Final Dec14Document10 paginiSyphilis+in+pregnancy Clinical+Guideline Final Dec14Enrique Domingo Pol OrdoñezÎncă nu există evaluări
- Tropmed - Lecture 4Document78 paginiTropmed - Lecture 4VerarisnaÎncă nu există evaluări
- EPIDIMIOLOGYDocument4 paginiEPIDIMIOLOGYMaxamed Ali AadenÎncă nu există evaluări
- HIV InfectionDocument13 paginiHIV Infectionsun shineÎncă nu există evaluări
- Division of Infectious and Tropical Diseases, Department of Internal Medicine, University of Sumatera Utara/ Adam Malik Hospital, Medan, IndonesiaDocument18 paginiDivision of Infectious and Tropical Diseases, Department of Internal Medicine, University of Sumatera Utara/ Adam Malik Hospital, Medan, IndonesiaIndah PutriÎncă nu există evaluări
- Sexually Transmitted DiseasesDocument71 paginiSexually Transmitted DiseasesAkwu AkwuÎncă nu există evaluări
- FilariaDocument65 paginiFilarialunaghilvin2026Încă nu există evaluări
- Scrub Typhus Guideline On Prevention and ControlDocument3 paginiScrub Typhus Guideline On Prevention and ControlVir balÎncă nu există evaluări
- Chlamydia TrachomatisDocument7 paginiChlamydia TrachomatisDewi SetiawatiÎncă nu există evaluări
- DENGUE CONTROL PROGRAM: Prevention, Symptoms, TreatmentDocument23 paginiDENGUE CONTROL PROGRAM: Prevention, Symptoms, TreatmentERMIAS, ZENDY I.Încă nu există evaluări
- Leptospirosissurveillance PDFDocument4 paginiLeptospirosissurveillance PDFHye GoÎncă nu există evaluări
- Scrub Typhus Info and Management Guideline On Prevention and Control 2015 EDCD, WHO DR Vivek DhunganaDocument2 paginiScrub Typhus Info and Management Guideline On Prevention and Control 2015 EDCD, WHO DR Vivek DhunganaVivek DhunganaÎncă nu există evaluări
- Lymphatic Filariasis InfectionDocument48 paginiLymphatic Filariasis InfectionmulatumeleseÎncă nu există evaluări
- Infectious Diseases RlsDocument54 paginiInfectious Diseases RlsA G I T OÎncă nu există evaluări
- Coronavirus: Update On Epidemiology and Clinical ManagementDocument28 paginiCoronavirus: Update On Epidemiology and Clinical ManagementTosin AbiodunÎncă nu există evaluări
- Health Problems MyselfDocument54 paginiHealth Problems MyselfKrishnaveni Murugesh100% (2)
- Renal Transplant: 1) Steps Involved in Kidney TransplantationDocument4 paginiRenal Transplant: 1) Steps Involved in Kidney TransplantationNadia SalwaniÎncă nu există evaluări
- Communicable DiseasesDocument161 paginiCommunicable DiseasesNader Smadi95% (20)
- Typhoid Fever: Doni Priambodo WijisaksonoDocument25 paginiTyphoid Fever: Doni Priambodo WijisaksonoRafif Abdurrahman WijisaksonoÎncă nu există evaluări
- Definition:: Pelvic Inflammatory Disease (Pid)Document20 paginiDefinition:: Pelvic Inflammatory Disease (Pid)Malueth AnguiÎncă nu există evaluări
- Tuberculosis: An Infectious DiseaseDocument39 paginiTuberculosis: An Infectious Diseasecheolyn sealyÎncă nu există evaluări
- DengueDocument45 paginiDengueRachel AlbertÎncă nu există evaluări
- Synonyms Causative Agents Incubatiob Period Mode of Transmission Signs and Symptoms Period of Communicability Diagnostic Test Medical Management Nursing Management ComplicationsDocument13 paginiSynonyms Causative Agents Incubatiob Period Mode of Transmission Signs and Symptoms Period of Communicability Diagnostic Test Medical Management Nursing Management ComplicationsYnah DominiqueÎncă nu există evaluări
- Nosocomial infections and their preventionDocument48 paginiNosocomial infections and their preventionNovita Trilianty MagdalenaÎncă nu există evaluări
- Leptospirosis: Nurul Hidayu - Nashriq Aiman - Audi AdibahDocument28 paginiLeptospirosis: Nurul Hidayu - Nashriq Aiman - Audi AdibahAkshay D'souzaÎncă nu există evaluări
- Lymphatic Filariasis GuideDocument23 paginiLymphatic Filariasis GuidePrincess Gutierrez RositaÎncă nu există evaluări
- Common DiseasesDocument7 paginiCommon DiseasesAlter BadonÎncă nu există evaluări
- Sexually Transmitted Infections and PregnancyDocument19 paginiSexually Transmitted Infections and PregnancyBeyins TiuÎncă nu există evaluări
- 2. Pelvic Inflammatory DiseaseDocument25 pagini2. Pelvic Inflammatory DiseasedeepaÎncă nu există evaluări
- Epidemiology of Lymphatic FilariasisDocument26 paginiEpidemiology of Lymphatic FilariasisvaishnaviÎncă nu există evaluări
- FilariasisDocument76 paginiFilariasisJhey MalanyaonÎncă nu există evaluări
- Yellow Fever: Mosquito-Borne Viral Illness and Vaccine ReviewDocument8 paginiYellow Fever: Mosquito-Borne Viral Illness and Vaccine Reviewprof. Irina SolomonÎncă nu există evaluări
- Emergency MedDocument4 paginiEmergency MedbencleeseÎncă nu există evaluări
- Communicable Disease Lectures 2Document2 paginiCommunicable Disease Lectures 2Sheana TmplÎncă nu există evaluări
- Infections in ICUDocument7 paginiInfections in ICUNikolay ToméÎncă nu există evaluări
- A. Infectious ProcessDocument22 paginiA. Infectious ProcessKyla Malapit GarvidaÎncă nu există evaluări
- SchistosomiasisDocument5 paginiSchistosomiasisBryan TarrobalÎncă nu există evaluări
- Antiretroviral Therapy: Awlachew Firde (S.Pharmacist)Document40 paginiAntiretroviral Therapy: Awlachew Firde (S.Pharmacist)wedajoyonas50Încă nu există evaluări
- DLP HEALTH8 APRIL17 2023 Emerging and Re Emerging DiseasesDocument6 paginiDLP HEALTH8 APRIL17 2023 Emerging and Re Emerging DiseasesAljun MansalapusÎncă nu există evaluări
- Methicillin-Resistant Staphylococcus Aureus (MRSA) in Adults - Treatment of Skin and Soft Tissue Infections - UpToDateDocument22 paginiMethicillin-Resistant Staphylococcus Aureus (MRSA) in Adults - Treatment of Skin and Soft Tissue Infections - UpToDateSiddhartha PalaciosÎncă nu există evaluări
- Literature Review On Nosocomial Infection PDFDocument6 paginiLiterature Review On Nosocomial Infection PDFafmzrvaxhdzxjs100% (1)
- ACTIVITY 4 - Albarico JuanDocument3 paginiACTIVITY 4 - Albarico JuanKynah AmorÎncă nu există evaluări
- Ingrown Toenail: A Small Nail Causing A Big Pain: Healthy ToenailsDocument4 paginiIngrown Toenail: A Small Nail Causing A Big Pain: Healthy ToenailsZoganiteÎncă nu există evaluări
- Swab GuideDocument1 paginăSwab GuideMoe Zaw LinÎncă nu există evaluări
- CPE203 Response 2Document3 paginiCPE203 Response 2Evita Angelina Putri JumaÎncă nu există evaluări
- BloodDocument26 paginiBloodSachidanand ShahÎncă nu există evaluări
- Febrile Antigens Package InsertDocument2 paginiFebrile Antigens Package InsertAhmed AliÎncă nu există evaluări
- Treating UTIs and PneumoniaDocument1 paginăTreating UTIs and PneumoniaNatalia SpencerÎncă nu există evaluări
- Maternal, Fetal, and Neonatal Outcomes in Pregnant Dengue Patients in MexicoDocument8 paginiMaternal, Fetal, and Neonatal Outcomes in Pregnant Dengue Patients in MexicoLola del carmen RojasÎncă nu există evaluări
- Presentation 1Document21 paginiPresentation 1Shekinah Ruth ManupacÎncă nu există evaluări
- Infection Prevention and Control Guidelines For Anesthesia CareDocument35 paginiInfection Prevention and Control Guidelines For Anesthesia CareAlexis MutuyimanaÎncă nu există evaluări
- Centers For Disease Control and Prevention's Sexually Transmitted Diseases Infection GuidelinesDocument6 paginiCenters For Disease Control and Prevention's Sexually Transmitted Diseases Infection GuidelinesabhinavrautÎncă nu există evaluări
- Al-Bayan University Pharmacy College 3 Stage: Metabolism Inhibitors Antibacterial DrugsDocument8 paginiAl-Bayan University Pharmacy College 3 Stage: Metabolism Inhibitors Antibacterial DrugsAhmed HadeerÎncă nu există evaluări
- Nursing Body Parts and Health ProblemsDocument8 paginiNursing Body Parts and Health ProblemsKiki MaharaniÎncă nu există evaluări
- The Vaccine WatchmanDocument46 paginiThe Vaccine WatchmanHan Gi Chase100% (2)
- Foreword: OIE Terrestrial Manual 2008 IIIDocument8 paginiForeword: OIE Terrestrial Manual 2008 IIIWormInchÎncă nu există evaluări
- API 20 E Part IDocument5 paginiAPI 20 E Part IÖzgür ÇanakÎncă nu există evaluări
- CXC Social Studies Sba 2023Document27 paginiCXC Social Studies Sba 2023David DillonÎncă nu există evaluări
- Grammar work sheet questions and passagesDocument6 paginiGrammar work sheet questions and passagesSamyaÎncă nu există evaluări
- Case StudyDocument7 paginiCase StudyLeighvan PapasinÎncă nu există evaluări
- IELTS Discuss Both Views QuestionDocument2 paginiIELTS Discuss Both Views QuestionOngky SetiawanÎncă nu există evaluări
- Anti Mycobacterial DrugsDocument16 paginiAnti Mycobacterial DrugsIqra NaeemÎncă nu există evaluări
- Heavens Medicinal Plants PDFDocument9 paginiHeavens Medicinal Plants PDFۦۦ ۦۦ ۦۦ ۦۦÎncă nu există evaluări
- Medical Nursing I MCQs .Document7 paginiMedical Nursing I MCQs .naa Adel 01Încă nu există evaluări
- Seminar Presentation Plus Ultra 10%Document10 paginiSeminar Presentation Plus Ultra 10%Adaeze Ezem-NjokuÎncă nu există evaluări
- Aflds White Paper: Covid-19: Experimental Vaccine CandidatesDocument35 paginiAflds White Paper: Covid-19: Experimental Vaccine CandidatesfabioÎncă nu există evaluări
- Formulation, Evaluation and Antibacterial Efficiency of Herbal Hand Wash GelDocument6 paginiFormulation, Evaluation and Antibacterial Efficiency of Herbal Hand Wash GelKalpesh PatilÎncă nu există evaluări
- Essay:-''Coronaviruses Are A Family of Viruses Known For Containing Strains That Cause PotentiallyDocument4 paginiEssay:-''Coronaviruses Are A Family of Viruses Known For Containing Strains That Cause PotentiallymuddasirnaddemÎncă nu există evaluări